contact
lens case reports
A New Look at Vascularized Limbal Keratitis, Part 1
BY
PATRICK J. CAROLINE, FAAO, & MARK P. ANDRé,
FAAO
Vascularized limbal keratitis (VLK) is a rigid lens-induced inflammatory complication hallmarked by an elevated peripheral corneal nodule most commonly located along the horizontal meridian at three or nine o'clock. The nodules appear related to chronic irritation of the peripheral cornea secondary to large-diameter, minimal-edge-lift lens designs.
|
|
|
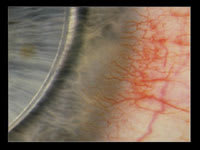
Figure 1. Early-stage VLK. |
Differentiating VLK
In the early stages of VLK, patients report a localized intrapalpebral injection with moderate ocular irritation and lens awareness. Early clinical manifestations include a slightly elevated, opaque corneal nodule approximately 0.25mm to 0.50mm from the limbus, along the horizontal meridian. This may be accompanied by coalesced superficial punctate keratopathy at three o'clock or nine o'clock with conjunctival hyperemia (Figure 1).
In the later stages, patients can report a significant decrease in lens tolerance that's often accompanied by photophobia and pain. Ocular findings include localized corneal edema with adjacent intrapalpebral conjunctival hyperemia. A vascular leash crosses the limbus to the elevated nodule with both superficial and deeper stromal vascularization. Recurrent epithelial erosion, at the apex of the nodule, is a common clinical finding.
Treatment
VLK is self-limiting. Following discontinuation of rigid lens wear, the lesions slowly (over a period of weeks) melt away. However, lens design changes are necessary to reduce mechanical trauma to the peripheral cornea and to prevent reoccurrence. This is often best accomplished by reducing the overall lens diameter by 0.5mm or more. Additionally, you can flatten the base curve and/or peripheral lens design to lessen lens tightening, which can result in peripheral corneal trauma. Frequent ocular lubricants are also suggested.
Advanced stages of the condition may require lens wear discontinuation for seven to 21 days. You can topically treat the lesion with a seven- to 10-day course of a combination antibiotic/steroid drop. To avoid VLK recurrence, make appropriate lens design changes (as described above).
Our VLK Case
|
|
|
Figure 2. DB's right eye VLK lesion. |
Patient DB is a 28-year-old female with a 12-year history of GP contact lens wear. She presented with a three-month history of increasing lens intolerance, right eye only. Slit lamp examination showed a classic, late-stage VLK lesion near the nasal limbus OD (Figure 2).
To date, ophthalmic literature has never described the exact histological makeup of VLK lesions. DB agreed to have her lesion biopsied for detailed histologic examination, the results of which we will present next month.
Patrick Caroline is an associate professor of optometry at Pacific University and is an assistant professor of ophthalmology at the Oregon Health Sciences University. He is also a consultant to Paragon Vision Sciences and SynergEyes, Inc. Mark André is director of contact lens services at the Oregon Health Sciences University and serves as an assistant professor of optometry at Pacific University. He is also a consultant for Alcon Labs, CooperVision and SynergEyes, Inc.