POST-LASIK ORTHO-K
Fitting
Post-LASIK Progressive Myopes with Accelerated Ortho-k
Reverse-curve
lenses and overnight orthokeratology offer an excellent alternative to additional
surgery.

After having successfully fit many orthokeratology patients, and having tentatively avoided post-LASIK and other post-refractive surgery patients who requested that I help improve their declining distance vision, I decided to research the literature to see if I could find any significant contraindications to post-refractive surgery contact lens corneal reshaping. I found three studies that provided some insight.
Alharbi and Swarbrick (2003) indicated that the reduction in myopia with orthokeratology results from epithelial thinning and increased stromal thickening in the midperiphery. The consequent change in corneal sagittal height and curvature is the primary factor underlying the ortho-k refractive effect. Reverse geometry lenses appear to cause a migration of the epithelial cells to the lower-pressure area under the reverse curve.
Wang et al (2003) from the University of Waterloo in Waterloo, Ontario, Canada used optical coherence tomography to measure thickness changes in the epithelium as well as total corneal thickness. Their findings indicated that, "Immediately after removal of the test lens, the central epithelium was 5.1 percent ± 4.5 percent thinner than baseline, and all other locations (P < 0.005 post hoc tests) and the epithelium in the midperiphery showed significant thickening (1.9 percent on the temporal side and 2.4 percent on the nasal side, both P < 0.006 compared with the baseline). There were no significant changes in epithelial thickness with the control lens during the study period (post hoc tests: P > 0.05)."
Sridharan and Swarbrick (2003) concluded that the ortho-k response results from the redistribution of the corneal epithelium.
|
|
|
Figure 1. Difference map OD of Patient FS following overnight ortho-k treatment. |
Getting Started
Because of the relatively small (only about 5 percent) changes in the tissues involved, I felt it safe to perform orthokeratology on post-refractive surgery patients. Careful monitoring to grade changes in the cap interface and position, as well as microfolds, Bowman's cracks or any evidence of cap dehiscence, is a critical part of follow up for these patients.
Fitting reverse curve lenses is generally straight forward. The base curve is a mathematical calculation that's based on either the spherical correction or the spherical equivalent and the flat curve or mean curve on the cornea. Some reverse curve lenses are fit using the e-value or slope of the cornea as measured from the center to the periphery. Others use a four-curve design that contains a base curve, a return curve, a landing zone with a plano or flat flap, and an engineered edge to provide proper fluid control. I've used several designs and have found that they all have advantages and disadvantages for specific corneas. Very steep corneas respond better to thicker, traditional lathe-cut and polished four-curve designs while "average" curvatures respond well to a thinner, "harmonic surface" design. Very flat corneas remain challenging and, depending on the amount of myopia, you can attempt fitting them in stages using a very thin design and a larger diameter than that of lenses used on an average cornea.
Fitting Post-refractive Surgery Patients
My intention wasn't to re-invent reverse-curve lenses to accommodate post-refractive surgery corneas, but to use the current technology.
Getting the proper fluorescein pattern with a reverse-curve, accelerated ortho-k lens was a challenge when fitting post-LASIK patients because of the relatively flat optical zone with respect to the steeper midperipheral cornea. After trying several lens designs, I was able to achieve the best patterns with the flexibility of the adjustable return zone depths (RZD) and landing zone angles (LZA) of Paragon CRT lenses.
|
|
|
Figure 2. Difference map OS of Patient FS following overnight ortho-k treatment. |
I initially fit four post-refractive surgery patients with Paragon CRT. This is currently an off-label use of these lenses. Because the myopia was mild in all of these cases, ranging from –0.75D to –1.75D, I felt that the procedure would be safe because it involved a minimal amount of tissue movement. The following reports describe three of these four very successful post-refractive surgery cases — two LASIK and one PRK — achieved with Paragon CRT.
Case #1 Patient FS is a 36-year-old male who underwent LASIK surgery in 1997 with a pre-op refraction of OD –7.75 –0.75 x 070 and OS –7.75 –0.75 x 090. His refraction one-day post-op was OD plano –0.50 x 005 and OS plano –0.75 x 010.
By 1998, his refraction had slipped to OD –0.50 –0.50 x 010 and OS –0.25 –0.75 x 180.
By 2001 his refraction was OD –1.25 –0.50 x 010 and OS –0.25 –0.50 x 175.
In the summer of 2002, we found that his refraction had progressed to OD –1.25 –0.75 x 010 and OS –1.00 –0.50 x 175.
Finally, by the summer of 2003 he measured OD –1.75 –0.25 x 010 and OS –1.00 –0.50 x 170, and he was wearing eyeglasses full time. BCVA was 20/20 at all visits.
I began the procedure in July 2003. I determined a base curve of 8.9mm OD based on FS's manifest refraction sphere (MRS) of –1.75D and flat K of 40.37D. I determined a base curve of 8.8mm OS based on his MRS of –1.00D and flat K of 40.00D. I achieved the best fluorescein patterns with RZDs and LZAs of 500μ and –34 degrees respectively.
We saw FS the next morning while he was still wearing the lenses. Although the refraction had improved to OD +0.25 –1.00 x 010 and OS plano –0.50 x 150, the fluorescein pattern had sufficiently changed to indicate that there was excessive edge lift. I didn't want to lose the central bearing, so I replaced these initial lenses with a second set that had the same base curves, but I reduced the RZDs to 475μ and increased the LZAs to –35 degrees.
|
|
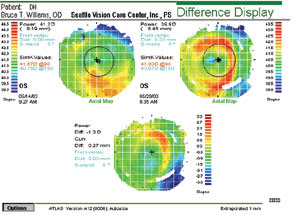
| Figure 3. Difference map OD of Patient DH following overnight ortho-k treatment. |
This lens provided the best fit for the left eye, but I still had centering problems with the right lens. I increased the LZA OD to –37 degrees. I wanted to achieve a final correction of OD +0.25 DS and OS plano. FS's visual acuity is 20/20 OU, and he wears the lenses every other night and is happy with the results. Figures 1 and 2 show the difference maps OD and OS following FS's ortho-k treatment.
Case #2 Patient DH is a 31-year-old male who'd undergone LASIK approximately three years prior. He came to our practice for punctal plugs because his surgeon had suggested that his poor vision resulted from dry eyes. His uncorrected visual acuities were 20/80 OD and 20/60 OS and his refraction measured –1.25D OD and –1.00D OS.
We trial fit and dispensed Paragon CRT lenses with parameters of 8.7mm base curve, 475μ RZD and LZA of 34 degrees OD and 8.6mm base curve, 475μ RZD and LZA of 34 degrees OS. His subsequent refraction was plano OD and +0.25D OS. Figures 3 and 4 show the subsequent difference maps.
Case #3 Patient SR is a 37-year-old male who'd undergone PRK four year prior. He reported that his vision was fuzzy like a wet windshield. His refraction was –1.25D OD and –0.75D OS. I noted some residual haze at the level of the pupil margins and the mires were slightly distorted.
I fit SR with Paragon CRT lenses with parameters of 8.6mm base curve, 500μ RZD and LZA of 33 degrees OD and 8.5mm base curve, 500μ RZD and LZA of 33 degrees OS. His refraction is now plano OU. It's important to note that his vision is much crisper because of reduced surface irregularities from the procedure, which not only flattens the cornea but smoothes the surface as well.
A Great Alternative
|
|
|
Difference map OS of Patient DH following overnight ortho-k treatment. |
After monitoring my four patients for several months and seeing no change in the appearance of their refractive surgery aftermath, I've concluded that the ortho-k procedure is safe and effective for such patients. They're happy to have an alternative to surgical enhancement or re-treatment. Don't be afraid to ask lens manufacturers to accommodate curvatures and diameters to achieve the optimum results for these patients. I find manufacturers very helpful and anxious to know about my patients' progress.
I feel that the opportunity to actively participate in controlling myopia in post-refractive surgery patients is a responsibility of the eyecare profession whether we use conventional or orthokeratology lenses. Overnight ortho-k lenses offer patients an alternative to the current options of additional surgery, daytime spectacles or contact lenses. Corneal refractive therapy/ortho-k is another tool to help us provide our patients with optimal visual quality and convenience.
Dr. Williams is a member of the American Optometric Association, the Orthokeratology Academy of America, the British Contact Lens Association and the British Ortho-K Society. He practices in Seattle, WA, in a contact lens-focused general practice that specializes in orthokeratology. He has also given several presentations on the subject of orthokeratology.
The author has no financial or proprietary interest in any of the products mentioned in this article.
For references article, visit www.clspectrum.com/references.asp and click on document #123.