Fitting Reverse Geometry Lenses for Keratoconus
This lens design may improve best corrected
visual acuity and reduce aberrations for keratoconus patients.
By Paul A. Kusy, OD, MS, & Joseph T. Barr, OD, MS, FAAO

Methods
|
|
|
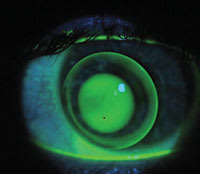
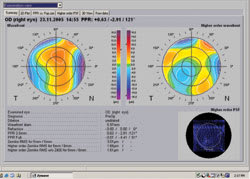
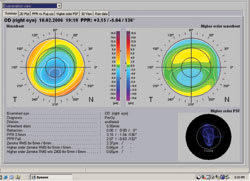
Figure 1 |
|
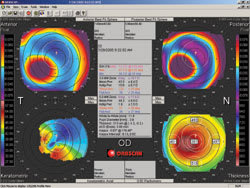
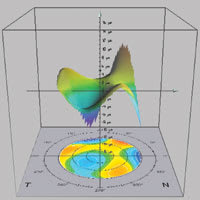
| Figure 2 |

|
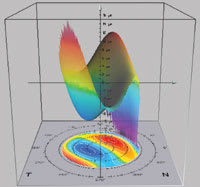
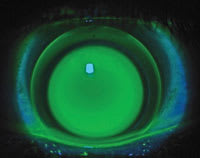
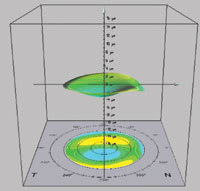
| Figure 3 |
|
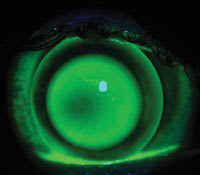
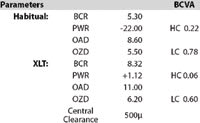
| Figure 4 |
We obtained data from a group of patients (n=13) wearing a variety of KC contact lens designs. Measurements we took while the patients wore each of the lenses included high contrast (HC) and low contrast (LC) Bailey-Lovie BCVAs and the HC/LC (mixed contrast) Nearpoint card. We measured aberrations using the Bausch & Lomb ZyWave Aberrometer, and we used the B&L Orbscan II system to measure decentration between the center of the contact lens and the visual axis. We performed these measurements on each subject with both lens designs and then compared the measurements.
Results
The BCVA HC, LC and amount of lens decentration of the standard design ranged from 20/47 to 20/20 HC, 20/118 to 20/30 LC and 2.44mm to 1.00mm decentration. The range for the XLT lens design ranged from 20/13 to 20/42 HC and 20/25 to 20/115 LC. The level of aberration variance (coma) among lenses was 3.47μm to 0.25μm with standard lenses and 0.72μm to 0.16μm with the reverse geometry XLT lens (MedLens Innovations, Inc., manufactured in Contamac materials). The graph on page 26 compares the magnitude of each patient's coma with their habitual lenses and with the XLT lenses. The XLT lens required a reduction of power ranging from 2.00D to 22.00D in comparison to standard design lenses in this study.
The amplitude of decentration and the power of contact lenses are directly proportional to the BCVA and the measured level of aberrations.
A Closer Look at Two Subjects
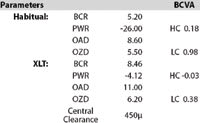
Table 1 and Table 2 illustrate the results of two patients from our study, providing the measurements first with their habitual contact lenses and then with the XLT contact lens (BCVA –0.03~20/20, 0.38~20/50).
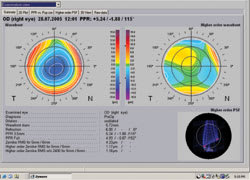
Subject #1 Figure 1 shows Subject 1 wearing an 8.6mm overall diameter regular geometry contact lens. Figure 2 shows the initial topography, which demonstrates decentration of the apex. Our aberrometry measurements show that these habitual lenses resulted in a high amount of overall aberrations (Figure 3). Figure 4 shows a three-dimensional illustration of this patient's higher-order aberrations, which measured 3.56μm on the right eye with the habitual lens design.
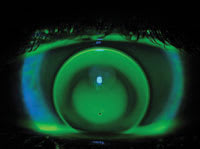
Next we fit the patient with an 11.0mm OAD XLT reverse geometry lens and checked the lens fit with fluorescein (Figure 5). The aberrometry readings in Figure 6 indicate the amplitude of aberrations with the same patient in the XLT lens design. Figure 7 shows the three-dimensional illustration of a decreased level of higher-order aberrations, which measured 1.17μm OD with the XLT lens design.
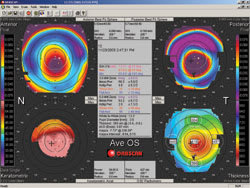
Subject #2 Figure 8 shows Subject #2 wearing an 8.6mm OAD regular geometry contact lens. The initial topography in Figure 9 illustrates the location of the apex. Figure 10 shows the aberrometry readings indicating the amplitude of aberrations with this patient's habitual lens. A three-dimensional illustration of higher-order aberrations measuring 1.65μm OD with the habitual contact lens design appears in Figure 11.
Next we fit Subject 2 with an 11.0mm OAD XLT reverse geometry lens (Figure 12). Figure 13 shows the amplitude of aberrations with the same patient in the XLT lens design. Figure 14 shows a three dimensional illustration of a decreased level of higher order aberrations measuring 0.66μm on the right eye with the XLT lens design.
Conclusions
The BCVA and aberration of the KC patients fit with contact lenses can vary depending on the centration and power of the lens. Factors that result in a higher level of BCVA and lower aberrations include reduced decentration and power. In this study, the XLT lens consistently provided better vision and lower aberration, as compared to the patients' habitually worn GP lenses.
|
|
|
| Figure 5 | Table 1 | Figure 6 |

|
|
|
| Figure 7 | Figure 8 | Figure 9 |
|
|
|
| Figure 10 | Figure 11 | Figure 12 |
|
|
|
| Table 2 | Figure 13 | Figure 14 |
Dr. Kusy recently graduated from The Ohio State University College of Optometry with an MS in Vision Science and was previously on staff at the Cleveland Clinic Foundation Cole Eye Institute.
Dr. Barr is a professor and associate dean for clinical services and professional program at The Ohio State University College of Optometry.