HYBRID SPECIALTY FITS
Fitting Irregular
Corneas with a Hybrid Lens
Learn
step by step how to fit keratoconic, post-surgical and other irregular corneas with
hybrid lens designs.
By Michael DePaolis, OD, FAAO, Jane Beeman,
COT, FCLSA, & Robert Ryan, OD, FAAO
The emergence of a newer-generation soft skirt hybrid lens modality has resulted in as much of an evolution in fitting methodology as in material science. The SynergEyes family of lenses (SynergEyes, Inc.) offers multiple FDA indications ranging from the full continuum of naturally occurring ametropia and presbyopia to irregular astigmatism resulting from keratoconus, refractive surgery and corneal trauma. The broad indications have opened the door for clinicians to harness the potential of these new designs.
New Materials, New Fitting Techniques
During the SynergEyes FDA clinical trials, clinicians used fitting methods similar to those with previous-generation hybrid lenses. The learning that took place was manifold. Apical clearance quickly replaced alignment fitting in an effort to increase post lens tear film thickness given the surface properties of the hyper-Dk rigid material. We now generally recommend central clearance of at least 30μm on most eyes.
Controlling apical clearance goes beyond modulating the base curve radius. SynergEyes offers multiple skirt curve radii for a given base curve radius. The Total Clearance Technique recommended for the SynergEyes KC (keratoconus) and PS (post surgical) lenses determines the optimum parameters from the center of the lens outward.
|
|
|
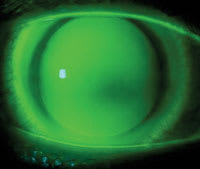
Figure 1. SynergEyes KC on a post-LASIK patient. |
Total Clearance Technique for Keratoconus
The SynergEyes KC design is a prolate ellipse with a fixed eccentricity for all base curve radii. The base curve continues to a diameter of 9mm where it transitions to a spherical skirt curve radius that terminates at a peripheral bevel. The lens is designed to clear the keratoconic cornea until a feather touch at 9mm. The skirt should align with the peripheral cor-nea and suspend the lens above the cornea from the 9mm chord inward.
For the initial diagnostic lens, we recommend that you use keratometry or topography (simulated keratometry) values to determine a lens closest to the steep meridian as a starting point. Consider cone morphology, assessing the keratoconus as either a globus, oval or nipple type. A base curve approximately 2.00D flatter than the steep meridian is more appropriate for a nipple cone, while a base curve closer to the steep meridian is required for a globus cone. Use the flattest skirt curve radius in the initial diagnostic lens.
The goal is to observe total apical clearance without bubbles larger than 1mm. Occasionally, bubbles indicate air trapped in the retrolens space upon application and are transitory in nature. Simply removing the lens, placing a drop of high molecular weight fluorescein in the bowl and reapplying the lens will resolve this issue. However, persistent bubbles warrant a base curve change. When a base curve provides total clearance free of bubbles, the next step is to optimize the skirt curve radius.
Optimizing Skirt Curve Radius The base curve radius that meets the above conditions in conjunction with the flattest skirt may be ideal. The determining factor is the presence or absence of a dark ring of touch at about a 9mm chord. If a dark ring is present, the touch at the base curve/skirt curve is too heavy, which may lead to late onset tightening. Reduce the dark ring of touch by using a steeper skirt curve radius.
The proper step in this case is to keep the same base curve radius and go to the next steeper skirt curve radius. Continue to steepen the skirt curve radius until you observe a feather touch at the 9mm chord, which assures adequate contact lens vaulting and continual blink-induced movement.
Optimizing Base Curve Radius Bubbles may sometimes reappear under the optic zone when the proper skirt curve is in place. When this occurs, flatten the base curve by 0.1mm to eliminate the bubble. Once the bubble is gone and you observe a feather touch at 9mm, the diagnostic fitting is complete and you can over-refract to determine lens power.
Case Study A 47-year-old female presented having undergone well-healed LASIK OU four year ago with two enhancements OU. She had a post-surgical ectasia and complained of blurred vision and dryness. Biomicroscopy revealed inferior thinning and epithelial pigment OU. Her K readings were OD 48.00/56.00 and OS 42.50/49.75, and her refraction was OD +2.00 –7.50 x92 = 20/100 and OS +2.00 –6.50 x88 = 20/60. We fit her with SynergEyes KC with parameters of 6.90mm base curve, 8.5mm skirt curve, 14.5mm diameter, –8.50D 20/30+ OD and 6.70mm base curve, 8.5mm skirt curve, 14.5mm diameter, –6.50D 20/25 OS. Figure 1 shows the fluorescein pattern OS. The patient wears the lenses for approximately 14 hours each day.
Total Clearance Technique for Irregular Oblate Corneas
|
|
|
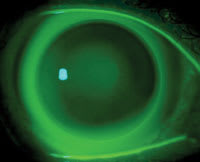
Figure 2. SynergEyes PS features three sagittal depths. |
Refractive surgery for myopia including RK, PRK, LASIK and Intacs (Addition Technology) renders corneas oblate in geometry. In addition, some corneas that undergo penetrating keratoplasty, experience mechanical trauma or develop pellucid marginal degeneration may be best suited for an oblate lens design. The SynergEyes PS lens features a spherical base curve that transitions into an oblate ellipsoidal zone that continues to a diameter of 9mm, where it transitions to a spherical skirt curve radius that terminates at a peripheral bevel.
The lens is designed to clear the irregular central cornea until a feather touch at 9mm. The skirt should align the peripheral cornea and suspend the lens above the cornea from the 9mm chord inward.
The PS lens offers fewer constraints on the base curve radius of the initial diagnostic lens because you can use the oblate ellipsoid portion of the base curve to create clearance. For post refractive surgery, the optimal base curve is frequently what results in a near plano lens power. The goal of the optimum base curve is to represent the closest reference sphere to the cornea to reduce the potential for bubbles. A base curve approximately equal to the average of the flat and steep meridians is a good starting point. As with the KC design, we recommend the flattest skirt curve in the initial diagnostic lens.
The goal is to observe total apical clearance without bubbles larger than 1mm. When a base curve provides total clearance free of bubbles, the next step is to optimize the skirt curve radius.
Optimizing Skirt Curve Radius It's possible to observe total alignment with little highs and lows in the base curve but not complete clearance. If you observe alignment with inadequate clearance or if clearance with a dark ring at the 9mm chord is present, the lens is not adequately suspended over the cornea and late onset lens tightening may occur. You can reduce the central alignment or the dark ring of touch by going to a steeper skirt curve radius.
The proper step in this case is to keep the same base curve radius and go to the next steeper skirt curve radius. Continue to steepen the skirt curve radius until you observe clearance over the cornea with a feather touch at the 9mm chord.
Optimizing Base Curve Radius Once again, bubbles may sometimes reappear under the optic zone when the proper skirt curve (that lifts the optic zone and the junction to a feather touch) is in place. When this occurs, flatten the base curve by 0.1mm to eliminate the bubble. Once you eliminate the bubble with the flatter base curve and proper skirt curve, diagnostic fitting is complete. The final step is an over-refraction to determine lens power.
Sagittal Depth Factor Options Irregular corneas are the sequelae of disease, trauma and surgery and demonstrate extreme geometric diversity. A single oblate sagittal depth isn't adequate to properly fit the continuum of post-surgical irregular eyes. SynergEyes PS is available in three sagittal depths or Sagittal Depth Factors (shallow, medium and deep, Figure 2) to accommodate the geometric diversity. Standard diagnostic lenses are in the medium depth.
When the otherwise optimum base curve that parallels the cornea exhibits too much depth with the flattest skirt curve, the shallow depth is indicated. You may also observe a lens in the proper base curve that demonstrates heavy touch or alignment on the central cornea that you can't eliminate by suspending the lens with the steepest skirt curve radius. These cases require the deep Sagittal Depth Factor. This option provides a strategy to modulate sagittal depth in the presence of an optimal base curve/skirt radius relationship. Without this option, you could only steepen the base curve in an effort to achieve clearance, and central bubbles would frequently result due to the mismatch of the base curve and the central corneal radius.
Case Study A 41-year-old male presented having undergone well-healed LASIK OU. Biomicroscopy revealed corneal thinning OU. His topography maps showed oblate post-LASIK corneas OU. Keratometry readings were OS 37.25/39.00. We fit him with a SynergEyes PS lens OS with parameters of 8.76mm base curve, 8.2mm skirt curve, 14.5mm diameter, plano power, 20/25 (Figure 3), giving the patient a wear time of 14 hours each day.
|
|
|
Figure 3. SynergEyes PS lens on a post-LASIK, oblate cornea. |
Diagnostic Lens Considerations
The SynergEyes KC and SynergEyes PS each come in a 24-lens diagnostic set configured with three skirt curve radii for each of eight base curve radii. The SynergEyes KC base curves are in 0.2mm steps while SynergEyes PS are in 0.3mm steps and the skirt curve radii for each are steep, median and flat. We recommend large-molecule fluorescein, and evaluating the pattern is essential. You can observe lenses upon application and in some, but not all, cases we recommend another observation after 15 minutes.
Achieving a pattern that is free of central touch or alignment and free of a heavy 9mm touch is the best prevention of late onset tightening. In our experience, patients will report a mild awareness of the lens when 9mm touch is too heavy.
Hybrid lenses are known for the counter intuitive characteristic of exhibiting more movement when fit steeper. A proper sagittal depth clearance of about 30μm under the rigid portion is the key to ensuring all day comfort, consistent vision and an optimal physiologic response for compromised corneas.
Dr. DePaolis is in group practice in Rochester, NY. He also serves as a clinical associate faculty member at the University of Rochester Medical Center and is on the Board of Directors at TLC Vision.
Ms. Beeman holds an advanced level certification in contact lens fitting from the National Contact Lens Examiners and is also certified as an ophthalmic assistant. She is in clinical practice in Rochester, NY, and is the Academic Education Coordinator for the GP Lens Institute.
Dr. Ryan is in group practice in Rochester, NY. He has also been appointed Clinical Associate in Ophthalmology at the University of Rochester, School of Medicine.