NEW TECHNOLOGY
A
New Attitude About New Technology
Incorporating
new instrumentation in your practice can lead to improved patient and practice success.

Technology creates proactive eye care. Never has this been truer than in the contact lens field.
Contact lens patients can present to our offices with complex clinical histories. Modern corneal surgical procedures create eyes that have been sliced, cut, burned, tunneled and sutured and still require a contact lens for adequate vision. Many patients present with a history of decades of wearing PMMA and lenses made of low-oxygen-permeable materials. This can result in warped corneas, diseased corneas, dry eyes and irregular corneal surfaces that create complex higher-order aberrations.
Are you prepared to meet the contact lens challenges of the 21st Century? Does your office provide the technology and instrumentation to ensure "patient success"?
Scanning any optometric publication reveals a myriad of instruments that are easy to use, raise the quality of eye care and have hefty prices tags that could profoundly impact your bottom line. Next to satisfying your contact lens patients' needs, a sensible approach to instrument purchasing may be your greatest challenge.
The Basics
Essentially, contact lens fitting instrumentation allows for better time management. You need well-trained staff, a computerized office and a convenient space before incorporating new instruments. Well-trained personnel and practitioners who have a "can-do attitude" go far in making instruments more effective.
|
|
|
|
|
Figure 1. Custom soft contact lens for Post Intacs for Keratoconus. |
Traditional tools may be inadequate for contact lens treatment for keratoconus, pellucid marginal degeneration, corneal transplants, RK, post-LASIK ectasia, corneal dystrophies and severe dry eyes. Fits such as corneal refractive therapy, multifocal contact lenses, toric contact lenses, opaque background tinted designs, semi-sclerals, hybrid lenses, continuous wear and piggyback designs often require more sophistication in patient evaluation.
Raising the Instrument Bar
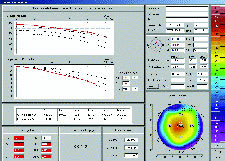
Understanding corneal surface characteristics has always been paramount when designing contact lenses. Corneal topography instruments have evolved to a level where videokeratoscopy, supercharged with high-speed processing and complex software, produces reliable axial, tangential, elevation and refractive maps with built-in nomograms and statistical analysis systems.
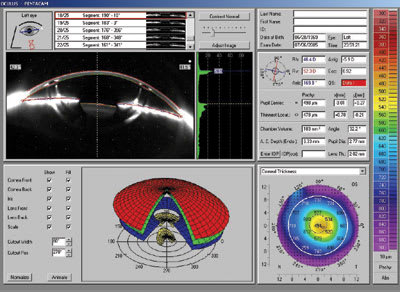
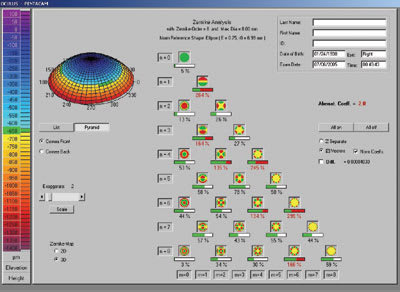
Fluorescein simulation fitting programs, keratoconus detection software and 3-D color mapping are able to send information directly to your contact lens labs via the Internet. New models such as the Oculus Pentacam (Oculus Optikgeräte GmbH) use Scheimflug camera systems that show both anterior and posterior corneal topography, limbal to limbal pachymetry and analysis of Zernike polynomial higher-order aberrations. Other instruments, such as the ReeSeeVit Focus Wave Front topographer (Veatch Ophthalmic Instruments), feature the combined ability of autorefraction, corneal mapping and wavefront aberrometry measurement.
|
|
|
|
Figure 2. Pentacam Keratoconus Indices and Pachymetry. |
|
Wavefront aberrometry will redefine refraction in optometry. Ironically, modern refractive surgery has resurrected contact lenses as the best treatment plan for post-surgical and irregular corneal higher-order aberrations. Auto refraction with measurement of wavefront aberration, point spread and modulation transfer function, and contrast sensitivity will become the future. There are new contact lens designs that incorporate aberration-controlling technology and more are on the way.
With the advent of silicone hydrogel contact lenses, corneal oxygen requirements have become an area of major scrutiny. Clinical specular microscopes such as Konan's Cell Chek, which can photodocument corneal endothelial cell changes and stromal edema, are now available for optometric use. Evaluating the condition of a longtime contact lens wearer's endothelial layer can provide important information to the clinician as to which contact lens material to use. The specular microscope allows clinical evaluation of patients who have compromised endothelial cell function and whom you're refitting into higher-Dk/t materials.
|
|
|
|
Figure 3. Pentacam Higher-Order Aberration. |
|
There are many instances when proper instrumentation is vital to satisfying a patient's lens needs. The following are case examples from our practice.
Case #1
Patient LD was referred to our clinic for blurred vision after bilateral cataract surgery. She was a 76-year-old woman who had worn rigid contact lenses for 45 years and was diagnosed with operable cataracts. It was recommended that she discontinue lens wear two weeks before cataract surgery and IOL implantation. After surgery, her refraction and acuity were OD pl –2.00 x 168 20/50, OS +0.25 –1.75 x 160 20/40 with a +2.50D add. Evaluation with the Oculus Pentacam showed thin central corneas, higher-order aberrations and corneal indices revealing keratoconus, which was previously undiagnosed. (Figures 2 and 3) We successfully fit her with a translating GP bifocal in a high-Dk/t material that corrected her vision to 20/20 distance and near.
|
|

|
|
Figure 4. Specular Microscope photos. Left, refit Night & Day. At right, wearing 30 Dk/t hydrogel. |
|
Case #2
Patient DW entered our office for contact lens treatment of anisometropia. Ocular history revealed a 52-year-old nurse who developed a cataract in her left eye after retinal tear treatment. She previously demonstrated high myopia and had worn low-Dk/t soft hydrogels OU for many years. Post-surgery refraction was OD –10.50 –0.75 x 95 20/20 add +2.00D, OS –0.75 –0.75 x 80 20/30 add +2.50D with regular corneal topography and sim K readings of OD 43.00/42.75 x 96 OS 44.00/43.50 x 97. Specular microscopy of the right cornea showed endothelial polymegethism, pleomorphism, low cell density and stromal edema. We refit her postoperatively with a high-Dk/t Night & Day (CIBA Vision) lens that had an 8.4mm base curve, power of –9.50D and a 13.8mm diameter in the right eye, which corrected her vision to 20/20. She wore no lens in the left eye for intermediate vision. Three months after her right eye was refit, specular microscopy showed improvement in the edema of the right cornea (Figure 4).
Case #3
JK, a 35-year-old male who had keratoconus since age 17, became
intolerant of lens wear in his left eye and opted for an Intacs (Addition Technology,
Inc.) procedure to reduce the prolate nature of the keratoconic cornea. Evaluation
of the left eye six months postoperatively with the Pentacam showed a less prolate
topography, with increased peripheral corneal thickness, less irregular astigmatism,
a Sim K of 46.00/52.00 and refraction of –5.00 –6.00 x 7 to 20/40 VA
(Figure 5). We refit his left eye with a SuperNova Keratoconus design soft lens
(Innovations in Sight) with a base curve of 6.50mm/
8.15mm, power of –7.00D
and 14.4mm diameter, which corrected the vision to 20/30 (Figure 1).
|
|
|
|
|
Figure 5. Pentacam overview Post Intacs for Keratoconus. |
Embrace the Technology
Be proactive in your approach to new technology. Merging the advantages of new diagnostic instrumentation with the multitude of contact lens materials and designs will supercharge your contact lens practice. You'll be able to streamline the fitting of your less complicated contact lens patients and more effectively tackle complex contact lens challenges.
Contact lens practitioners can lead the way to modern vision enhancement by embracing new technology and incorporating it into their lens designs, materials and lens fitting techniques. Watch as your contact lens practice grows with new instruments, a new attitude and satisfied and happy patients.
Dr. Edmonds is in a group contact lens specialty
practice, which he founded, in Tucson, AZ. He is a diplomate of the Cornea and Contact
Lens Section of the AAO, an adjunct assistant clinical professor for the Pacific
University College of Optometry, a past president of the Arizona Optometric Association
and past AZOA OD of the Year.