INSTRUMENTATION
Instrumentation
for Eyecare Practice
Upgrading
your instruments can benefit both your patients and your bottom line.
By Clint Cappelle
Modern practitioners face many challenges on a daily basis, some that originate from outside of the practice and some from within. In my years of visiting many optometric practices around the country, I've observed and learned from some very talented clinicians and gifted business owners.
I've also learned and personally observed what is not usually successful in eyecare practice. How you manage these daily external and internal challenges is usually visible the instant patients walk in your door, and it will continue to leave an impression on them throughout their visit.
|
|
|
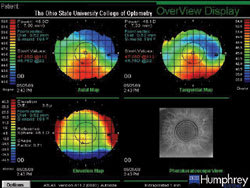
Figure 1. Corneal topography image of keratoconus. |
Build Value into Your Practice
You can be the most gifted clinician around, but that won't necessarily get patients in the door and keep them coming back. The most successful practitioners I know are very talented at building value into every aspect of their practice.
Diagnostic equipment is one tool you can use to build value into the examination you perform on your patients. I'll describe some of the clinical and financial benefits that diagnostic equipment can provide for you and your patients.
Screening Fields
They come in many forms, but perimeters are a must for all practices. Clinically, a perimeter is an extremely valuable tool for your practice. The question you should ask yourself is: Am I using my perimeter to its fullest potential?
Following are my recommendations for your practice. You need a good screening perimeter, and it needs to be fast and accurate — no more than two minutes per eye in screening mode, with excellent sensitivity and specificity values. (Ask company representatives to show you that information.) I highly recommend that you present every new patient and every established patient returning for yearly or bi-yearly examination with the option to perform the test. Automated screening peri-metry is beyond what some insurers require for payment. They may require only a confrontation peripheral visual field test and/or amsler grid. Practitioners should consider whether or not they will charge for this service beyond their comprehensive examination or other examination fee. Too many doctors have told me how pleased they are with the success of a screening perimeter in their office for it to not be true. Please remember, it's in your patients' best interest to have the test done, and the first time you find something that you otherwise most likely would have missed, the instrument pays for itself.
Threshold Fields
If you treat glaucoma or aspire to treat it, a good thresholding perimeter is a requirement. You'll need an instrument that is able to perform at least a 30 degree test. Pay close attention to how the instrument gathers the information, and what it does with the data once obtained. You have many options for thresholding perimeters. Projection, StaticLED and Frequency Doubling are the most popular. Each has its own positives and negatives, and you need to determine which will benefit your practice and your patients the most, both today and in the future. Don't make the mistake of filling a temporary gap today only to find that you have a hole in the future. Purchase for where you are today and where you will be in the future.
If you are in the market for a perimeter or are contemplating trading in your old one, ask yourself this question: Am I treating or will I be treating glaucoma? If not, your best option may be a perimeter that isn't full-featured. If you are treating glaucoma or have intentions too, I recommend that you consider a full-featured model. Which one is the best? The one that fits your needs and provides reliable, accurate information. Talk to your peers and to the doctor to whom you refer the most to assist you with your choice.
Auto-refractors
|
|
|
Figure 2. Pseudomonal corneal ulcer image taken with a digital photo slit lamp system. |
Efficiency, efficiency, efficiency — that's the name of the game when choosing an auto-refractor. How do you know if you're a candidate for purchasing one or if you're using your current auto-refractor to its fullest potential? In an ideal situation, I recommend the following approach: First, don't run it yourself. Train someone in your office to run it. Most current auto-refractors are very user friendly and accurate to about ±0.50D, depending on the age and accommodative ability of the patient. If your unit has visual acuity capabilities, train your staff to do this also. Instruct your staff to enter the refraction from the unit into your phoroptor. You can now spend more time attending to patients' needs, rather than gathering information that others can obtain. Efficiently managing your resources will provide the opportunity to spend more quality time with patients while managing more patients per day.
I believe about 25 models of auto-refractors are currently on the market. I recommend a unit with fast acquisition speed, auto-tracking and alignment, pupilometer and visual acuity measurements with subjective refinement. I know that's a lot to ask for in an auto-refractor, but such models do exist and are very useful to maximize your time.
Corneal Topography
Corneal topography may be more difficult to justify for a small practice, but sometimes you need to dig just a little deeper. Clinically, the benefits of topography are fairly straightforward. Keratoconus (Figure 1), pellucid degeneration and even elevated levels of post-surgical astigmatism are all acceptable and billable diagnoses.
Today, billing out and receiving payment for corneal topography is somewhat difficult. You need to bill it out under the 92499 unlisted code and send the proper required documentation. It's my understanding that corneal topography will have its own procedure code beginning in January 2007. This should make the medical billing for topography much easier and help clear up the blurry lines of what is an approved diagnosis code and what is not.
You can't effectively screen and comanage refractive surgery patients without corneal topography, and it's an excellent way to introduce refractive surgery to your patients. The bulk of your patients who are candidates for refractive surgery are your contact lens patients, so it makes sense to perform topography on all of them. There are several schools of thought as to the proper implementation model for corneal topography. One way is to offer it as a fee for value added service and charge a nominal fee for the test. I don't feel this is the best way to promote topography in your practice, especially if you're currently offering screening visual fields in this manner. I suggest you instead perform topography on all of your contact lens patients and increase your contact lens fitting fee. This way you perform it on the patients who will potentially benefit the most from it.
I also recommend printing out an extra copy of the exam report and giving it to the patient to take home. This will add value to the experience your patient has while in your practice and will help improve retention rates because it demonstrates that you have a progressive, hi-tech, advanced practice that provides the highest level of care possible.
If you're contemplating the purchase of a new topographer or trading in your old one, you may find several diagnostic tools that some topographers provide valuable. All topographers can perform axial and tangential maps fairly accurately; what all topographers can't do is elevation mapping, in which the topography software fits a patient's cornea with a best-fit reference sphere and then calculates the patient's corneal elevation to that reference sphere. A common mistake I've observed in practice is when clinicians misinterpret corneal steepness for corneal elevation. If a part of the cornea is steep, that doesn't necessarily mean it's elevated.
The software programs available today will show you corneal elevation based on a reference sphere and corneal irregularity based on a best-fit reference toric. Instead of fitting the cornea with a best-fit sphere, the software will fit the cornea with a best-fit reference toric, a hypothetical best-fit lens for the eye, and it will show you the residual corneal irregularity that spectacles or toric contact lenses can't correct. This could help you determine why your 20/25 or 20/30 patient doesn't have acuity of 20/20. In most cases, a simple axial map would not be able to clarify this for you, unless the condition was very obvious.
|
|
|
Figure 3. Papilledema image taken with a non-mydriatic digital photography system. |
Retinal Imaging
In the past three years, the usage of retinal imaging has grown significantly within eye care. The HRT II (Heidelberg Engineering), GDx VCC (Carl Zeiss Meditec AG) and Stratus OCT (formerly OCT 3, Carl Zeiss Meditec AG) have shown themselves to be the leaders in this area. Although they all use completely different technology to gather the data, the goal of objectively measuring and detecting structural loss to aid in the diagnosis and management of glaucoma and macular changes remains.
The most common question I receive about these devices is not "Should I get one?" but "Which is the best one for my practice?" That's usually a fairly difficult question to answer. All of the technologies have proven to work. Some are more user friendly than others, but the qualities that make them user friendly limit their versatility. Having the instruments demonstrated in your practice will assist you with the decision. Make sure your staff is present during the demonstration and that they use the instrument themselves. Will they be able to perform the testing needed without help from you? Remember, you use the information presented to you by your staff to make clinical choices for your patients. You must have full confidence in the information.
Slit Lamp Photography
Digital photodocumentation is one of the most overlooked and powerful communication tools available for practitioners today. It provides your patients the opportunity to visualize the damage/condition that they are confronting and may encourage greater patient compliance. For example, seeing an image of a corneal ulcer (Figure 2) generated by poor contact lens maintenance will remind a patient to remove and properly clean his lenses. Billing and coding for photodocumentation is well defined, and you should use it as necessary.
Retinal Photography
Retinal photography is another well-established procedure commonly used to verify retinal health or to visually document a specific retinal abnormality. It's very common for practitioners to offer or suggest this procedure for an additional fee. With the evolution of non-mydriatic digital photography systems, retinal photography is very user friendly and cost effective. Figure 1 shows an example of papilledema taken with this system. If you're currently using an old Polaroid system, I suggest considering the addition of a digital portion to your current system or trading in your current system for a new one. The cost of Polaroid film is astronomical, and it's becoming more difficult to find.
Legally, digital posterior pole photography is one of the smartest choices you can make to protect yourself against malpractice accusations. A digital photograph of the eye on a specific examination date is objective evidence of the health of the eye at that time. The value of a simple digital photograph could become priceless one day. Typically, medical billing for optic nerve photographs is yearly for glaucoma suspect patients.
Always Put Your Patients First
I want to emphasize that every point I've discussed in this article has your patients' best interests in mind. For example, I've personally seen the benefits of performing a screening visual field on every patient. It's well worth the effort to find a potentially life-threatening condition that might otherwise go undetected.
It is also in your patients' best interest for you to be efficient. Their time is valuable and, more importantly, the time they spend with you is valuable. The best way to achieve this level of efficiency is through automation. You can't do it all. If you properly build value into your exam, you'll have a more successful business — and clinically, you'll have the data you need to properly manage your patients. Your patients in turn will appreciate your thoroughness and will return year after year.
Mr. Cappelle is the Ocular Disease Service and Imaging Coordinator at the Ohio State University College of Optometry.