MANAGING KERATOCONUS
Piggyback Lens
Systems for Keratoconus
Fitting
a silicone hydrogel/GP lens combination may improve comfort and vision for keratoconic
patients.

Keratoconus is a corneal ectasia characterized by progressive corneal thinning, steepening and apical scarring. Presenting with variable amounts of irregular astigmatism, practitioners most often correct the resultant corneal distortion with GP lenses. Despite the success with GP lens wear in many keratoconic patients, problems with decreased comfort and wearing time may lead to lens intolerance as the condition progresses.

As keratoconus worsens, specialty soft keratoconic lenses, such as the Flexlens Tri-curve Keratoconus lens (X-Cel), are an option. Limited success with these lenses often results from low oxygen permeability (Dk), resulting in hypoxia and corneal neovascularization. Some hybrid lens designs, such as the SoftPerm lens (CIBA Vision), improve comfort and lens positioning, but these tight-fitting lenses often lead to similar complications associated with hypoxia.
Piggyback Systems
Piggyback lens systems date back to the early 1970s. First reported attempts at this combination lens fitting technique occurred in 1964 by Westerhout with results published in 1973, in which successful fitting of five dual-lens systems in keratoconic patients resulted in 14 to 16 hours of wearing time with good comfort and vision.
Consisting of a GP lens fit on top of a soft lens, older piggyback lens systems often resulted in corneal edema and neovascularization due to hypoxia. With improved GP and soft lens materials that offer higher Dk, piggyback lens systems have resurfaced as a viable option for keratoconic patients. Research shows that we can achieve the physiological corneal oxygen requirements necessary to reduce and prevent edema with these higher-Dk combination lenses.
This clinical study examines the comfort and visual quality outcomes of fitting a piggyback contact lens system utilizing an 8.3mm base curve silicone hydrogel soft lens (Acuvue Advance, Vistakon) on keratoconic patients who were current successful GP contact lens wearers.
|
TABLE 1 |
|||
| GP Materials Used in Successful Piggyback Fittings | |||
|
SUCCESSFUL
PIGGYBACK FITTINGS |
SUCCESSFUL PIGGYBACK DROPOUTS | ||
| Material | Dk | Material | Dk |
| Paraperm 02 | 16 | Unknown | |
| Paraperm 02 | 16 | Unknown | |
| Fluoroperm 30 | 30 | Unknown | |
| Fluoroperm 60 | 60 | Unknown | |
| Boston EO | 58 | Paraperm 02 | 16 |
| Boston EO | 58 | Paraperm 02 | 16 |
| Boston EO | 58 | ||
| Boston ES | 18 | ||
| Boston ES | 18 | ||
| Fluoroperm 30 | 30 | ||
| Fluoroperm 30 | 30 | ||
| Unknown | |||
| Unknown | |||
| Fluoroperm 30 | 30 | ||
| Fluoroperm 30 | 30 | ||
| Fluoroperm 60 | 60 | ||
| Fluoroperm 60 | 60 | ||
| Unknown | |||
| Unknown | |||
| Fluoroperm 30 | 30 | ||
| Fluoroperm 30 | 30 | ||
| Bolded material=new gas permeable lenses ordered for the study. | |||
Patients and Methods
We enrolled 16 mild-to-advanced keratoconic patients (30 eyes) at SUNY College of Optometry who were current GP wearers and had no additional ocular pathology in this study and followed them for a minimum of four weeks after a successful piggyback fitting. In the two patients who had only one eye each enrolled in the study, we excluded the fellow eyes because they didn't wear a GP lens on those eyes. Eligible patients must have worn a successful piggyback lens system for at least four consecutive weeks with acceptable visual acuity and absence of corneal compromise.
The mean age of eight females (15 eyes) and eight males (15 eyes) was 44.5 years ±13.33 SD (range 18 to 73 years). In this study, the average age for the initial keratoconus diagnosis was 29.13 years ±13.34 SD (range 14 to 68 years) and the average age when these patients first started wearing GP lenses was 27.8 years ±9.64 SD (range 14 to 45 years).
We performed a comprehensive pre-fitting evaluation on all patients, including case history, pre-fitting questionnaire (Appendix A, available in the online version of this article at www.clspectrum.com), verification of current GP lens parameters, fitting evaluation of current GP lenses, keratometry, subjective refraction, corneal topography (Alcon Eyemap) and biomicroscopy.
Once we determined that patients were candidates, we fit each eligible eye with an 8.3mm base curve silicone hydrogel lens (Acuvue Advance, Vistakon). After evaluating the fit of this soft lens, we applied each patient's own GP lens on top. To achieve a successful piggyback fitting relationship between the GP lens and the soft lens, the first variable that we adjusted, if necessary, was the power of the soft lens. Our goal was to achieve an acceptable piggyback fit utilizing each patient's own GP lenses.
Plus power soft lenses create a steeper anterior surface and minus power soft lenses create a flatter anterior surface. Thus, we could potentially achieve a successful fit by altering soft lens power. A fit is successful when a well-centered GP lens moves independently of the soft lens with each blink with acceptable visual acuity and absence of corneal compromise. Ideally, the GP lens should achieve three-quarters to 1 millimeter of movement over the soft lens surface with each blink. If the GP lens is too tight and moves less, the potential for central corneal edema increases. The soft contact lens should move one-quarter to one-half of a millimeter with each blink. Additionally, stationary air bubbles trapped between the soft and GP lens that can't be removed — indicating an exceedingly steep GP lens fitting relationship — are unacceptable.
In this study, we determined the optimal soft lens fit by trial and error. If we couldn't achieve a successful fit (as detailed above) by altering soft contact lens power, then we selected a new GP lens. To determine the ideal base curvature of the new GP lens, we performed keratometry over the soft lens. We then used the flat keratometry measurement as the initial base curvature of a diagnostic GP lens. After we determined the base curve through fitting relationship evaluation and calculated the power through over-refraction, we ordered a new GP lens. Table 1 lists the variety of GP materials worn in the study.
The cleaning protocol for the GP lenses included a GP lens cleaning solution (Boston Advance, Bausch & Lomb) and rinsing/storage with a soft lens multi-purpose solution (Opti-Free Express, Alcon). A separate cleaning protocol for the silicone hydrogel soft lenses included Opti-Free Express for disinfecting, rinsing and storage. We instructed patients to use rewetting drops (Blink Contacts, AMO) as needed.
|
|
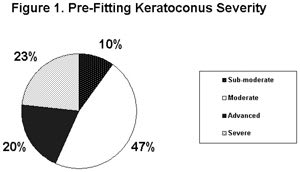
| Figure 1. Pre-fitting keratoconus severity. |
We instructed patients to return for follow up at one week, wearing the piggyback system for at least three hours before the visit. We evaluated vision, piggyback lens fit and corneal health; if these were acceptable, we scheduled a final evaluation at a minimum of four weeks following the successful fitting. At this last evaluation, we performed visual acuity testing and a slit lamp examination, including a lens fitting evaluation. Additionally, we asked patients to complete a post-fitting questionnaire (Appendix B, available in the online version of the article) to assess wearing time, visual quality and comfort levels with the new piggyback lens system.
We used a paired t-test for with-in group comparisons to assess statistically significant changes in wearing time and visual acuity. To analyze visual acuity data, we converted decimal values to logMAR equivalents.
Results
Piggyback Lens System Fitting Of the 30 eyes of 16 patients included in this study, we achieved successful piggyback fits in 26 eyes of 14 patients (87 percent). We excluded two eyes of the 14 successful patients because one eye wore soft contact lenses alone and the other eye did not wear any contact lens due to a history of corneal hydrops with secondary advanced scarring. Of the 26 successful piggyback fits, we achieved 20 using the patients' own GP lenses (77 percent).
Despite good comfort and fit with the piggyback lens system, three of the successfully fit patients (six eyes) dropped out of the study before the one-month follow up due to loss of interest. Of the 30 eyes included in this study, we couldn't achieve a successful piggyback fit in four eyes (13 percent) of two patients. In one of these patients who had advanced keratoconus, the silicone hydrogel base curve (8.3mm) wasn't steep enough to fit the cornea properly. In the other unsuccessful patient, despite numerous attempts with a variety of GP parameters, persistent stationary central air bubbles remained between the soft silicone hydrogel lens and GP lens.
|
|
|
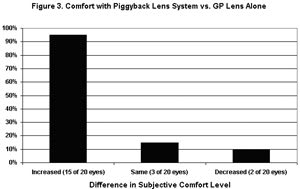
Figure 2. Comfort with piggyback lens system vs. GP lens alone. |
Corneal Health We conducted a thorough slit lamp examination of the anterior segment and more specifically the cornea before the piggyback fitting to assess baseline corneal health. The distribution of clinical findings in keratoconic eyes in this study included seven subclinical eyes (23 percent), nine eyes with Fleischer's rings and absence of striae/scarring (30 percent), one eye with striae, a Fleischer's ring and absence of scarring (3 percent), and 13 eyes with striae, Fleischer's rings and various degrees of scarring (43 percent). Subclinical keratoconic eyes exhibited classic topographical patterns in the absence of visible corneal findings.
To compare severity, Heyman (1967) categorized keratoconic eyes using keratometry readings, with moderate eyes ranging from 48D to 52D, advanced eyes from 52D to 56D and severe eyes from 56D to 60D. Based on this classification system, Figure 1 shows the severity of keratoconus in eyes included in this study: Three eyes with sub-moderate keratometric readings, 14 eyes with moderate keratometric readings (47 percent), six eyes with advanced keratometric readings (20 percent) and seven with severe keratometric readings (23 percent).
All 30 eligible eyes exhibited an absence of significant corneal compromise and complications throughout the piggyback fitting process and one-month follow-up period. Additionally, we found no evidence of hypoxia throughout the study. We noted sodium fluorescein staining in 28 of 30 (93 percent) eyes prior to the piggyback lens fitting. A large concentration of staining in eyes wearing only GP lenses was located in the typical 3 o'clock and 9 o'clock positions, with grade 3 staining in one eye (3 percent), grade 2 staining in three eyes and grade 1 staining in 18 eyes. Prior to the piggyback fitting, central sodium fluorescein staining appeared in 11 eyes (37 percent) with grade 1 staining in nine eyes and grade 2 staining in two eyes.
Before the piggyback lens fitting, 18 of the 20 eyes successfully fit in piggyback systems demonstrated 3 o'clock and 9 o'clock staining with an average grading of 1 and six of the 20 eyes (30 percent) showed central staining with an average grading of 1. One month after the successful piggyback fittings, only two of these 20 eyes showed 3 o'clock and 9 o'clock staining with an average grading of 1, and we noted no central staining.
Comfort Figure 2 compares subjective comfort after wearing the piggyback lens system for one month vs. prior GP lens wear alone. Eighteen of the 20 (90 percent) eyes successfully fit with a piggyback lens system had the same or improved comfort compared to previous GP lens wear alone. Using a scale of 1 to 10 on the patient questionnaires, the mean subjective comfort rating improved to 8.95 one month after the piggyback fitting from the 8.00 mean rating prior to piggyback fitting.
|
|
|
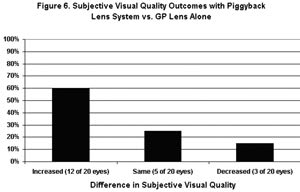
Figure 3. Subjective visual quality outcomes with piggyback lens system vs. GP lens alone. |
Wearing Time All 20 eyes successfully fit with a piggyback system had the same or increased wearing time vs. the GP lens worn alone. The mean wearing time reported before the piggyback fitting was 13.1 hours vs. a mean wearing time of 13.4 hours one month after the piggyback fitting, which is not statistically significant (p=0.21).
Visual Outcomes Seventeen (85 percent) of these eyes fit with piggyback lens systems experienced the same or better Snellen visual acuity. Figure 3 compares subjective visual satisfaction one month after successfully wearing the piggyback lens system. Seventeen of 20 eyes (85 percent) had improved visual quality with the piggyback lens system vs. their previous GP lens alone. Using a scale of 1 to 10 on the patient questionnaires, the mean pre-fitting subjective visual quality rating was 8.05, which improved to a 9.00 mean visual quality rating one month after the piggyback fitting.
Handling and Care While 12 of 20 (60 percent) eyes reported more difficulty and inconvenience with handling a piggyback lens system, six of these 12 eyes reported that other benefits associated with the piggyback lens system outweighed this potential disadvantage. Using a scale of 1 to 5 on the patient questionnaires, the mean convenience rating decreased from 4.05 before the piggyback fitting to 3.65 one month after the piggyback fitting.
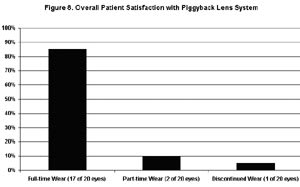
Overall Patient Satisfaction Figure 4 compares overall patient satisfaction with the piggyback lens system vs. prior GP lens wear alone. Only one of the 20 successful piggyback fits that completed the one-month follow-up felt that the piggyback lens system was worse than wearing the GP lens alone. After the one-month follow up, 17 of 20 (85 percent) eyes continued with full-time piggyback lens wear. Two eyes of one patient continued with part-time piggyback lens wear after the study. One patient continued with GP lenses alone in one eye and full-time piggyback lens wear in the other eye.
|
|
| Figure 4. Overall patient satisfaction with piggyback lens system. |
Discussion
With limited vision correction alternatives for keratoconus, piggyback lens systems have evolved into a viable option for a wide range of keratoconic patients. Using the methods described, it's possible for practitioners to improve vision and comfort for many problematic keratoconic patients by simply introducing a soft silicone hydrogel lens beneath their existing GP lens.
One of the most important outcomes of the successful piggyback lens system fittings was the resolution of many previous complications, including central and peripheral superficial punctate keratitis. Improved corneal health with a significant reduction of sodium fluorescein staining occurs because the soft contact lens provides a cushioning or bandage effect from the overlying GP lens. The soft lens covers the entire cornea, minimizing abrasions of the fragile cone apex and peripheral corneal tissue.
In this study, it appears that a variety of GP lens materials in combination with a higher-Dk silicone hydrogel contact lens sufficiently eliminated hypoxic complications. Researchers must attempt longer-term follow up and more material combinations to confirm this finding.
Between 10 percent and 25 percent of keratoconic patients undergo a penetrating keratoplasty because of lens intolerance, reduced vision and/or corneal compromise. By increasing comfort, wearing time and vision while decreasing corneal compromise, a piggyback system may delay or prevent the need for a penetrating keratoplasty.
We can attribute improved comfort and increased wearing time with the piggyback system to a lack of significant GP decentration or excessive GP lens movement. Kok et al (1993) found that in 80 percent of eyes, patients wore piggyback systems longer than 12 hours per day without discomfort. Decreased mechanical irritation and pressure on the weakened corneal apex allows keratoconic piggyback lens wearers longer wearing times without comfort difficulties.
Improved subjective visual quality and objective visual acuity with a piggyback lens system is yet another advantage for keratoconic patients. The soft contact lens effectively masks some of the irregularity of the corneal surface. This enables the GP lens to more effectively correct the remaining irregular astigmatism common in keratoconic eyes.
Despite the advantages this study found with piggyback lens systems, many patients found the care and handling necessary to maintain the lenses inconvenient. In addition to the need for handling two different types of lenses for each eye, patients must use two different care systems to optimally disinfect each lens type. Because of this time-consuming care process, several patients successfully fit with piggyback lens systems dropped out of this study. One commonality among all of these patients was an absence of comfort and vision problems associated with wearing their habitual GP lenses alone. Symptomatic patients may be more receptive to the potential increased comfort and visual quality of the piggyback lens system.
Promising Option for Problematic Patients
As reported in this study, it's often possible to achieve a successful piggyback lens fitting utilizing a patient's own GP lens. The relative ease of completing this piggyback fitting allows you more corrective options in managing keratoconic patients. With proper patient selection, the advantages of increased comfort, wearing time and visual quality can outweigh the inconvenience associated with handling and caring for two sets of lenses. Tsubota et al (1994) reported that 10 of 11 patients who had keratoconus and weren't able to tolerate hard lenses were successful in avoiding surgical intervention by switching to a piggyback system. By fitting piggyback systems using new higher-Dk GP and soft lens materials, you may help symptomatic keratoconic patients delay or avoid the long recovery period and other complications often associated with a penetrating keratoplasty.
For references, please visit www.clspectrum.com/references.asp and click on document #130.
Dr. Rodio-Vivadelli graduated from State University of New York College of Optometry in 2004, then completed a fellowship program in cornea and contact lenses in New York City, which provided advanced training in specialty contact lens fitting and refractive surgery. She currently lives in Hammonton, NJ, and practices in the area.
Dr. Gundel is an associate clinical professor and director of the Cornea and Contact Lens Fellowship Program at SUNY State College of Optometry, New York, NY.