SILICONE HYDROGEL BENEFITS
Benefits
of Silicone Hydrogel Lenses
Higher
oxygen levels mean a healthier cornea with fewer contact lens-related complications.
By Desmond Fonn, DipOptom, MOptom, FAAO,
Kathy Dumbleton, MSc, FAAO, Isabelle Jalbert, OD, PhD, FAAO, and Alisa Sivak, BA,
Dip Ed, MA
Contact lenses composed of silicone hydrogel materials were introduced to the European market in 1999 and to the United States in 2001. Initially, their development focused on meeting — even surpassing — the oxygen transmissibility requirements for overnight wear. The superior health benefits of these materials for continuous wear have been thoroughly documented,1–5 and studies confirm similar advantages with daily wear of silicone hydrogels.5–8
Today, the range of available lenses includes five materials, spherical and toric designs, and several wearing modalities: Daily wear, flexible wear and continuous wear. Regardless of wearing modality, the health benefits of these lenses remain the same: Sufficient oxygen means a healthier cornea, free of hypoxic effects and able to combat common contact lens-related complications. In this article, we'll review some of these complications and how silicone hydrogels address them.
|
|
|
Figure 1: Limbal hyperemia at each of the study visits, as subsequently graded by a masked observer on a 0 to 100 scale from digital photographs of the temporal quadrant of 32 subjects. Baseline is the measurement taken when subjects entered the study wearing their habitual low-Dk hydrogel lenses. |
Corneal Edema
The cornea depends on oxygen to maintain its thickness and transparency, and contact lenses reduce the amount of oxygen reaching the cornea, creating a hypoxic environment. Studies also have shown a strong correlation between corneal swelling and oxygen transmissibility.9–11 Corneal swelling with contact lenses is exacerbated when the lenses are worn overnight, with the amount of swelling ranging from 7% to 15% with the wear of low-Dk hydrogel lenses.11–16
Numerous studies have shown that lenses made from silicone hydrogel materials induce significantly less overnight corneal swelling (ranging from 2% to 5%) than traditional low-Dk hydrogel lenses. These values are similar to overnight (closed-eye) corneal swelling without contact lens wear.11,12,17–23 This demonstrates the value of high-Dk silicone hydrogel lenses, which have effectively eliminated hypoxia for most patients.
Ocular Redness
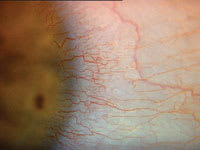
Ocular redness — in particular, limbal redness — is the clinical sign associated with HEMA contact lens wear that patients recognize. It becomes apparent as the limbal blood vessels dilate. While a number of mechanical and physiological factors can contribute to limbal hyperemia, it has been linked directly to the amount of oxygen able to reach the ocular surface and, therefore, the oxygen transmissibility of a contact lens.24 Limbal redness is seen when low-Dk conventional lens materials are worn, even on a daily-wear basis. A rapid increase in redness can be detected as early as 4 hours after lens application.25
Several studies have shown significantly less limbal hyperemia with overnight wear of silicone hydrogel contact lenses, compared with conventional hydrogel lenses.2,3,26–28 This suggests hypoxia plays a major role in its appearance. More recently, studies also have reported less limbal hyperemia in neophytes adapting to daily wear of silicone hydrogel lenses,5 as well as a reduction in hyperemia when adapted HEMA lens wearers were refitted with silicone hydrogel lenses.7
One study7 showed that a group of conventional low-Dk hydrogel lens wearers who were refitted with daily-wear silicone hydrogels experienced a reduction in limbal hyperemia over time (Figure 1). The results of this study showed the reduction was most marked for those subjects who presented with higher baseline levels of limbal hyperemia and occurred very rapidly (Figures 2a and 2b). The subjects also reported a corresponding reduction in end-of-day redness when they wore silicone hydrogel lenses.
Neovascularization
|
|
|
Figure 2a (top): Limbal hyperemia subsequent to long-term conventional hydrogel lens wear. Figure 2b (bottom): Reduction in limbal hyperemia after 2a was refitted with a silicone hydrogel lens. |
Typically, neovascularization in a contact lens wearer presents as a moderate circumlimbal or regional encroachment of 1 mm or less into the cornea from the limbus (Figure 3a). This condition is also associated with hypoxia induced by low-Dk contact lens wear. Although many patients are unaware they have this complication, it's unquestionably in their best interest for practitioners to resolve it.
Until recently, the only solution we could offer patients with neovascularization was to suggest they reduce the hours or days of lens wear, or possibly to refit them with gas permeable lenses. These strategies offer limited success, making the option of a soft lens with significantly higher oxygen transmissibility appealing to patients and practitioners.
Clinicians have observed remarkably rapid emptying of these vessels after refitting long-term low-Dk lens wearers with silicone hydrogel lenses1,28 (Figures 3a and 3b). One month after refitting long-term low-Dk lens wearers with Night & Day lenses worn on a daily-wear basis, patients exhibited apparent shrinking of the vessels in diameter and length (extension of the vessels into the cornea). The vessels do not regress, but rather remain as "ghost vessels."29 However, some stimuli, including mechanical trauma and inflammatory reactions, can cause these vessels to refill.
Changes in Refractive Error
Many soft contact lens wearers demonstrate a slow but progressive increase in myopia known as "myopic creep." Small increases in myopia (< 0.50D) were first reported with daily wear of thick (> 0.1 mm) hydrogel lenses.30-33 Reports continued with thinner hydrogel lens designs, particularly when they were worn on an extended-wear basis.34,35
This myopic shift may be related to chronic corneal hypoxia. It is well established that traditional hydrogel lens materials fail to provide the cornea with enough oxygen to avoid hypoxic consequences, particularly during overnight wear. The resulting corneal edema is thought to induce changes in the corneal curvature and refractive index, which increase the eye's total refractive power.
An early clinical trial of silicone hydrogel lenses at the Centre for Contact Lens Research, University of Waterloo, Waterloo, Ontario, found that extended wear of a silicone hydrogel lens induced little or no change in refractive error compared with extended wear of a low-Dk conventional hydrogel lens.3 The low-Dk conventional hydrogel lens induced an increase in myopia when worn for the same period on a contralateral eye.
A subsequent study comparing low-Dk hydrogel wearers with silicone hydrogel wearers over a 9-month period of extended wear found similar results. The mean spherical refractive error increased in patients wearing the low-Dk lenses but did not change for those wearing silicone hydrogel lenses (Figure 4).27 Spherical refraction in the hydrogel wearers increased to a greater extent in patients with low-baseline myopia, compared with those with moderate-baseline myopia.
Some clinicians have reported
hyperopic shifts in subjects wearing silicone hydrogel lenses. This has been attributed
to either a reduction in previous myopia induced by chronic hypoxia27
or to pressure-
induced changes in corneal shape.36 The latter hypothesis
speculates that the relatively stiff silicone hydrogel materials flatten the central
cornea, leading to an
orthokeratology-like effect. Central corneal flattening
seen during silicone hydrogel wear further supports this idea.27,36 The
precise etiology of these hyperopic shifts isn't clear, but both factors probably
play a role.
|
|
|
Figure 3a (top): Neovascularization subsequent to long-term conventional hydrogel lens wear. Figure 3b (bottom): Regression of the vessel response following refitting of the eye in 3a with a silicone hydrogel lens. |
Practitioners should conduct a careful over-refraction 2 to 4 weeks after fitting patients with silicone hydrogel lenses, particularly patients who previously wore low-Dk lenses. Otherwise, a patient may end up wearing an over-minused or under-plussed lens, which could result in near-vision problems, particularly for a patient who is on the verge of presbyopia.
Epithelial Microcysts
Epithelial microcysts — small, circular, refractile inclusions typically found in the cornea's paracentral zones — usually develop as a result of chronic hypoxia from contact lens wear. They occur more predictably as a result of extended or continuous wear, with the number of microcysts peaking approximately 3 months after extended wear begins. They sometimes occur with daily wear if the lenses have very low oxygen transmissibility. Epithelial microcysts have been described as one of the best clinical indicators of chronic corneal hypoxia.
Studies show the development of microcysts is closely related to corneal swelling37 and, therefore, oxygen transmissibility, with the number of microcysts corresponding to the level of swelling. In a contralateral extended wear study of patients wearing a low-Dk soft lens on one eye and a GP lens (of the same low-Dk value) on the other eye, the frequency of microcysts was significantly greater in the eye wearing the soft lens. The difference is attributed to the increased oxygen as a result of the GP tear exchange during the open-eye phase. In contrast to low-Dk soft lenses, extended wear of silicone hydrogels induces very few epithelial microcysts.3,38
Other Epithelial Effects
Homeostasis is the process through which the eye maintains its natural balance. For the corneal epithelium, this means a complex system in which limbal stem cells give rise to migratory basal epithelial cells that divide and gradually differentiate into wing and surface cells39 (Figure 5). The eye eventually sheds surface cells in the tear film after they die in a natural, preprogrammed fashion called apoptosis.40 Blinking also plays an important role by encouraging the regular "shearing" of loosely attached mature apoptotic surface cells.
We can clinically gauge the state of this
delicate balance between proliferation (Figure 6), differentiation and desquamation
by measuring epithelial thickness, cell-shedding rate, and cell size in vivo. To
do this, we use research tools, such as modified optical pachometry,41
optical coherence tomography,42
confocal microscopy,43
eye washing and irrigation chambers,44-46 and contact lens cytology.47
Clinical trials consistently demonstrate that contact lenses — regardless of
lens type or wearing schedule — disturb this natural process, causing epithelial
thinning, reduced cell shedding and increased cell size.44-46
It's not surprising that the introduction of a contact lens as a barrier between the eyelid and the eye's front surface leads to a reduction in natural cell-shedding, increased cell size and decreased cell proliferation, as does normal eye closure. What's harder to explain is that the retention of bigger cells on the eye's surface for longer periods does not lead to a corresponding increase in epithelial thickness. In fact, the opposite occurs: Researchers consistently observe epithelial thinning, indicating that the lens-wearing effects that lead to thinning override the effects associated with thickening. The pressure exerted by the contact lens modulates these thinning effects. Unfortunately, high-Dk GP lens materials have proven to have the highest thinning impact on the corneal epithelium.44–46
Researchers also have observed decreased cell regularity in the deeper epithelium of long-term extended wearers of low-oxygen transmissibility lenses.41 This is somewhat reminiscent of the endothelial polymegethism changes described in long-term low-Dk lens wearers.48 We now know these changes are reflected at the cellular level by a decrease in the proportion of naturally dead and dying (apoptotic) cells found at the surface of the epithelium,49,50 as well as a reduced proliferation rate of basal epithelial cells.51,52
|
|
|
Figure 4: Mean change in refractive error over time for high-Dk (lotrafilcon A, n=39) and low-Dk (etafilcon A, n=23) wearers. |
A number of these effects appear
to depend on the level of oxygen available to the epithelium and thus are proportional
to the oxygen transmissibility of the contact lens worn. For example, overnight
wear
induces more thinning than daily wear of the same lens and high-Dk silicone
hydrogel lens materials induce less thinning than low-Dk conventional soft HEMA
lenses.44,53,54
The organism most commonly isolated from contact lens-related microbial keratitis cases is Pseudomonas aeruginosa. In-vitro studies have shown these organisms have the propensity to bind to harvested epithelial cells. The level of binding that occurs has been used to measure epithelial health. Studies examining epithelial cells harvested from both rabbits and human subjects whose corneas were exposed to low-Dk and silicone hydrogel contact lenses show that P aeruginosa-binding was significantly lower with silicone hydrogel contact lenses (i.e., high oxygen transmissibility), regardless of wear schedule.44,53,54 This paradigm has been suggested as a surrogate for prospective clinical trials as a means of predicting the risk for contact lens-related microbial keratitis.55
The corneal stroma is largely ignored by contact lens researchers, yet it is responsible for maintaining vital ocular functions, such as transparency, mechanical strength and wound-healing response.56 Recent technological advances, such as in-vivo confocal microscopy, let us see subtle and previously undetected changes associated with contact lens wear, such as a reduction in the number of stromal keratocytes57 and the presence of stromal microdot deposits.58 Again, these changes appear somewhat related to hypoxia and, therefore, the capacity of contact lens material to transmit high levels of oxygen to the stroma.
In essence, contact lens wear seems to "slow down" the eye's natural renewal processes in proportion to the lens material's oxygen transmissibility. This effect can increase susceptibility to harmful bacteria. Although we can't completely eliminate the effects of contact lens wear, we can minimize them by choosing a material that provides the highest possible oxygen transmissibility, such as silicone hydrogel materials.
|
|
|
Figure 5: Epithelial homeostasis. |
Comfort Concerns
Ocular discomfort is a major concern for patients and the entire contact lens industry. In fact, it's the reason most patients discontinue wearing their lenses. The most common symptom of contact lens-related discomfort is dryness, which generally increases over the day. Comfort tends to be lower on awakening with extended wear of both hydrogel and silicone hydrogel lenses, a pattern that may be related to a reduction in tear volume and changes in the chemical composition of tears during sleep.59
Strong anecdotal evidence indicates contact
lenses made from silicone hydrogel materials provide better end-of-day comfort and
less end-of-day dryness, and the research literature supports this observation to
some degree.2,7 Other research confirms silicone
hydrogels are no
less comfortable than conventional hydrogels.60
|
|
|
Figure 6: Epithelial proliferation rate in the central cornea, 24 hours after BrdU injection.5 Chart © 2003 Investigative Ophthalmology & Visual Science. Reprinted with permission of Access Copyright. |
This perception could result from the lower water content of silicone hydrogel materials, which do not dehydrate on the eye as quickly as other lens materials. Also, silicone hydrogel materials are treated to enhance wettability and comfort to make up for the hydrophobic nature of the silicone component. First-generation silicone hydrogel lenses display surface wettability similar to that of conventional hydrogels, according to a grading scale at the Cornea and Contact Lens Research Unit at the University of New South Wales, Sydney.59 However, two second-generation silicone hydrogels from Johnson & Johnson contain leachable materials that incorporate soluble polymers instead of hydrophilic coatings. The intent of this chemistry is to maintain lens wettability for longer-lasting comfort.
Truly Different Material
By now, it should be clear to eyecare practitioners that silicone hydrogel lenses are in a completely different league from their conventional hydrogel counterparts. However, it may take some effort to convince "happy HEMA" soft contact lens wearers that switching to silicone hydrogel lenses is in their best interest. The health and safety benefits offered by these lenses don't have as much impact on average contact lens wearers, particularly those who have been wearing conventional lens materials for some time with no perceptible problems. Still, practitioners must learn the benefits offered by higher oxygen transmissibility from the extensive resources that are available.




REFERENCES
1. Dumbleton K, et al. Vascular response to extended wear of hydrogel lenses with high and low oxygen permeability. Optom Vis Sci. 2001;78:137-151.
2. Brennan NA, et al. A 1-year prospective clinical trial of balafilcon A (PureVision) silicone hydrogel contact lenses used on a 30-day continuous wear schedule. Ophthalmology. 2002;109:1172-1177.
3. Fonn D, et al. The ocular response to extended wear of a high-Dk silicone hydrogel contact lens. Clin Exp Optom. 2002;85:176-182.
4. Malet F, et al. Clinical results comparing high-oxygen and low-oxygen permeable soft contact lenses in France. Eye Contact Lens. 2003;29:50-54.
5. Maldonado-Codina C, et al. Short-term physiologic response in neophyte subjects fitted with hydrogel and silicone hydrogel contact lenses. Optom Vis Sci. 2004;81:911-921.
6. Long B, McNally J. The clinical performance of a silicone hydrogel lens for daily wear in an Asian population. Eye Contact Lens. 2005;31:1-7.
7. Dumbleton K, et al. Redness, dryness and comfort following refitting long term low Dk hydrogel lens wearers with silicone hydrogels. Optom Vis Sci. 2004;81:31.
8. Roth H, et al. A silicone hydrogel for daily, flexible and extended wear. Optician. 2005;6013:20-25.
9. O'Neal MR, Polse KA, Sarver MD. Corneal response to rigid and hydrogel lenses during eye closure. Invest Ophthalmol Vis Sci. 1984;25:837-842.
10. Andrasko GJ. Corneal deswelling response to hard and hydrogel extended wear lenses. Invest Ophthalmol Vis Sci. 1986;27:20-23.
11. La Hood D, Sweeney DF, Holden BA. Overnight corneal edema with hydrogel, rigid gas-permeable and silicone elastomer contact lenses. Int Contact Lens Clin. 1988;15:149-154.
12. Fonn D, et al. Sympathetic swelling response of the control eye to soft lenses in the other eye. Invest Ophthalmol Vis Sci. 1999;40: 3116-3121.
13. Comstock T, et al. Overnight edema response of the PureVision lens. Cont Lens Anterior Eye. 1999;22:160.
14. Brennan N, Coles C. Overnight corneal swelling response of Pure-Vision toric. Optician. 2005;229:21-24.
15. Holden B, Mertz GW. Critical oxygen levels to avoid corneal edema for daily and extended wear contact lenses. Invest Ophthalmol Vis Sci. 1984;25:1161-1167.
16. Bullimore MA, et al. Overnight corneal swelling with 7-day continuous wear of soft contact lenses. Invest Ophthalmol Vis Sci. 2002;S43:Abstract 3100.
17. Mertz GW, Holden BA. Clinical implications of extended wear research. Can J Optom. 1981;43:203-205.
18. Cox I, Zantos SG, Orsborn G. The overnight corneal swelling response of non-wear, daily wear and extended wear soft lens patients. Int Contact Lens Clin. 1990;17:134-137.
19. Kiely PM, Carney LG, Smith G. Diurnal variations of corneal topography and thickness. Am J Optom and Physiol Opt. 1982;59:976-982.
20. Harper C, et al. Diurnal variations in
human corneal thickness.
Br J Ophthalmol. 1996;80:1068-1072.
21. Du Toit R, et al. Diurnal variation of corneal sensitivity and thickness. Cornea. 2003;22:205-209.
22. Fonn D., et al. Corneal oxygen deficiency. Eye Contact Lens 2005;31:23-27.
23. Holden B, Mertz G, McNally J. Corneal swelling response to contact lenses worn under extended wear conditions. Invest Ophthalmol Vis Sci. 1983;24:218-226.
24. Papas E. On the relationship between soft contact lens oxygen transmissibility and induced limbal hyperaemia. Exp Eye Res. 1998;67:125-131.
25. Papas E. High-oxygen-transmissibility soft contact lenses do not induce limbal hyperaemia. Curr Eye Res. 1997;16:942-948.
26. Nilsson SE. Seven-day extended wear and 30-day continuous wear of high oxygen transmissibility soft silicone hydrogel contact lenses: a randomized 1-year study of 504 patients. CLAO J. 2001;27:125-136.
27. Dumbleton K, et al. Changes in myopic refractive error with nine months' extended wear of hydrogel lenses with high and low oxygen permeability. Optom Vis Sci. 1999;76:845-849.
28. Chalmers RL, et al. Impact of previous extended and daily wear schedules on signs and symptoms with high-Dk lotrafilcon A lenses. Optom Vis Sci. 2005;82:549-554.
29. McMonnies CW. Contact lens-induced corneal vascularization. Int Contact Lens Clin. 1983;10:12-21.
30. Harris MG, Sarver MD, Polse KA. Corneal
curvature and refractive error changes associated with wearing hydrogel contact
lenses.
Am J Optom and Physiol Opt. 1975;52:313-319.
31. Hill RM, Variation in refractive error and corneal curvature after wearing hydrophilic contact lenses. Optometry. 1975;46:1136-1138.
32. Grosvenor T. Changes in corneal curvature and subjective refraction of soft contact lens wearers. Am J Optom and Physiol Opt. 1975;52:405-413.
33. Barentt WA, Rengstorff RH. Adaptation to hydrogel contact lenses: variations in myopia and corneal curvature measurements. Optometry. 1977;48:363-366.
34. Miller JP, Coon LJ, Meier RF. Extended wear of Hydrocurve II55 soft contact lenses. Optometry. 1980;51:225-230.
35. Binder PS. Myopic extended wear with the Hydrocurve II soft contact lens. Ophthalmology. 1989;90:623-626.
36. Jalbert I, et al. Changes in myopia with low-Dk hydrogel and high-Dk silicone hydrogel extended wear. Optom Vis Sci. 2004;81:591-596.
37. Holden BA, La Hood D, Sweeney DF. Prediction of extended wear microcyst response on the basis of mean overnight corneal response in an unrelated sample of non-wearers. Am J Optom Physiol Opt. 1987;64:S83.
38. Keay L, et al. Microcysts response to high Dk/t silicone hydrogel contact lenses. Optom Vis Sci. 2000;77:582-585.
39. Lavker RM, Tseng SCG, Sun T. Corneal epithelial stem cells at the limbus: Looking at some old problems from a new angle. Exp Eye Res. 2004;78:433-446.
40. Ren H, Wilson G. Apoptosis in the corneal epithelium. Invest Ophthalmol Vis Sci. 1996;37:1017-1025.
41. Jalbert I , Sweeney DF, Stapleton F. The effect of long term wear of soft lenses of low and high oxygen transmissibility on the corneal epithelium. Optom Vis Sci. 2005:82.
42. Wang, J, Fonn D, Simpson TL. Topographical thickness of the epithelium and total cornea after hydrogel and PMMA contact lens wear with eye closure. Invest Ophthalmol Vis Sci. 2003;44:1070-1074.
43. Jalbert I, et al. In vivo confocal microscopy of the human cornea. Br J Ophthalmol. 2003;87:225-236.
44. Ladage PM, Yamamoto K, Ren DH, Effects of rigid and soft contact lens daily wear on corneal epithelium, tear lactate dehydrogenase, and bacterial binding to exfoliated epithelial cells. Ophthalmology. 2001;108:1279-1288.
45. Ren DH, et al. Adaptive effects of 30-night wear of hyper-O2 transmissible contact lenses on bacterial binding and corneal epithelium: A 1-year clinical trial. Ophthalmology. 2002;109:27-39.
46. Cavanagh HD, et al. Effects of daily and
overnight wear of a novel hyper oxygen-transmissible soft contact lens on bacterial
binding
and corneal epithelium. Ophthalmology. 2002;109:1957-1969.
47. Stapleton F, et al. Short-term wear of high-Dk soft contact lenses does not alter corneal epithelial cell size or viability. Br J Ophthalmol. 2001;85:143-146.
48. Holden B, et al. Epithelial and endothelial effects from the extended wear of contact lenses. Curr Eye Res. 1985;4:739-742.
49. Yamamoto K, Ladage PM, Ren DH, Effect of eyelid closure and overnight contact lens wear on viability of surface epithelial cells in rabbit cornea. Cornea. 2002;21:85-90.
50. Li L, Ren DH, Ladage PM. Annexin V binding to rabbit corneal epithelial cells following overnight contact lens wear or eyelid closure. CLAO J. 2002;28:48-54.
51. Ladage PM, et al. Effects of eyelid closure and disposable and silicone hydrogel extended contact lens wear on rabbit corneal epithelial proliferation. Invest Ophthalmol Vis Sci. 2003;44:1843-1849.
52. Cavanagh HD, The effects of low- and hyper-Dk contact lenses on corneal epithelial homeostasis. Opthalmol Clin N Am. 2003;16: 311-325.
53. Ren DH, Yamamoto K, Ladage PM. Adaptive effects of 30-night wear of hyper-O2 transmissible contact lenses on bacterial binding and corneal epithelium: a 1-year clinical trial. Ophthalmology. 2002;109:27-40.
54. Cavanagh HD, Ladage PM, Li L. Effects of daily and overnight wear of a novel hyper oxygen-transmissible soft contact lens on bacterial binding and corneal epithelium: a 13-month clinical trial. Ophthalmology. 2002;109:1957-1969.
55. Cavanagh HD, et al. Effects of daily and overnight wear of hyper-oxygen transmissible rigid and silicone hydrogel lenses on bacterial binding to the corneal epithelium: 13-month clinical trials. Eye Contact Lens. 2003;29:S14-S16.
56. Jalbert I, Stapleton F. The corneal stroma during contact lens wear. Cont Lens Anterior Eye. 2005;28:3-12.
57. Jalbert I, Stapleton F. Effect of lens wear on corneal stroma: preliminary findings. Aust NZ J Ophthalmol. 1999;27:211-213.
58. Böhnke M, Masters BR. Long-term contact lens wear induces a corneal degeneration with microdot deposits in the corneal stroma. Ophthalmology. 1997;104:1887-1896.
59. Sweeney DF, et al. Clinical performance of silicone hydrogel lenses. Silicone Hydrogels: Continuous Wear Contact Lenses. 2004; 164-216.
60. Fonn D, Dumbleton K. Dryness and discomfort with silicone hydrogel contact lenses. Eye Contact Lens. 2003;28:s101-s104.