contact
lens case reports
Fit What's Available Today
BY
PATRICK J. CAROLINE, FAAO, & MARK P. ANDRé, FAAO
|
|
|
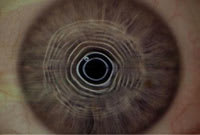
Figure 1. KW's left eye post-RK and hexagonal keratotomies. |
|
| Figure 2. Photokeratoscopy OS, note the distortion of the center five rings. |

|
| Figure 3. Improved keratoscopy image over the soft contact lens. |
Patient KW underwent bilateral radial keratotomy surgery in 1985 to correct his moderate –4.00D OU myopia. After numerous "touchups" and bilateral hexagonal keratotomies, his vision stabilized at OD +7.50 sphere, VA 20/20, and OS +0.75 –2.25 x003, VA 20/60 (Figure 1).
In 2000 KW began wearing a custom daily wear soft lens (+8.50D) OD with good success and a functional VA of 20/25. With his traditional toric soft lens on the left eye, his VA was 20/50 and he complained of significant distortion at distance and near as well as of glare and halos at night. Figure 2 shows the patient's photokeratoscopy OS — note the distortion and uneven spacing between the center five rings.
In March 2002 we fit KW's left eye with a custom toric soft lens in a reverse geometry configuration that had increased center thickness to try to mask some of the irregular astigmatism. The final lens specifications were 9.75mm base curve, 8.6mm midperipheral curve, power of +1.00 –1.75 x180 with a 14.8mm diameter and 0.25mm center thickness. Photokeratoscopy over the anterior surface of the custom toric soft lens revealed a remarkable improvement in the keratoscopy image (Figure 3), which was also reflected in the patient's improved VA of 20/25 and decrease in his subjective symptoms.
KW has continued to wear his soft lenses for 14 to 16 hours each day for the past four years. His unstable cornea OS has necessitated yearly prescription changes and he's currently wearing a lens of power +2.25 –3.50 x165.
Evolve with the Technology
KW was initially referred to the University of Oregon for a corneal transplant OS in the late 1990s. Since that time we've effectively managed him with a series of custom toric soft lenses. We often hear from colleagues that a ballasted, 0.25mm-thick, 59-percent-water HEMA soft lens is sure to induce some cor-neal hypoxia and/or neovascularization. We agree! However, long-term corneal physiology isn't this patient's major problem.
Our philosophy has always been to use the tools we have at our disposal today in the patient's best interest even if the long-term corneal physiology isn't optimal. With the continual evolution in technology and materials in the contact lens industry, we reassure patients that the lenses we fit today most likely aren't what they'll be wearing in two to three years. We're confident that the next time we order lenses for KW, they'll be a higher Dk, latheable, silicone hydrogel material.
Patrick Caroline is an associate
professor of optometry at Pacific University and is an assistant professor of ophthalmology
at the Oregon Health Sciences University. He is also a consultant to Paragon Vision
Sciences and SynergEyes, Inc. Mark André is director of contact lens services
at the Oregon Health Sciences University and serves as an assistant professor of
optometry at Pacific University. He is also a consultant for Alcon Labs, CooperVision
and SynergEyes, Inc.




