LENS-RELATED DRY EYE
The
Latest Research and Treatment Options for Lens-Related Dry Eye
Recent studies shed light on what's new and
what's on the horizon for managing lens-related dry eye.

We can't seem to get away from dry eye. With up to 12 million North Americans experiencing the disorder and more than 25 percent of contact lens wearers experiencing dry eye symptoms, there's been a push for new treatments, improved diagnostic techniques and new theories on dry eye etiology.

Something Old, Something New
Over the last 15 years, research in the area of dry eye with and without contact lenses has significantly increased, largely driven by the report of the National Eye Institute and Industry workshop on clinical trials in dry eye (Lemp, 1995). This workshop attempted to systematically define dry eye, to set forth a classification scheme for different types of dry eye and to recommend diagnostic criteria for the diagnosis of dry eye for clinical researchers. While the workshop provided a framework for the study of dry eye, the report highlighted many areas in which knowledge about dry eye, including contact lens-related dry eye, was lacking.
|
|
|
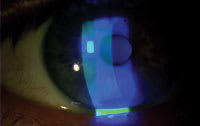
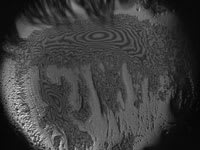
Figure 1. Does reduced tear break-up time demonstrate "dysfunctional tear film"? |
Two groups, the Delphi Panel and the Dry Eye Workshop (DEWS), recently assembled expert clinicians and researchers to redefine and reach consensus regarding dry eye treatment, the status of the field and emerging research directions. The pending peer-reviewed reports of these two groups will provide the most comprehensive overview of dry eye in terms of research and of treating patients.
The NEI/Industry report set forth a definition of dry eye as follows: "Dry eye is a disorder of the tear film due to tear deficiency or excessive tear evaporation which causes damage to the interpalpebral ocular surface and is associated with symptoms of ocular discomfort." This is somewhat different from the term "Dysfunctional Tear Film," developed by the Delphi Panel. This term, while different from "Dry Eye Syndrome," is more encompassing and supports the common notion that some characteristic unifies all the sub-categories of dry eye (Figure 1).
Symptoms in Contact Lens Patients
We've all had patients for whom the dry eye symptoms outweigh the abnormal ocular signs. In contrast, some severe dry eye patients who have significant surface damage report symptoms that don't seem to correlate with the clinical signs. Regardless of the severity of the disorder, asking the appropriate dry eye questions can assist you in monitoring change in the disorder over time or with treatment.
|
|
|
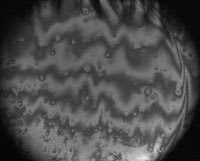
Figure 2a. In-vivo OSU interferometric images of PLTF (roughly 8mm surface). |
|
| Figure 2b. Unlike 2a (stable PLTF after blink), this image shows few fringes, and much of the lens surface is exposed. |
In general, contact lens wearers report more ocular symptoms than do non-contact lens wearing patients. Both groups report symptoms of dryness, soreness, grittiness, light sensitivity, pain or itching. Contact lens wearers typically report increased ocular dryness compared to non-lens wearers, and their complaints of dryness often increase with daily wearing time.
In addition, patients frequently cite complaints of dryness as reasons for discontinuing lens wear. Prichard and coworkers (1999) found that after 5 ±6 years of lens wear, 12 percent of contact lens patients discontinued contact lens wear permanently, primarily due to discomfort (49 percent) and dryness (9 percent) symptoms. Schlanger (1993) surveyed 199 individuals who had discontinued contact lens wear and again showed the most common reason for lens discontinuation was discomfort (72 percent of individuals cited this reason). In addition, patients who undergo refitting because of dryness complaints are more likely to discontinue lens wear altogether.
We know little about factors other than symptoms (such as demographics, differences in lens types, etc.) associated with lens discontinuation. Why do certain patients tolerate uncomfortable lens wear while others seek refractive surgery? Why do some patients find contact lens wear too inconvenient (solutions, drops, out-of-pocket costs)? Few studies to date have examined differences in patient factors when comparing self-perceived satisfied current lens wearers with self-perceived dissatisfied current wearers. At the 2005 American Academy of Optometry annual meeting, Nichols et al presented data demonstrating that in patients reporting current or previous experience with contact lenses, 26.3 percent reported that contact lenses weren't the ideal form of visual correction for them (contact lens dissatisfaction) and 24.1 percent had permanently discontinued contact lens wear. Previous lens wearers were more likely than current lens wearers to be male, to be older, to have started contact lens wear at a later age and to have tried either rigid or both soft and rigid lenses. The primary self-reported reason for both contact lens dissatisfaction and discontinuation was ocular symptoms (dryness and discomfort) followed by preference for another corrective modality.
Factors Associated with Lens-related Dry Eye
Nichols and Sinnott (2006) showed that several factors are related to contact lens-related dry eye status, including female gender, lenses with higher nominal water content, rapid pre-lens tear film thinning time, frequent usage of over-the-counter pain medication, limbal injection and increased tear film osmolality. While some of this is common sense and well accepted, some findings, including the increased tear film osmolality and rapid tear film thinning, suggest potential mechanisms for dry eye in contact lens wearers.
Osmolality has often been touted as a gold standard test for dry eye, and this study is the first to confirm higher osmolality in lens-related dry eye using a new generation, small sample tear osmometer.
In summary, monitoring changes in lens comfort, particularly in female patients wearing high-water contact lenses, may help prevent this group from contact lens dropout.
Contact Lens and Tear Film Interactions
|
|
|
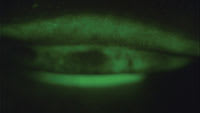
Figure 3. Superior lid staining with fluorescein. |
The stability of the tear film during contact lens wear depends on the surface chemistry of the lens and its physical interactions with each layer of the tear film. The superficial lipid layer prevents evaporation of the tear film, which helps maintain lens hydration in contact lens wearers. In general, the pre-lens tear film (PLTF) provides comfort and lubrication to the conjunctiva, especially during the blink, in addition to providing a smooth optical surface. An irregular PLTF, similar to what happens during the dewetting or evaporative process, results in light scatter and reduced visual acuity, especially in low contrast situations. This finding is consistent with clinical reports and symptom research findings describing changing or fluctuating vision which may clear with a blink (Begley et al, 2001).
The past several years have brought the development of optical techniques to investigate tear film thickness and stability, including interferometric analysis (King-Smith et al, 2000, 2006; Goto et al, 2004), OCT analysis (Wang et al, 2003) and methods of quantitatively evaluating tear film breakup dynamics (Begley et al, 2006). Figure 2 illustrates the process of PLTF dewetting and breakup on the surface of a hydrogel lens using imaging interferometry techniques.
Diagnostic Advances
It's been a unique challenge to improve our ability to diagnose contact lens-related dry eye beyond symptomatology. Many of the diagnostic tests have existed for many years, and we've largely performed them without change. Recent advances in real-time digital video assessment of tear film break-up patterns and interferometric techniques have not reached a level to which the technology is commercially available.
|
|
|
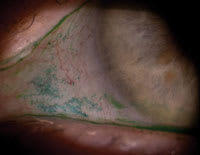
Figure 4. Conjunctival lissamine green staining in a symptomatic lens wearer. |
What's new in this area? Over the past few years, Korb et al coined the term "lid wiper epitheliopathy" (Figure 3) to represent staining of the anterior superior tarsal conjunctiva, which is highly associated with symptomatic contact lens wear. To evaluate this staining, instill fluorescein and lissamine green in the eye in a sufficient quantity to cover the ocular surface. Then evert the superior lid and evaluate for staining. Grade the horizontal length and the width of the staining, with a grade 2 representing approximately 50 percent staining of the "lid wiper" area (a staining pattern of approximately 6mm x 1mm coverage). Although studies using different treatment regimens haven't utilized this as an outcome measure, if you do see this staining pattern in symptomatic patients, you should monitor it for possible improvement with changes in the management plan.
Along the lines of using vital dyes, lissamine green has essentially replaced rose bengal dye in clinical practice. In evaluating contact lens-related dry eye, lissamine green assessment of conjunctival staining is often the most significant abnormal finding and can be very dramatic (Figure 4). You can also monitor this staining for improvement with treatment.
Don't Change Everything at Once
It's often more successful to take a step-wise approach to managing contact lens-related dry eye patients rather than changing several components simultaneously. Such an approach may involve changes to lens materials, wearing schedules, replacement frequency, solutions and rewetting drops, as well as punctal occlusion and pharmacological intervention. Since the approval of cyclosporine A (Restasis, Allergan) and with the advent of several good lubricating eye drops for treating dry eye, contact lens management strategies have moved away from multiple contact lens refittings or only changes in solution use.
|
TABLE 1 |
||
|
Studies of Dry Eye Symptoms During Lens Wear |
||
|
STUDY |
SAMPLE |
FREQUENCY
OF CL/DE SYMPTOMS |
| Brennan, et al (1989) | 104 | 75% |
| Guillon, et al (1997) | 184 | 44% |
| Doughty, et al (1997) | 3285 | 50% |
| Vajdic, et al (1999) | 171 | 73% |
| Begley, et al (2000) | 83 | 50% |
| Nichols, et al (2005) | 893 | 52% |
In addition, the popularity of silicone hydrogel lens materials has changed initial and refitting patterns, leading many practitioners to fit dry eye patients with silicone hydrogel lenses. Peer-reviewed data supporting increased comfort with silicone hydrogel lenses in contact lens-related dry eye patients is limited. Manufacturers continue to market both hydrogel and silicone hydrogel lenses for patients who have dryness symptoms, such as Acuvue Oasys (Vistakon), Proclear Compatibles (CooperVision) and Extreme H2O (Hydrogel Vision Corp.). Future studies are needed to determine whether changing to a different lens material or changing the lens mater-ial/solution combination is more effective in managing dryness.
Studies have demonstrated that pre-lubrication of the ocular surface with a lubricant eye drop before applying a contact lens may increase the comfortable lens wearing time. The use of cyclosporine A in contact lens patients before lens application and after lens removal can also significantly increase comfortable wearing time. Studies in this area have been relatively small, and we need larger-scale studies that control for additional factors such as additional rewetting drop/artificial tear usage, contact lens material, age of lens, solutions and associated patient factors.
Management strategies for contact lens wearers are the same as those for non-wearing dry eye patients, with the caveat that patients who can wear lenses are most likely not in the severe dry eye diagnosis/management category. However, you will occasionally see a patient who has significant dry eye and extremely high motivation to wear contact lenses. In these cases, the typical management strategy fails. Adding omega fatty acid supplementation (recommended dose ~2g per day), lid massage and warm compresses and/or tetracycline/doxycycline, in addition to cyclosporine, are clinically recommended to ensure adequate management of any concurrent lid disease. Clinical evidence and scientific studies in this area are beginning to support improvement on the basis of this management strategy, which will continue to undergo evaluation in ongoing and future ocular surface research.
Team Players in the Future
Future recommendations for contact lens wearers who have symptoms of dryness may include the pairing of specific solutions and materials to maximize comfort and vision with lens wear. Proteomic and lipidomic studies to investigate changes in tear film composition and lipid and protein deposition on contact lenses in well-defined groups of patients may lead to customized lens/lens care approaches through the development of biomarkers to diagnose and monitor changes in dry eye disease. Current and anticipated advances in technology related to contact lenses will change practitioner patterns in the next decade, and with those changes will come the opportunity to reduce the rate of contact lens dropout and improve the practice of contact lenses.
To obtain references for this article, please visit http://www.clspectrum.com/references.asp and click on document #130.
Dr. Kelly Nichols is an associate professor at The Ohio State University College of Optometry focused on the area of dry eye research.
Dr. Jason Nichols is an assistant professor of optometry and vision science at The Ohio State University College of Optometry.