SILICONE HYDROGEL FINDING
A Conjunctival Response to Silicone Hydrogel Lens Wear
A
new finding reveals how silicone hydrogel lenses may affect the conjunctival epithelium.
By Tom Løfstrøm, OD, MScOptom
& Allan Kruse, OD
The introduction of silicone hydrogel lenses has certainly made great strides in improving the physiological response to contact lens wear. Silicone hydrogels also allow wearers the benefit of wearing their lenses for longer periods of time without compromising their eye health.
Objectively, practitioners see the advantages of lenses that provide higher oxygen transmissibility. Clinically, we find a significant decrease in limbal and bulbar conjunctival redness and ghost vessels as well as minimal signs of corneal edema.
However, in spite of their positive qualities, silicone hydrogels are associated with some complications. Researchers have to date focused much attention on the adverse event rate, corneal response and lid response with silicone hydrogels, giving little attention to the conjunctival tissue response. Although it's common to observe conjunctival staining with any type of lens wear, practitioners often aren't too concerned about it because of its minimal clinical significance.
|
|
|
|
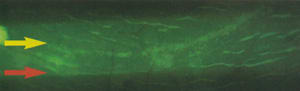
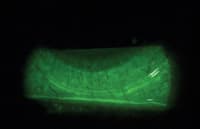
Figure 1. Conjunctival epithelial flap. |
|
|
|
| Figure 2. A conjunctival flap that extends across the entire inferior quadrant. | |

|
|
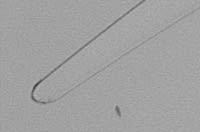
| Figure 3. Conjunctival flaps vary in width among subjects. |
Because silicone hydrogel materials have different properties than do hydrogel lenses and thus may affect the eye differently, we examined silicone hydrogel lens wearers.
Upon close observation of the conjunctival tissue of silicone hydrogel wearers, we noted a new clinical observation that no research has previously reported. We call this new finding a conjunctival epithelial flap.
Discovering a New Finding
We examined 16 subjects who had successfully worn either balafilcon A or lotrafilcon A contact lenses for 30-day continuous wear for a period of at least six months. Of the 16 subjects (32 eyes), seven subjects (14 eyes) wore balafilcon A lenses and nine subjects (18 eyes) wore lotrafilcon A lenses.
We used high magnification, fluorescein dye, a yellow filter and cobalt blue light to observe the conjunctival epithelial flaps. We're surprised that we, and other clinicians, haven't observed the flaps before, but they're difficult to see using white light alone. Slit lamp examination revealed conjunctival flaps in 34 percent of eyes (11/32).
We noted a significant difference in the prevalence of conjunctival flaps between the two lens types (Table 1.) Prevalence with lotrafilcon A was significantly higher compared to balafilcon A (56 percent vs. eight percent, Fisher's test p=0.01).
Clinical Appearance
Figure 1 shows a conjunctival flap located about 1mm beyond the limbus, in the area adjacent to the lens edge. The flap has an uneven margin. Using the eyelid margin, we were able to manipulate the flap and move it around. In this picture, the left part of the flap is facing down whereas the right part of the flap is facing up.
Figure 2 shows a conjunctival flap that spans the entire inferior quadrant. Conjunctival flap appearance can vary significantly between subjects in both the extent (length of the conjunctival flap area) and the width (Figure 3) of the flap tissue.
We observed conjunctival flaps only in the superior, inferior or in both quadrants at the same time, and none in the nasal or temporal areas. The flap may be present by itself or in combination with conjunctival staining and indentation (which may be the early development stage of the flap). We typically observe the flap originating from a slightly raised ridge of what we believe is hyperplastic conjunctival epithelium. We saw no evidence of fluorescein penetration into the conjunctival flap or into the underlying tissue. However, we did observe pooling corresponding to the shape of a pre-detached flap.

Possible Contributing Factors
We have observed the flaps almost exclusively in overnight wear of silicone hydrogels, but we've also seen a few small flaps in daily wear of these lenses.
Clinicians commonly observe contact lens-induced conjunctival staining (CLICS) outside of the limbus, following the lens outline (near the lens edge). This indicates greater lens-tissue interaction and thus may be a factor in flap development.
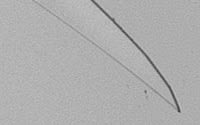
Certain lens edge shapes (Figure 4) may cause more CLICS than others regardless of the lens material. Contact lenses that have a knife-point edge, for example, are known to cause more CLICS than do lenses that have rounded edges.
Silicone hydrogel lens materials have a higher modulus than traditional hydrogel lenses, and non-rounded edge shapes in these lenses may have greater influence in inducing CLICS, indentation and, therefore, conjunctival epithelial flaps. The two silicone hydrogel contact lenses that we studied had similar modulus but different lens edge shapes, and we found that they produced different conjunctival response, particularly in conjunctival flap prevalence.
Based on this pilot study, we conclude that the chisel-shape lens edge design of the lotrafilcon A lens worn on a continuous wear basis resulted in a higher prevalence of conjunctival flaps compared to the round-edge design of the balafilcon A lenses.
Lotrafilcon A lenses are available in two base curves, and Table 1 shows our findings for each. Because of the small sample size for the steep base curve, it's difficult to determine the effect of base curves on conjunctival flap development, although it appears that the steeper base curve may result in a slightly higher prevalence.
|

|
|
|
Figure 4. Contact lens edge shapes: Knifepoint (left), chisel (center) and round. |
||
Discussion
To date, the presence of conjunctival flaps doesn't appear to have a direct impact on lens wearing satisfaction or on subjective comfort. Subjects wearing balafilcon A lenses tended to have less bulbar conjunctival hyperemia compared to those wearing lotrafilcon A lenses.
We are currently considering a few hypotheses for what causes the epithelial flaps. As we discussed previously, most are related to the shape of the lens edge and how it interacts with the conjunctival tissue and how this relates to overnight wear. In particular:
• The lens edge shape configuration may be carving into the superficial conjunctival tissue, facilitated by lens binding during eye closure and subsequent movement upon eye opening. However, the absence of fluorescein penetration and the presence of occasional pooling around this area may indicate that the conjunctival epithelium is splitting or delaminating.
• The lens edge constantly irritates the conjunctival epithelial tissue and consequently increases the conjunctival epithelial cell production or redistributes the epithelial cells. We typically observe what we believe is a raised ridge of hyperplastic conjunctival epithelial tissue. However, we often see flaps (Figure 5, red arrow) outside of the areas with CLICS (yellow arrow). Some lens decentration during eye closure may explain this.
• Conjunctival tissue irritation results in conjunctival chemosis/swelling. When you place a higher-modulus contact lens that has a non-rounded edge on a swollen tissue and a certain pressure is applied (blinking), then the lens edge becomes superficially embedded in the soft swollen conjunctival tissue area and a heaping of cells results. Overnight lens wear under closed-eye conditions and no lens movement may encourage some cells to grow over this area. Upon waking, the lens starts to move with the blink and shreds the emerging tissue.
|
|
|
|
Figure 5. A
conjunctival epithelial flap (red arrow) located outside
of the area with CLICS (yellow arrow). |
|
Questions Remain
Because this observation is new and hasn't been previously reported, further investigation is needed. We believe that manufacturers need to recognize that because of the nature of silicone hydrogel materials, lens fitting, edge shape and parameters are important factors that ultimately determine their clinical performance. Therefore, we believe manufacturers should further consider these factors when designing new silicone hydrogel lenses.
We would like to advise our colleagues to look for the presence of conjunctival epithelial flaps, or "Lens-Induced Flap Excess of conjunctiva" (LIFE), with silicone hydrogel lens wear and to help us understand their etiology and clinical significance.

|
Dr. Løfstrøm is the clinical research operations manager and manager of the Synoptik Contact Lens R & D Clinic in Copenhagen, Denmark. A contact lens specialist, he has also served as a clinical investigator for several international companies and holds several teaching positions. |

|
Dr. Kruse is a research optometrist in Synoptik Research Clinic, Copenhagen, Denmark. |