SILICONE HYDROGELS
Daily
Wear Experience with Two Silicone Hydrogel Lenses
This
study evaluated the performance of two silicone hydrogel lenses worn for two weeks
of daily wear.
By D. Priya Janakiraman, OD, & Joseph
M. Rappon, OD, MS, FAAO
|
TABLE 1 |
||
| Lens Specifications | ||
| O2OPTIX | ACUVUE ADVANCE | |
| Base curve (mm) | 8.6 | 8.3/8.7 |
| Diameter (mm) | 14.2 | 14.0 |
| Material | lotrafilcon B | galyfilcon A |
| % H2O | 33 | 47 |
| FDA Group | I | I |
| Center thickness at �3.00DS (mm) | 0.08 | 0.07 |
| Dk | 110 | 60 |
| Dk/t at �3.00DS | 138 | 86 |
During their commercial release in 1999, silicone hydrogel lenses were primarily marketed as extended wear lenses. Since then practitioners have also recognized the clinical advantages of prescribing silicone hydrogel lenses on a daily wear basis. Many practitioners began switching their established two-week HEMA disposable lens wearers into silicone hydrogel lenses as well as fitting these lenses on their neophyte wearers. According to a 2006 Health Products Research survey, silicone hydrogel lenses accounted for 40 percent of new soft contact lens fits in the United States during the fourth quarter of 2005, compared to just 17 percent in the first quarter of 2004. This change that is still underway indicates a massive shift in practitioners' dispensing habits and has presumably resulted from advantageous clinical properties of silicone hydrogel lenses.
This article reports the performance of two silicone hydrogel contact lenses, O2Optix (lotrafilcon B, CIBA Vision) and Acuvue Advance with Hydraclear (galyfilcon A, Vistakon), during a two-week period of daily wear usage. Table 1 lists the specifications for the two study lenses.
Methods
An Ethics Committee approved this study and all subjects underwent informed consent in accordance with the Declaration of Helsinki. Researchers carried out a single-center, open label, parallel group, staggered enrollment (non-randomized) study in which we enrolled 92 subjects based on the inclusion/exclusion criteria outlined in Table 2; 43 to wear O2Optix and 49 to wear Acuvue Advance bilaterally. The age, gender, refractive error, corneal curvature and lens wear experience of the subjects was representative of the normal contact lens population and similar between the two study groups.
|
|
|
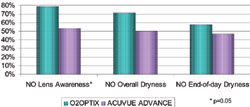
Figure 1. Subjects reporting lens-wear attributes at two weeks. |
Researchers prescribed a daily wear schedule with overnight disinfection using Clear Care (CIBA). All subjects were instructed to rinse the lenses for five seconds through the basket of the lens case with Clear Care and, if significant deposits were present, a rub/rinse step was recommended on lens removal at the clinician's discretion. Patients were required to wear their lenses for a minimum of six hours per day and at least five days per week. We set no restriction on the maximum hours of wear per day or the number of days per week that patients could wear their lenses, but we required that they not sleep in their lenses. Three subjects didn't meet the inclusion criteria and were not dispensed lenses, two in the O2Optix group (astigmatism outside of parameter range; lid papillae) and one in the Acuvue Advance group (viral keratoconjunctivitis). We fit all other subjects with the range of parameters commercially available.
After two weeks of wear, subjects completed questionnaires to rate a variety of subjective variables such as comfort, dryness, vision and handling on a 1 to 10 scale, in which 1 was poor and 10 was excellent. We also sampled satisfaction with the lenses using a five-point scale with choices of "strongly agree," "somewhat agree," "neither agree nor disagree," "somewhat disagree," and "strongly disagree." We asked subjects for the average number of hours that they were able to wear the lenses on a daily basis as well as the average number of hours they felt that the lenses were comfortable to wear on a daily basis.
|
TABLE 2 |
|
Inclusion/Exclusion
Criteria INCLUSION CRITERIA • Signed subject informed consent EXCLUSION CRITERIA • Any active corneal infection |
Other measurements included contact lens surface assessment and corneal physiology, recorded using a 0 to 4 scale in which 0 indicated a score of "none" and 4 indicated a score of "severe," with descriptors for each variable.
For subjective data we present average subjective ratings, the percentage of subjects that fully or somewhat agreed that they were satisfied to predetermined questions and the average total comfortable wearing time. We present frequency distributions of the clinical grades for the objective results.
We analyzed the subjective ratings data with linear mixed models using restricted maximum likelihood method of estimation. We set overall differences between lens types at 5 percent level of significance and analyzed it using the t-test. We compared the severity of symptoms data using the Fisher's exact test at each visit and set the level of significance also at 5 percent. Physiological, lens and vision variables were analyzed as eye-specific data. The methods and principles of data analysis for these variables were similar to the subjective ratings with a few exceptions: We compared baseline physiological variables between the two lens groups for similarity. We did not consider variables that were significantly different at baseline for further analysis. We also performed visit-specific analysis using mixed models due to correlated eye data within each subject.
Subjective Results
Eight subjects discontinued lens wear prior to the two-week visit, two wearing O2Optix (both for discomfort) and six wearing Acuvue Advance (one patient couldn't adapt to lens wear, one had near vision and handling difficulties, one withdrew consent for an unknown reason and three were lost to follow up). Of the 81 subjects who finished the study, we excluded the data from 21 of these subjects in the analysis because the subjects presented for examination at two weeks not wearing the study lenses, wearing the lenses inside out or they presented outside the specified visit window period of 10 days to 19 days from lens dispensing. A total of 60 subjects (28 with O2Optix and 32 with Acuvue Advance) successfully completed the study and were included in the analysis. Table 3 accounts for all subjects.
Comfort O2Optix wearers rated their lenses significantly better than did Acuvue Advance wearers in terms of comfort during the day, lens awareness, dryness (overall and at the end of the day) and burning (Table 4).
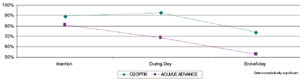
At two weeks, a higher percentage of subjects wearing Acuvue Advance lenses reported dissatisfaction with lens awareness compared to those wearing O2Optix lenses (p=0.05). A trend also occurred for a higher percentage of subjects wearing O2Optix lenses to agree that they were satisfied with comfort (p<0.10). Although not statistically different, more than 20 percent more subjects wearing O2Optix lenses than those wearing Acuvue Advance agreed that the lenses didn't make their eyes feel dry overall (Figure 1). Comfort tended to decline less throughout the day with O2Optix lenses than with Acuvue Advance lenses (Figure 2).
| TABLE 3 | ||
|
Subject Accounting |
||
| O2OPTIX | ACUVUE ADVANCE | |
| Enrolled | 43 | 49 |
| Enrolled, not dispensed | 2 | 1 |
| Discontinued | 2 | 6 |
| Missed or not evaluable | 11 | 10 |
| Successfully completed | 28 | 32 |
The average number of hours of total and comfortable wear time was 1.4 and 1.7 hours greater for O2Optix wearers and Acuvue Advance wearers respectively (p<0.10), with 68 percent of O2Optix wearers reporting a comfortable wearing time of nine hours or more compared to 47 percent of Acuvue Advance wearers (p=0.12).
Other Subjective Results O2Optix wearers also rated subjective eye redness better (less redness) than did Acuvue Advance wearers (9.1 ±1.3 vs. 7.9 ±2.9, p<0.05). Subjective ratings and satisfaction ratings for vision and handling were not different between the two lens types.
Other Results
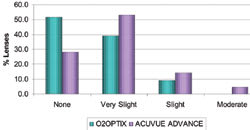
Lens Surface O2Optix lenses attracted less front surface deposits compared to Acuvue Advance lenses (p<0.05). The percentage of lenses with these deposits for each grade appears in Figure 3 for both study lenses.
|
|
|
Figure 2. Subjects reporting good comfort throughout the day at two weeks. |
At two weeks, four (6.3 percent) Acuvue Advance lenses accumulated raised linear front surface deposits. None of the O2Optix lenses developed such deposits.
At dispensing, eight (7.4 percent) Acuvue Advance contact lenses had star-shaped fractures (Figure 4). We didn't observe these fractures with any O2Optix lenses.
Physiological Response and Visual Acuity We observed less corneal staining in O2Optix wearers compared to Acuvue Advance wearers (p<0.05), and there was a trend for less conjunctival staining with O2Optix lenses (p<0.10). We found no differences in objective redness measurements (Table 5). The lenses performed equally well for both high and low contrast visual acuity.
|
|
|
Figure 3. Front surface deposits at two weeks. |
Discussion
The prime reason for discontinuation of contact lens wear is discomfort, particularly dryness-related discomfort. In addition, many patients may decrease their wearing time during the day because of discomfort and thus have a lower expectation of contact lens performance.
Corneal physiology and long-term eye health are paramount particularly with respect to busy lifestyles and the desire to wear contact lenses for longer periods during the day. Maintaining and improving comfort and vision are also key motivators in the contact lens industry. We believe O2Optix lenses address all of these issues.
A compromise of the corneal epithelium may place contact lens wearers at a higher risk for complications such as bacterial, viral or fungal infections. Although typical for contact lens wearers, both lenses in this study caused a low degree of corneal and conjunctival staining, but staining did tend to be higher with Acuvue Advance lenses.
| TABLE 4 | |||
| Subjective Ratings* | |||
O2OPTIX |
ACUVUE ADVANCE |
P |
|
| Comfort during the day | 8.6 ± 1.2 |
7.8 ± 2.2 |
0.05 |
| Lens Awareness | 8.7 ± 1.1 |
7.1 ± 2.9 |
0.01 |
| Overall Dryness | 8.5 ± 1.1 |
6.9 ± 2.6 |
<0.01 |
| Dryness at the end of the day | 7.9 ± 1.8 |
6.3 ± 2.9 |
0.01 |
| Burning | 9.3 ± 1.0 |
8.0 ± 2.9 |
0.03 |
| * Subjective Rating (1 to 10) (1 = "poor," 10 = "excellent") | |||
Schnider and Steffan (2004) cited better vision, comfort and overall satisfaction with Acuvue Advance lenses compared to O2Optix lenses, but presented results after one week of wear despite having a two-week wearing period for the study. The recommended replacement schedule for both Acuvue Advance and O2Optix is two weeks. Our study, which we believe is more indicative of real world conditions, shows the impact of the full two-week wearing schedule.
A
Note about Oxygen Transmissibility An average of 9 percent of daily disposable
subjects in clinical studies sleep in their lenses, and the industry estimates that
84 percent of patients nap in their lenses. We also know that corneal oxygen requirements
vary among individuals. O2Optix lenses provide additional oxygen transmissibility
(62 percent higher) than Acuvue Advance lenses, which may be beneficial for many
patients including those who have higher oxygen requirements, patients who occasionally
sleep in their lenses, those who have higher prescriptions and those under some
environmental conditions such as higher altitudes. This is vital not only for the
thicker plus and toric lenses, but also for higher myopic lenses where peripheral
lens thickness can be significant.
Figure
4. Example of star-shaped fractures on Acuvue Advance lens (magnified 50X).

Papas (1998) indicated that even for daily wear, a recommended Dk/t level of 125 is required to minimize limbal redness. Papas reported that the 95 percent confidence intervals around that value are from 56 to 274, and recommends that at a minimum, lenses should provide a Dk/t of at least 56 at the lens periphery. Having a central Dk/t of 86 and a peripheral lens thickness of 240μm, Acuvue Advance has a Dk/t of 25 in the periphery for a –3.00D lens. However, O2Optix has a central Dk/t of 138 and a peripheral lens thickness of 150μm, which creates a peripheral Dk/t of 73 for a –3.00D lens. This may explain why O2Optix wearers felt they had whiter eyes and wore their lenses longer than did the Acuvue Advance group. Although we found no difference between the lenses in terms of objective limbal and bulbar redness, increased redness with Acuvue Advance as compared to O2Optix may have been evident had we examined the patients at the end of the day. In addition, this study was only two weeks in duration. Possible long-term differences would need further evaluation.
It's also important to note that Papas' work recommending these minimum peripheral levels has been cited as very important to the long-term growth and repair functions of the eye. Being the only source of new corneal epithelial cells, hypoxic stress on the limbal stem cells, which are covered by the peripheral portion of a soft contact lens, may have serious long-term corneal health implications.
| TABLE 5 | |||
| Physiology (0 to 4) | |||
O2OPTIX |
ACUVUE ADVANCE |
P |
|
| Corneal staining | 0.5 ± 0.5 |
0.9 ± 0.6 |
0.01 |
| Conjunctival Staining | 1.1 ± 0.5 |
1.3 ± 0.5 |
0.09 |
| Bulbar redness | 0.9 ± 0.6 |
0.8 ± 0.6 |
0.75 |
| Limbal redness | 0.7 ± 0.6 |
0.8 ± 0.7 |
0.75 |
Deposits While protein deposition on silicone hydrogels is known to be low, studies have noted increased lipid spoilation compared to conventional hydrogel materials. The prominent, raised shiny deposits we found on some Acuvue Advance lenses in this study appeared to be lipid in nature.
Higher deposit levels on soft contact lenses are connected with poorer comfort performance, impacting lens awareness, disrupting wettability and potentially leading to increased dryness and decreased wearing time. Deposits may also cause a mechanical irritation of the palpebral conjunctiva, and lens surface defects have been shown to harbor microbes.
Conclusion
Our results indicate that O2Optix lenses outperformed Acuvue Advance lenses in terms of comfort, dryness, lens awareness, subjective redness, deposit resistance and corneal staining over two weeks of daily wear. Both lenses performed well in terms of vision and handling. We feel that the performance of O2Optix lenses combined with its high Dk/t positions it as an outstanding lens for both daily and occasional overnight wear (up to six nights).
For references, please visit www.clspectrum.com/references.asp and click on document #133.
Dr. Janakiraman is a Senior Principal Scientist at CIBA Vision Research and Development division. She holds a Doctor of Optometry degree from New England College of Optometry and completed a clinical fellowship at the prestigious L.V. Prasad Eye Institute in India. Currently, her main area if interest is to study comfort and visual responses to various silicone hydrogel lenses.
Dr. Rappon is the manager of medical marketing for CIBA Vision, North America. He is a member of the American Optometric Association and is the co-chair of the Georgia Optometric Association's CE committee. He was also named Georgia's Young OD of the Year for 2005.