contact
lens practice pearls
Staff
Dispensing of GP Lenses
BY
THOMAS G. QUINN, OD, MS, FAAO
Contact lens dispensing is a task well-suited for your technicians. I find this most beneficial when a GP lens wearer loses or breaks a lens and needs a simple replacement. Here's how I instruct my staff to dispense GP lenses.
Understand the Goal
I begin by emphasizing that their role in dispensing a new lens is to ensure that the patient is seeing as expected with a comfortable lens that is positioning and moving well on the eye.
Prep Work
We verify all GP lenses for accuracy when they arrive from the lab. I emphasize measuring not only base curve, power and diameter, but also optic zone size and center thickness. These variables are frequently overlooked but can significantly affect on-eye lens performance.
Once the lenses are deemed acceptable, our technician cleans them and then stores them in the appropriate conditioning solution for at least four hours before dispensing. We take these steps to ensure a clean, smooth lens surface.
|
|
|
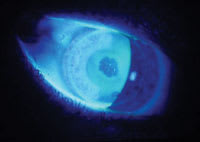
Figure 1. Poor surface wetting of a GP lens on the eye. |
Dispensing Day
If the patient applies the lenses, our technician makes sure the patient washes his hands before handling the lenses. Aside from hygiene issues, lotions or skin oils can wreak havoc on a lens surface.
Note the time lenses are applied in the chart, then invite the patient to the reception area for the lenses to settle for at least 10 minutes. This time frame is important when dispensing special lens designs such as multifocals, as visual performance improves significantly after lenses have adequate time to stabilize on the eye.
Assessing Vision
After the patient returns to the examination room, the technician should begin by asking an open question regarding initial impressions of comfort and vision. This response can be a valuable guide if troubleshooting is necessary.
Before measuring visual acuity, I advise the technician to review the chart to determine expected acuity and familiarize herself with the lens design. Understanding expected acuity prevents being thrown by a patient who has amblyopia or is wearing monovision.
If dispensing a single-vision lens, measure monocular distance acuity in each eye. If dispensing a multifocal, increase room light to normalize pupil size, then measure binocular acuity at distance and binocular acuity at near. Use a text chart at near. These steps ensure a more accurate assessment of lens performance in a real world environment.
If visual acuity isn't as good as expected, the technician instills fluorescein and assesses surface wetting. Adhering to the prep work minimizes the need to manage a poorly wetting surface.
Assessing Lens Fit
The key fitting criteria for both soft and GP lenses are good lens centration and movement. GP lenses offer the added benefit of permitting instillation of fluorescein so we may assess how the curves of the central and peripheral portions of the lens relate to the corneal surface.
Fitting notes for GP lenses should describe lens centration and movement, base curve/cornea relationship and peripheral curve lift. The GP Lens Institute (www.gpli.org) offers resources to assist staff with fit assessment.
The Next Level
My technicians enjoy the challenges and the expertise they develop from dispensing contact lenses. Patients like it because we're more available to get their lenses to them at their convenience. Everyone is happy!
Dr. Quinn is in group practice in Athens, Ohio, is a diplomate of the Cornea and Contact Lens Section of the American Academy of Optometry and advisor to the GP Lens Institute.