orthokeratology today
Troubleshooting Astigmatic Orthokeratology Fits
BY JOHN MOUNTFORD, DIP. APP. SC, FAAO, FCLSA
Practitioners often ask me to review difficult orthokeratology cases that haven't gone according to plan. In other words, they haven't achieved the refractive target or there's unwanted residual astigmatism. In the huge majority of cases, the simple truth is that the practitioners have forgotten the basic rules that govern the success or failure of ortho-k.
Adjust Your Expectations
The most common mistake is that they haven't properly reconciled the pre-fit refractive astigmatism and the corneal astigmatism. The FDA has approved most of the corneal reshaping lenses for reducing up to 6.00D of myopia and 2.00D of astigmatism, but these are the exceptions rather than the rule.
|
|
|
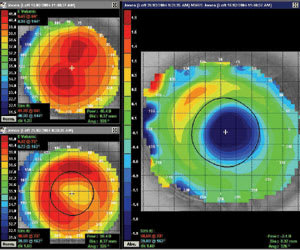
Figure 1. Mildly astigmatic cornea fit with a spherical lens. |
|
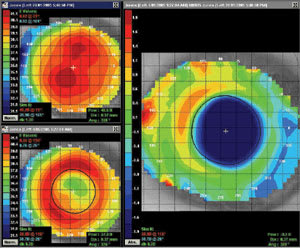
| Figure 2. Same eye with a toric lens, showing improved ortho-k effect. |
Published studies show either no reduction of astigmatism or, at best, a 50-percent reduction of corneal astigmatism over the central 2.00mm chord. Therefore, if a patient has 2.00D of pre-fit astigmatism, the best possible outcome is a residual 1.00DC.
So, let's have a quiz: What's the likely outcome for the following four patients?
1. The refraction is �2.50/�1.50 @ 180 with K readings of 44.00D sphere.
2. Same Rx as above, but the K readings are 44.00D @ 180 and 45.50 @ 90.
3. Same Rx as above, but the K readings are 44.00D @ 180 and 44.50 @ 90.
4. The refraction is �2.50/�1.00 @ 180. The K readings are 44.00 D @ 180 and 46.00 D @ 90.
I'd really like to see some answers to these questions, which I may include in a later column. Send them to besty@bigpond.net.au. The most important hint I can give is that you should always compare the refractive to the corneal cylinder and take into account the likely effects of induced lenticular astigmatism.
Review the Topography
The second most common problem is that the practitioner has poorly understood the pre-fit corneal map. The most common cause of chronic lens lateral decentration is a markedly flatter nasal cornea compared to the temporal cornea, and superior decentration resulting in a difference of greater than 50μm of corneal sag between the flat and steep meridians.
Figure 1 shows a mildly astigmatic cornea fit with a spherical lens. The difference in sag was 58μm between the flat and steep meridians. Note the small treatment zone, and the K readings showed an increase of the corneal cylinder from 1.20D to 1.609D.
Figure 2 shows the same eye fit with a "toric" lens where the difference in sag between the steep and flat meridians was 50μm. Note three main improvements: Increased treatment zone diameter, better centration and decreased lateral decentration, all resulting in an increased prescription change.
Dr. Mountford is an optometrist in private practice specializing in advanced contact lenses for keratoconus, post refractive surgery and pediatric aphakia. He is a visiting contact lens lecturer to QUT and UNSW, Australia.