Quantifying Regression
with Orthokeratology
This
prospective study evaluated how long the effects of myopia reduction persist
over a 16-hour period following overnight corneal reshaping.
By Helen K. Gardiner, OD, FAAO, Michael
A. Leong, OD, FAAO, & Ralph E. Gundel, OD, FAAO
Although researchers have conducted studies of regression associated with orthokeratology in the past, they assessed the regression to the pretreatment levels of myopia following complete cessation of treatment. This type of study was motivated by claims that orthokeratology may permanently reduce myopia after continuous lens wear was discontinued.
More recent studies on regression by Mountford (1998) and Horner et al (1993) assessed short-term regression, but didn't go beyond nine hours following lens removal. The average American gets seven hours of sleep each night (National Sleep Foundation 2001 National Poll), resulting in about 17 waking hours during which a person would require visual correction. Our study takes a closer look at the rate of regression over a longer period of time — approximately 16 hours — to try to more accurately describe what the typical orthokeratology patient may experience as he or she remains uncorrected throughout the waking hours.
This prospective study is designed to evaluate how long the effects of myopia reduction persist once patients remove their lenses over a period of a typical waking day of approximately 16 hours and to quantify the rate of regression throughout this period. We also made a qualitative assessment of patients' experience and satisfaction with Paragon CRT lenses.
|
|
|
|
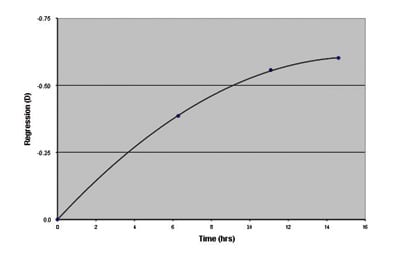
Figure
1. Mean regression (D) vs. time since lens removal. |
|
|
|
|
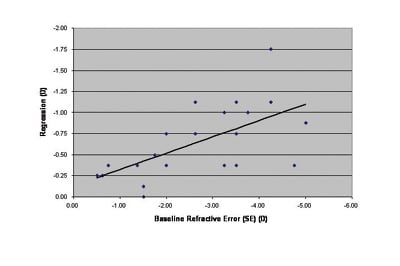
Figure 2. Individual 16-hour regression values (D) vs. baseline degree of myopia (n=22). |
Study Subjects
We enrolled 20 subjects with inclusion criteria of: Age between 18 years and 35 years, myopic distance correction between –0.50D and –6.00D, refractive cylinder no greater than –1.00D at any axis, no near correction, best corrected visual acuity of 20/20 in each eye, no prior GP lens wear, no ocular pathology and no systemic condition that would interfere with GP lens wear.
During the treatment period, we assessed and documented the subjects' eye health, including a thorough evaluation of corneal health, at each visit using slit lamp biomicroscopy. We removed subjects from the study if at any time during the study they demonstrated any of the following signs or symptoms: Persistent decentered treatment zones or any other fits deemed unacceptable according to the Paragon CRT fitting protocols; persistent eye pain, irritation or discomfort; significant or persistent corneal staining (greater than Grade 1); corneal edema; corneal abrasion; keratitis; corneal infiltrates or ulcers; or any other ocular condition requiring the use of therapeutic ophthalmic medications.
Study Procedures
We obtained informed consent from each subject before the interview and initial examination. We recorded a history of what type of corrective lenses subjects used and obtained baseline refractive error and best-uncorrected and corrected Snellen visual acuities. We recorded keratometry readings for use in the fitting process and took baseline corneal topography measurements (EyeMap Corneal Topographer System, version 5.30.16, Alcon Laboratories) for each eye.
For subjects who met the study criteria, we fit Paragon CRT lenses according to the manufacturer's fitting protocols at the same initial visit. (All examiners involved in the fitting process were trained and certified in the fitting and prescribing of Paragon CRT lenses.) The lenses were manufactured in Paragon HDS material (paflufocon B, a fluorosilicone acrylate polymer), having an oxygen permeability (ISO/ANSI Dk) of 100. Using manifest refractive sphere and flat keratometry readings, we selected an initial lens from the fitting set and evaluated fluorescein patterns. If the fluorescein patterns and over-refractions were adequate and acceptable according to the fitting protocols, we instructed the patients about their lens wear schedule and proper lens care using Unique-pH (Alcon) and then dismissed the subjects with the lenses.
After one night of overnight wear (minimum six hours of closed eye wear) we instructed the subjects to return for follow up wearing their lenses in the morning. We then evaluated the lens fit by assessing the fluorescein pattern and corrected visual acuity through the lens. We removed the lenses and performed retinoscopy, manifest refraction, slit-lamp biomicroscopy and corneal topography. If the lens fits were appropriate, then we asked subjects to continue with overnight lens wear and to return in six to seven days for their one-week follow-up visit.
At the one-week visit, we took the same measurements and if lens fit and corneal health was acceptable, we instructed the subjects to continue with overnight lens wear for the next four weeks. Although the wearing schedule for Paragon CRT lenses may vary according to pretreatment refractive errors, (lower myopes may not need continuous overnight wear) we instructed each subject to wear the lenses overnight for a minimum of six hours for the duration of the study.
If we discovered ill-fitting lenses at any of the follow-up visits or if the subjects returned with subjective complaints of blur or fluctuating vision, then we immediately refit those subjects with new lenses, with the appropriate one-day and subsequent one-week follow-up visits.
After four weeks of overnight lens wear, the subjects reported to the clinic for assessment of regression. Following at least six hours of overnight lens wear, we instructed them to remove their lenses and report to the clinic within one to two hours of lens removal for the first baseline measurement. We performed uncorrected and corrected Snellen visual acuity with manifest refraction and slit lamp examination for each eye at this visit. We obtained the same information over the additional three visits, which we scheduled approximately five hours apart for a total review period of approximately 16 hours.
Throughout the course of the study, the subjects cleaned, disinfected and stored their lenses using Unique-pH as recommended by the lens manufacturer.
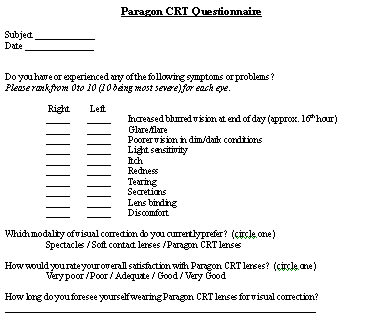
On the final day of assessment, each subject completed a subjective written questionnaire to assess their satisfaction with the treatment using Paragon CRT lenses. For each symptom, the subject rated and scored the severity on a 0- to 10-point scale (0 = best, 10 = worst). We also asked their preferences of visual correction and their overall satisfaction with the performance of Paragon CRT lenses.
Results
Based upon these criteria, data from 11 subjects (22 eyes, four males and seven females, mean age = 25.8 years) were included in our data analysis. We excluded one subject because of a corneal abrasion that resulted midway through the treatment. We excluded an additional eight subjects for the following reasons: Acceptable lens fits not achieved (1), poor quality of vision (1), loss of interest (4) and scheduling conflict (2).
We converted all refractive errors to spherical equivalents. After four weeks of lens wear (range of 35 to 42 days), the patients had worn the lenses overnight for a mean time of 6.55 hours (ranging from 6.00 hours to 7.83 hours) before the day of assessment. After the first measurement at about one to two hours following lens removal, we took subsequent measurements at four intervals (about five hours apart) over an approximate 16-hour period. We plotted the individual amount of regression from baseline (as a function of time since lens removal) for all 22 eyes). After the initial measurement, the mean times of the next three measurements were 6.28 ± 0.63, 11.09 ± 0.68, and 14.61 ± 0.60 hours following lens removal, respectively. The mean regression in diopters from baseline to each of the three mean times of measurements was 0.39D ± 0.35D, 0.56D ± 0.36D, and 0.60D ± 0.48D (Figure 1).
Using the spherical equivalent of each subjects' pretreatment refractive error, we plotted the total end-of-day regression as a function of the presenting level of myopia (Figure 2). The data suggest a direct correlation between the baseline refractive error of each eye and the total amount of regression that occurred by the end of the day.
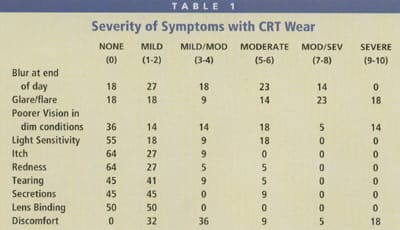
Responses from the questionnaire given at the conclusion of the study showed that the most frequently reported problem was lens discomfort (Table 1). The most severe complaints reported were glare or flare and lens discomfort. Patients also frequently reported minor complaints of itching, redness and tearing.
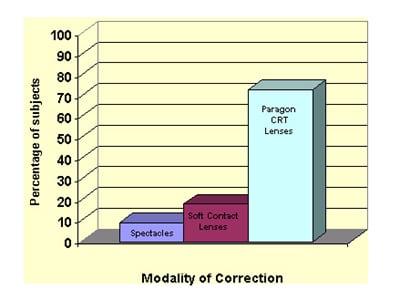
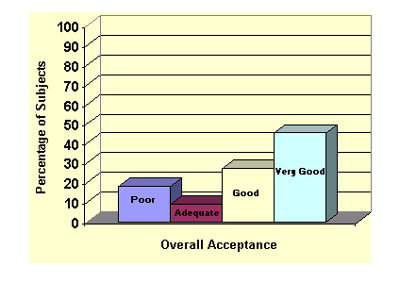
We asked all subjects which vision correction modality they preferred, and 73 percent preferred orthokeratology. At the conclusion of the study, after approximately five weeks of overnight lens wear, nearly half (45.5 percent) of the subjects rated their overall satisfaction with Paragon CRT lenses as "very good," with an additional 27.3 percent rating it as "good."
|
|
|
|
|
|
Discussion
Regression Trend To assess the rate of regression in our subjects, we averaged the intervals at which the regression was measured for all the subjects and then calculated the mean regression of the group for each of the four averaged time intervals (Figure 1). The regression rate as a function of time after lens removal wasn't found to be linear. Instead, the results of this study indicate that most of the regression occurred earlier in the day rather than later in the day. There was 0.39D of regression up until the first interval at 6.28 hours following lens removal, with only an additional 0.21D of regression measured over the next 8.33 hours. Extrapolating from Figure 1, 50 percent (0.301D) of the total regression (0.602D) occurred at approximately 4.6 hours following lens removal.
A previous report by Mountford (1998) found that after 90 days of orthokeratology treatment using OK series lenses (Contex), regression was at the level of 0.50D to 0.75D at eight hours to nine hours following lens removal. He also found that when comparing the regression at seven-day, 30-day and 90-day intervals, the amount of regression appeared to slightly decrease with time, leveling off at about 0.50D to 0.75D after eight hours to nine hours post-wear.
Mountford also found in his experience using reverse geometry lenses that there was an increase in against-the-rule (ATR) astigmatism after lens wear. We found the same trend in our study, where out of a total of 88 separate measurements of regression, 47.8 percent of the measurements were astigmatic errors, with 73.8 percent being ATR astigmatism. While Paragon CRT lenses can correct up to –1.75D of astigmatism, you must take into account the type of astigmatism before initiating orthokeratology. With this in mind, be cautious when considering orthokeratology with patients who reveal ATR astigmatism in pretreatment testing.
Although the bulk of the type of regression was towards corneal steepening, three cases (13.6 percent of total) of corneal flattening occurred after lens removal. Mountford also found evidence of this phenomenon and labeled it "creep," and proposed that the corneal tissue continued to respond to the induced stresses caused by the orthokeratology lens even after the lens was removed. In his study, at the 30-day interval he reported that eight percent of his subjects showed "creep," which is similar to our findings.
|
|
|
|
Subjects� preference for visual correction (n=11) |
|
|
|
|
Subjects� overall subject acceptance of Paragon CRT Lenses (n=11). |
Regression and Baseline Myopia There's an apparent direct correlation between the total amount of regression that occurs throughout a day following lens removal and the degree of myopia at pretreatment (Figure 2). The relationship is linear and directly related such that patients who have more myopia can be expected to experience a greater degree of regression of their myopia, and vice versa for lower myopes. For this reason, practitioners may have more success with orthokeratology if they screen and select their patients carefully. Although the approved range of myopia correctable with Paragon CRT lenses is up to –6.00D, you should lower patients' expectations if their refractive error lies in the upper part of this range. Some orthokeratologists believe that the maximum attempted change should be –4.00D. Based on Munnerlyn's formula, higher amounts of myopia result in smaller treatment zone diameters. This results in an increase in halos, glare, and poor low contrast vision. Therefore make sure that the higher the myopia, the less visually critical the patient is.
A study by Horner et al (1993) on the retention and regression of refractive changes found that increased wearing times of reverse geometry lenses resulted in a slower regression to 95 percent of baseline level of myopia. He wasn't able to demonstrate a correlation between change in initial refractive error and regression. Mountford's study was also unable to find a correlation between refractive change, as measured as change in apical corneal power, and regression. However, results from our study suggest that the degree of regression increases with the degree of myopia at pretreatment.
Subjective Questionnaire Despite the various complaints compiled from the questionnaire, including blur at the end of the day by the 16th hour, the majority of the subjects still preferred to continue to use Paragon CRT lenses as their main mode of visual correction after the study.
Before enrolling in the study, 82 percent of the subjects were soft contact lens wearers, and at the conclusion of the study, only 18 percent of them preferred to continue to wear soft contact lenses. The subjects who preferred soft contact lenses or spectacle correction over Paragon CRT lenses were the ones who reported the most complaints of lens discomfort and glare or flare.
Finally, from the subjective responses at the conclusion of the study, the majority of the subjects were satisfied with orthokeratology using Paragon CRT. As expected, the subjects reporting more visual and ocular symptomologies were the ones who tended to prefer other modalities of visual correction.
|
|
|
|
Appendix A |
|
Conclusion
A certain degree of regression will intrinsically affect all methods and techniques of orthokeratology, and you must consider and account for the amount of regression that will occur before initiating orthokeratology and in selecting and managing patients for the procedure.
Because our findings indicate that the regression associated with Paragon CRT contact lenses occurs most rapidly in the first five hours to six hours after lens removal, obtaining a +0.50D manifest refraction may help "mask" and minimize most of it. This over-correction is important because it compensates for the majority of the regression that occurs by midday and eliminates any significant subjective degradation of vision early in the day, with only a few tenths of a diopter of regression that may adversely affect the patient throughout the late day and early evening. This finding should decrease any concerns about monitoring regression that occurs later in the day.
Our study clearly demonstrates that the higher the degree of baseline myopia, the greater the total end-of-day regression that will occur. Based on our findings, it appears that individuals who present with more than –4.00D of myopia are likely to experience regression of approximately 1.00D, which may limit subjective acceptance because of excessive late-day blurring of vision.
Despite the existence of regression in orthokeratology, if you carefully screen and control the expectations of potential patients in difficult cases, such as those patients who have a greater degree of myopia, the success rate is likely to be quite favorable. Further studies on regression in patients who have used orthokeratology for extended periods would reveal whether regression does indeed decrease after prolonged treatment, which may further enhance patient acceptance.
The authors thank Paragon Vision Sciences, Inc. for supporting this study by providing all necessary Paragon CRT lenses and lens care materials used in this study. The authors have no commercial interest in the orthokeratology lenses used in this study.
To obtain references for this article, please visit http://www.clspectrum.com/references.asp and click on document #119.

|
Dr. Gardiner graduated and completed a Cornea & Contact Lens Fellowship Program at the State University of New York (SUNY) College of Optometry. She currently practices in Los Angeles. |

|
Dr. Leong graduated from UC Berkeley School of Optometry and completed his residency at SUNY College of Optometry specializing in corneal disease and contact lenses. He is currently in private practice in Hawaii. |
| Dr. Gundel is an associate clinical professor and director of the Cornea and Contact Lens Fellowship Program at SUNY State College of Optometry, New York, NY. |