CONTINUING
EDUCATION
No
Fee Required
Intraocular Lens Update
Intraocular lens implantation for patients who have cataracts is common and usually successful. Improved aphakic IOLs have led to a revitalization of IOLs for non-cataractous patients because many aphakic IOL designs and surgical procedures are also applicable for phakic IOLs. Refractive surgery now encompasses corneal refractive surgery, aphakic IOLs and phakic IOLs. This article will discuss the various designs, procedures and applications of aphakic and phakic IOLs as well as complications, clear lens extraction and intracorneal implants.
Aphakic IOLs
Some milestone events have occurred in the evolution of aphakic IOLs. In 1949 the first IOL implant on a human was performed using a lens made from polymethylmethacrylate (PMMA). The surgeon placed the IOL in the posterior chamber after extracapsular cataract extraction (ECCE). Many problems from both the lens design and placement location ensued. For the next two decades, attempts to find a better fixation location included anterior chamber (AC), iris and iridocapsular placement. All of these were more problematic than the posterior chamber (PC) fixation, so this became the preferred position and many subsequent refinements have brought it to its present status.
An important development in 1967 was the phacoemulsification and aspiration procedure, which allowed a small incision and control for cataract removal. Unfortunately, because of the existing IOL design and PMMA material, the incision had to be enlarged for IOL insertion. There have been many improvements of phaco over the years.
In 1977 an IOL with flexible posterior haptics became available. Subsequent developments allowed for placement in the capsular bag. Combining the concepts of intracapsular phaco and IOL capsular bag fixation eventually led to today's minimally compression-resistant posterior chamber IOL (PCIOL) with short haptic configuration.
1980 brought the introduction of viscoelastic 1% sodium hyaluro-nate (Healon), which protected the corneal endothelium during IOL implantation and also made it easier to perform anterior capsulotomy. This was followed in 1984 by the first foldable silicone IOL. Manufacturers improved both the design and material, and in 1992 came the introduction of a procedure involving only a 3mm-wide, self-sealing, clear corneal incision that could accommodate phaco and IOL insertion. Now surgeons could implant silicone foldable IOLs without the need for cautery, scissors or sutures, although one suture is sometimes used.
In 1992 cataract surgery with only topical anesthetic was introduced and then improved with the addition of intracameral anesthesia. In 1995 the soft, foldable acrylic IOL received Food and Drug Administration (FDA) approval for use in the United States.
There are several dozen IOL manufacturers and almost a thousand variations of IOLs, but a majority of surgeons use silicone or acrylate foldable IOLs, temporal clear corneal incisions of about 3mm, topical-intracameral anesthesia and adjunctive viscoelastic solution.
IOL Materials
The four basic categories of IOL materials are PMMA, acrylic, acrylic hydrogel and silicone.
PMMA is a good IOL material, but it can cause mechanical irritation and inflammation and it requires a larger incision for implantation, which can cause intraoperative complications and delay postoperative healing. Because small-incision surgery and phacoemulsification are desirable, rigid IOL materials are less preferable.
Pure acrylics are soft, hydrophobic and mechanically weak. Copolymerization with methacrylates can maintain the flexibility of the acrylate and increase mechanical strength. Acrylates have a hydrogen group that, when replaced by a methyl group, creates a methylacryate, which can be copolymerized with other mono-mers such as PMMA and Poly-HEMA. A wide range of properties can be produced with various tensile strength, elongation and softness.
Hydrogels are hydrophilic and can be copolymerized with a variety of monomers to produce desired properties. For IOL materials, acrylate and methacrylate-based materials are most commonly used with hydrogels.
Medical grade silicone polymers have been used for drains in glaucoma surgery, scleral buckles and oculoplastic surgery as well as in IOLs.
Injectable IOL materials are under investigation.
About 25 percent of U.S. ophthalmic surgeons prefer silicone foldable IOLs, but about twice this number prefer acrylic foldable IOLs. Examples of silicone foldable IOLs are RMX3 (Staar Surgical) and SLM2 (Allergan), and of acrylic foldables are Acrysof (Alcon) and Sensar (Advanced Medical Optics [AMO], Figure 1).
Special Design Aphakic IOLs
Historically, aphakic IOLs have been spherical, single-vision and with some ultraviolet absorption. Many of the newer IOLs are designed to correct presbyopia, astigmatism, aberrations or to block specific wavelengths of light.
Presbyopia There are optical parallels between presbyopes who wear contact lenses and those who have IOLs. One obvious parallel is that both groups need one power correction for distance and a different one for near. Either group can attain this by correcting both eyes for distance or for near and wearing spectacles (for the opposite vision need) over the contact lenses or IOLs. Alternatively, patients can wear single-vision lenses in a monovision modality.

Another parallel between presbyopic users of contact lenses or IOLs is that some of them would prefer to not need auxiliary spectacles. Although the majority of presbyopic lens wearers do use single-vision lenses (with both eyes corrected for the same distance) with auxiliary spectacles or monovision, an increasing number are using some type of bifocal or multifocal contact lenses because of their improved optical designs.
An additional parallel is that the general optical concepts used for bifocal or multifocal contact lenses (diffraction or refraction) are also used for bifocal or multifocal IOLs. The overall designs of the contact lenses or IOLs both include concentric rings of two or more zones of various optical powers and aspheric progressive (on anterior surface of IOLs) or diffractive (on posterior surface of IOLs) optics.
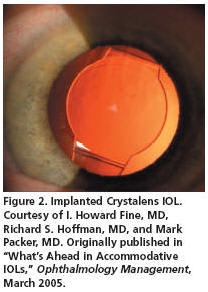
Although manufacturers have developed or are developing many bifocal or multifocal IOLs, the three that have FDA approval for use in the United States are ReZoom (AMO), ReStor (Alcon) and Crystalens (Eyeonics, Figure 2).
The predecessor to ReZoom was Array, which produced glare for many patients. ReZoom's improved refractive optics have decreased this using a five-optical-zone design of concentric rings in which the central zone is for distance and subsequent zones alternate near and distance correction. It also features aspheric transitions between adjacent zones designed for intermediate distance correction. The add power at the corneal plane is about +2.25D.
The ReStor IOL uses special diffractive optics. It has 12 diffractive steps that start with a 1.3μ height and taper to a 0.2μ height for the 12th step. The effective add is about +3.00D.
The Crystalens' optics are monofocal, contrasted to the multifocal optics of ReZoom or ReStor. Crystalens has a hinged-plate haptic that allows the IOL to move forward. When a patient attempts to accommodate, the ciliary body contracts, the tension on the capsular bag decreases and the pressure within the vitreous body produces the IOL's forward motion and near focus with an average add effect of +1.00D to +1.50D.
A final parallel between bifocal or multifocal contact lenses and IOLs is optical disturbances. Practitioners don't have the same variety of adds to prescribe with contact lenses or IOLs as they would have with spectacles. Also, the multi-zoned ReZoom and ReStor cause some light scatter, glare and halos, especially under reduced illumination. Some patients adjust to this better than others. In addition, distance and/or near contrast sensitivity may decrease. Because the Crystalens is monofocal, it's less likely to produce glare, halos or decreased contrast sensitivity.
Astigmatism Small-incision procedures have minimized surgically induced corneal astigmatism. Surgeons can correct some pre-existing corneal astigmatism using limbal relaxing incisions, using peripheral intralimbal arcuate relaxing incisions, by rotating the basic cataract incision to the steep axis or a combination of these. But the efficacy varies, and the development of toric IOLs is geared toward a more consistent efficacy without surgically weakening the cornea and increasing higher-order aberrations (HOAs).
To accurately correct pre-existing corneal astigmatism with a toric IOL, the IOL must be positionally stable in the capsular bag, the surgeon must place the IOL at the correct axis during surgery and there should be no surgically induced corneal astigmatism.
The front-surface toric Staar Surgical Toric IOL is a single-piece silicone IOL whose plate haptics have large holes to lock and stabilize the IOL in the capsular bag by migrating epithelial cells. It has linear axis marks on the front surface's periphery for axis alignment. A range of spherical powers are available as well as labeled cylinder powers of 2.00D and 3.50D, which after implantation respectively have an effect of about 1.40D and 2.30D.
Another method to correct higher amounts of post-operative corneal astigmatism is LASIK. Of course, spectacles with the appropriate cylindrical correction is an easy option.
Aspheric IOLs Even in healthy eyes, contrast sensitivity decreases with age, which decreases functional vision probably due to changes of the crystalline lens' spherical aberration. That is, the young crystalline lens' negative spherical aberration changes so that it reduces the older crystalline lens' compensation for the positive spherical aberration of the cornea. Consequently, retinal image quality decreases. Conventional spherical IOLs have positive spherical aberration. This adds to the cornea's positive spherical aberration, which increases spherical aberration.
The goal of aspheric IOLs is to improve functional vision and contrast sensitivity by a lens design that induces negative spherical aberration to help offset the cor-nea's positive spherical aberration. Three aspheric IOLs have FDA approval: AcrySof IQ (Alcon), SofPort LI61AO (Bausch & Lomb) and Tecnis Z 9000 (AMO).
The pre-surgical average corneal spherical aberration is +0.25μ; the AcrySof and SofPort add –0.15μ spherical aberration and the Tecnis –0.27μ. Ophthalmic surgeons can measure a patient's pre-operative corneal spherical aberration and choose the aspheric IOL that will best help offset it. The goal is to leave the patient with about +0.10μ, which seems to produce the best contrast sensitivity and functional vision including for night driving.
However, the pre-operative cornea doesn't always have the same amount of spherical aberration as the post-operative cornea. Surgery and incisions can induce HOAs such as coma. In the future more options may be available in the IOLs' negative spherical aberration range, which would allow greater customization.
Another technology is Calhoun Vision's light adjustable lens. This silicone IOL with photosensitive material uses wavefront sensing and can be adjusted after implantation to correct refractive errors and perhaps coma and spherical aberration. This lens is a foldable three-piece IOL with a cross-linked photosensitive silicone polymer matrix, a homogeneously embedded photosensitive macro-mer and a photo initiator. Irradiation of various areas of the lens can change spherical and toric power and perhaps reduce or eliminate HOAs.
Wavelength Blockage All IOLs block some UV light, but blue-light absorbing IOLs are also available. Studies are ongoing to determine which type of absorption provides the best retinal protection as well as the best visual performance under photopic and mesopic lighting conditions. AcrySof Natural (Alcon, Figure 3) blocks both UV and blue lights.
IOL Surgery Complications
Contemporary IOL surgery is a very common procedure that usually produces good results. However, complications can occur ranging from optical deficiencies to anterior or posterior segment problems. Many of these have a low incidence and/or can be managed.
The most common cause of IOL decentration occurs when a surgeon inserts the inferior haptic into the capsular bag and the superior haptic into the ciliary sulcus, which causes upward movement of the IOL optic. Superior migration of PCIOLs produces the "sunrise syndrome" while inferior migration produces the "sunset syndrome."
Pupillary capture occurs when some or all of the optic is within the pupil and the rest of the lens is behind the iris. It usually occurs one to two months postoperatively, and the incidence with silicone or acrylic foldable lenses is very low.
Anterior chamber inflammation and persistent iritis in patients after ECCE and PCIOL implantation probably averages about 2 percent. It results from the breakdown of the blood-aqueous barrier.
Uveitis-glaucoma-hyphema (UGH) more commonly occurs with anterior chamber IOLs (ACIOLs), but it occasionally occurs with PCIOLs. It's a rare complication and results from mechanical trauma on the angle or iris. Pupillary block glaucoma results when the IOL blocks aqueous flow through the pupil. Malignant glaucoma occurs when anterior aqueous flow is misdirected posteriorly.
Pseudoaphakic bullous keratopathy relates to progressive endothelial loss. It has a greater incidence with ACIOLs and iris-fixated IOLs, but less than 1 percent with ECCE and PCIOLs.

The crystalline lens' epithelium exists on the surface of the anterior lens capsule (where A-cells are located) and on the surface of the capsule at the equator (where E-cells are located). Anterior subcapsular opacities with some aphakic PCIOLs result from A-cell proliferation. E-cells are primarily responsible for "secondary cataract" (posterior capsular opacification, or PCO) after ECCE and IOL placement "in the bag." Cells proliferate and migrate onto the central region of the posterior capsule.
Anterior capsule opacification (ACO) usually occurs within a month or so after cataract surgery. It occurs along the anterior rim of the capsular bag, and its peripheral location away from the major portion of the anterior surface of the PCIOL has little effect on vision.
PCO clinically manifests as fibrous membrane and Elsching pearls. Typically the fibrous opacity develops two to six months postoperatively and is more common with silicone IOLs, while the Elsching pearls can develop several months to years after surgery and are more common with PMMA IOLs. Although various studies show different results, it seems that about 50 percent of patients who have ECCE/IOL will need neodymiumiyttrium-aluminum garnet (Nd:YAG) laser capsulotomy within four years postoperatively. The rates are believed to be lower with acrylic IOLs.
Posterior capsulotomy has a four times higher risk of developing retinal detachment (RD), probably because of loss of hyaluronic acid from the vitreous, its destabilization and disruptions in the vitreoretinal interface. Surgeons may reduce the incidence of PCO by intraoperative polishing of the posterior capsule and/or present day acrylic or silicone IOLs.
Cystoid macular edema (CME) is another common complication. Although estimates vary, with ECCE incidence of angiographic evidence is about 15 percent but clinically symptomatic CME is only about 2 percent. CME typically appears one to three months after surgery, but infrequently can occur months or years later. Usually it resolves spontaneously, but about 1 percent of cases are chronic and last more than six months. Use of ketotolac tromethamine both pre- and post operatively significantly decreases both angiographic and symptomatic vision problems of CME.
Phacoemulsification can cause dislocated crystalline lens fragments into the vitreous cavity. Surgeons can reduce the chance of this happening by using the lowest possible vacuum and power settings and infusion pressures. Dislocation of the IOL itself into the vitreous is quite rare.
RD after ECCE has a less than 1 percent incidence, much less than after ICCE. RDs usually occur within six months postoperatively, but pseudoaphakia increases the risk of RD even six years later. Major risk factors for postoperative RD are pre-operative conditions such as high myopia (eight times higher risk), retinal lattice degeneration (10 times higher risk), family history of RD and hereditary vitreoretinal degeneration. Intraoperative factors that predispose to RD include crystalline lens fragments, disruption of the posterior capsule (13 times higher risk) and Nd:YAG laser capsulotomy (four times higher risk). Postoperative ocular trauma also produces a four times relative risk increase. Retinal breaks in pseudoaphakic RD are often anterior near the vitreous base and therefore more difficult to detect.
Secondary IOLs Some patients are aphakic because of ICCE. Options for correction include spectacles or contact lenses, but there are patients who can't or won't use them and for whom secondary IOLs are a consideration. Placement of secondary IOLs may be in the anterior chamber on the iris, or in the posterior chamber with bag and sulcus fixation or sulcus suture fixation. Modern IOL designs and surgical procedures have somewhat reduced complications.
Phakic IOLs
Phakic IOLs aren't new. In 1983 there was a report of a phakic IOL implanted in the anterior chamber (AC) using the irido-corneal angle for support. Over the next decade, a number of phakic lens designs were developed and implanted, with little success because of designs that used solid materials with thick peripheries and because of challenging surgical technique. This produced a negative reaction among the ophthalmic professions and regulatory agencies that resulted in little phakic IOL use and development. In the mid-1980s, manufacturers developed newer and better-designed phakic IOLs. Combined with advances in aphakic IOL surgery that could be applied to phakic IOL implantation, a rebirth of interest resulted because of significantly improved results. Phakic IOLs are categorized by their location in the eye: AC angle-fixated, iris-supported and PC. Worldwide there are a fairly large number of various phakic IOLs in use, but fewer in the United States have received FDA approval. Most of the knowledge about phakic IOLs has been gathered by use and studies outside of the United States and from FDA-related clinical studies in the United States. Predominant phakic IOLs used worldwide include the Verisyse/Artisan (AMO) and the Implantable Collamer Lens (ICL, Staar Surgical) (Table 1).

Phakic IOLs and Corneal Refractive Surgery Improved phakic IOLs offer another option for refractive surgery. Corneal refractive surgery is probably preferable for low and moderate myopia because LASIK and its variants of laser subepithelial keratectomy (LASEK or Epi-LASEK) generally produce good comfort, quick recovery and stable results. However, efficacy and predictability decrease with high myopia. Similarly, LASIK and conductive keratoplasty (CK) are more effective in treating low hyperopia than high myopia. Thus, phakic IOLs may be preferable for myopia greater than about 10.00D and hyperopia greater than about 3.00D. Also note that phakic IOL implantation is reversible.
Bioptics In this context, bioptic simply means the use of more than one type of refractive surgery in two different planes for the same eye. One example is a phakic IOL to correct a spherical error and subsequent LASIK to correct corneal astigmatism. Or for very high myopes or hyperopes, correcting some of the spherical refractive error with a phakic IOL and the rest with LASIK (in cases in which the refractive error is too great for safe and effective correction by LASIK alone).
Anterior Chamber Considerations In addition to the degree of refractive error, other considerations for phakic IOLs could include stable refraction coupled with a patient's inability or disinterest in wearing contact lenses. Phakic ACIOLs (PACIOLs) occupy space, so the anterior chamber depth needs to be great enough (at least 3.4mm) to have the phakic IOL and maintain sufficient separation from the corneal endothelium (which should have a cell count of at least 2,250 cells/mm2). This ensures that the PACIOL causes no mechanical trauma to the corneal endothelium.
An accurate measurement of the anterior chamber is essential with PACIOLs. Ultrasound scans, the IOL Master (Carl Zeiss Meditec) and the Orbscan II (B&L) are traditionally used. Three newer instruments for measuring AC depth are the Pentacam (Oculus), Vosante OCT (Carl Zeiss Meditec) and Artemis #2 (Ultralink).
Phakic PCIOLs were originally developed because of concerns about PACIOLs contacting the cornea and also creating an ovalization of some pupils. Because the phakic PCIOL is positioned between the back of the iris and the front of the crystalline lens, there is some concern about mechanically induced cataracts.
Phakic IOLs and Trends The Verisyse Phakic IOL (AMO) is an FDA-approved iris-fixated PACIOL. It's a one-piece compression-molded PMMA lens with a length of 8.5mm and an optic diameter of 5mm or 6mm. Available powers are –3.00D to –23.50D.
The Visian Toric ICL (Staar Surgical) is a phakic PCIOL made of a proprietary UV-blocking porcine collagen/poly-HEMA copolymer. Powers are –6.00D to –16.50D.
The AcrySof is an angle-supported, foldable PACIOL. Powers are –6.00D to –16.50D.
These three phakic IOLs are comparable in some ways with aphakic IOL development. For example, for implantation the Verisyse PMMA lens needs a large incision and three to six sutures. Large incisions delay visual rehabilitation and have more potential for wound leaks and infection than small incisions, just as for similar aphakic IOL configurations. The foldability of the AcrySof phakic IOL is in line with the need for and development of foldable aphakic IOLs, and the Visian Toric ICL follows the same path as the development of toric aphakic IOLs. Not only are there aphakic and phakic IOLs to correct astigmatism, but also to correct presbyopia and spherical aberration and to filter blue light. In essence, many of the advancements in lens materials, lens design, optics and surgical procedure developed over the years for aphakic IOLs have been applied to phakic IOLs.
The present risk-to-benefit ratio makes phakic IOLs a viable alternative to other types of refractive surgery for high ametropia. As the risk-to-benefit ratio improves with better phakic IOLs and surgical procedures, the use of phakic IOLs may encompass more than the higher ametropias. But as with aphakic IOLs, potential complications exist.
Because of their more recent and limited usage, there are fewer studies in general and particularly fewer long-term studies for phakic compared to aphakic IOLs. Also, as with aphakic IOLs the continuing development and evolution of phakic IOLs and related surgical procedures try to address complications and to minimize or eliminate them. Phakic IOL complications include endothelial cell loss or damage, elevated IOP, pupillary changes, iris alterations, uveitis, RD and cataract formation. The first is more common with ACIOLs and the last with PCIOLs.
IOLs and Clear Lens Extraction
The clear crystalline lens provides high plus power to the eye, and a high myope's eye has excess plus power. Therefore, for over 100 years practitioners have thought about and at times removed a clear, healthy crystalline lens to better balance the axial length and overall power of an eye. Of course, ophthalmic surgeons have to compare the risk-to-benefit ratio of clear lens extraction (CLE) with other procedures for highly myopic patients. The major risk is RD.
As with cataract surgery, CLE has become somewhat more viable because of the use of small self-sealing incisions, phacoemulsification, viscoelastic agents and foldable IOLs. But the risk-to-benefit ratio is better for patients who have cataracts than for patients who have a clear crystalline lens.
Surgeons have also performed CLE for high hyperopes.
Intracorneal Implants
Various intracorneal implants have been tried over the years, but the only inlays now used to a large degree are Intacs (Addition Technology) intrastromal corneal ring segments. Surgeons place these at about two-thirds depth in the peripheral stroma outside the cor-nea's central optic zone. They reshape the anterior corneal surface to reduce or eliminate 1.00D to 3.00D of myopia.
The current design of intracorneal ring segments is two segments each with an arc length of 150 degrees. At the superior end of each segment is a small positioning hole to help the ophthalmic surgeon manipulate the segments after insertion.
Intacs occupy space within the cornea, which forces an anterior corneal curvature flattening. Thicker Intacs occupy more space and create greater anterior corneal flattening and myopia reduction; an increase of about 0.70D of flattening occurs for every 0.05mm increase of device thickness. The available thicknesses in the United States are 0.25mm (predicted correction of –1.03D), 0.30mm (predicted correction of –2.00D) and 0.35mm (predicted correction of –2.75D), with 0.40mm and 0.45mm available elsewhere to correct up to –4.50D.
Addition Technology also received a Humanitarian Device Exemption from the FDA in 2004 to market Intacs for reduction or elimination of myopia and astigmatism in patients who have keratoconus and where functional vision is no longer achievable with contact lenses or eyeglasses.
Conclusion
In only about two decades, vast improvements have occurred in the safety and efficacy of aphakic IOLs and corneal refractive surgery. Many millions of patients receive these procedures each year. Phakic IOLs probably won't experience as dramatic an increase as aphakic IOLs, but phakic IOL usage may increase significantly. CLS
Dr. White is a professor at New England College of Optometry and Continuing Education Editor of Contact Lens Spectrum.
To obtain references for this article, please visit http://www.clspec-trum.com/references.asp and click on document #135.
CONTINUING EDUCATION
Examination Questions
1. The first aphakic IOL implanted was made from:
a. PMMA
b. hydrogel
c. silicone
d. acrylic
2. Phacoemulsification and aspiration was first developed in:
a. 1992
b. 1980
c. 1967
d. 1949
3. U.S. ophthalmic surgeons most use IOLs made of which material?
a. PMMA
b. hydrogel
c. silicone
d. acrylic
4. Which is a silicone foldable aphakic IOL?
a. AcrySof
b. RMX3
c. Sensar
d. Hydroview
5. Which aphakic IOL uses diffractive optics?
a. ReStor
b. ReZoom
c. Crystalens
d. RMX3
6. The effective add of the Crystalens is about:
a. 2.50D to 3.00D
b. 1.75D to 2.25D
c. 1.00D to 1.50D
d. 0.25D to 0.75D
7. Which of these would probably produce the least glare and halos?
a. Crystalens
b. ReStor
c. ReZoom
d. All the same
8. The Staar Surgical Toric ICL's labeled cylinder power of 3.50D has an effective implanted cylinder power of about:
a. 1.40D
b. 2.30D
c. 3.50D
d. 4.50D
9. The average corneal spherical aberration before cataract surgery is about:
a. +0.55μ
b. +0.45μ
c. +0.35μ
d. +0.25μ
10. Which IOL has a photosensitive material and can be adjusted after implantation?
a. AcrySof IQ
b. SofPort LI 61AO
c. Calhoun
d. Tecnis Z 9000
11. Which IOL blocks blue light?
a. AcrySof Natural
b. SofPort
c. Tecnis Z
d. ReZoom
12. Anterior chamber inflammation and iritis after ECCE and PCIOL probably averages about:
a. 2 percent
b. 4 percent
c. 6 percent
d. 8 percent
13. PCO or "secondary cataract" is due to which type of cells?
a. A
b. E
c. H
d. K
14. About what percent of cataractous patients who undergo ECCE and implantation with need Nd:YAG laser capsulotomy within four years postoperatively?
a. 100
b. 75
c. 50
d. 25
15. The fluorescein angiographic incidence of cystoid macular edema with ECCE and aphakic IOLs is about:
a. 35 percent
b. 25 percent
c. 15 percent
d. 5 percent
16. Phakic IOLs may be preferable to corneal refractive surgery for myopes of over:
a. 3.00D
b. 5.00D
c. 7.00D
d. 10.00D
17. Anterior chamber depth for phakic anterior chamber fixated IOLs should be at least:
a. 3.4mm
b. 2.4mm
c. 1.4mm
d. 0.4mm
18. The Verisyse phakic IOL is made of:
a. hydrogel
b. silicone
c. acrylate
d. PMMA
19. The main risk in clear crystalline lens extraction is:
a. retinal detachment
b. iritis
c. cystoid macular edema
d. posterior capsular opacification
20. With Intacs a thickness increase of 0.05mm of the inlay creates about what amount of corneal flattening increase?
a. 0.90D
b. 0.70D
c. 0.50D
d. 0.30D
The following article is offered in conjunction with the
New England
College
of Optometry
INSTRUCTIONS
To obtain credit for this course, you must: 1. Be a licensed optometrist; 2. Read and study the course presented in Spectrum; 3. Complete the test within nine months of the publication date of this issue; 4. Obtain a grade of 70 percent or higher on the exam.
Complete the test by blackening the square that corresponds with your response on the pull-out reply card. Stamp and mail the self-addressed card. Tests must be postmarked by November 30, 2007.
There is no tuition or processing fee to you. The CE section is subsidized by Vistakon to support your professional enhancement. The New England College of Optometry will correct only the optometry tests, notify optometrists of their scores, and issue certificates of credit to those who have passed the test. For information regarding your CE credits and/or certificates, optometrists only can call NEWENCO's Center for Continuing Education at (617) 236-6283. Please allow 12 weeks for processing, which will be done in the order that they are received. You are encouraged to respond early.
STATE BOARD APPROVALS
Each optometry
state board has specific regulations about recognizing
correspondence courses
for continuing education certification (see below). If you have questions about
your particular state, please confirm with your state board. This course has also
been submitted for approval by the Council on Optometric Practitioner Education
(COPE).
This course is supported by an educational grant from VISTAKON®, Division of Johnson & Johnson Vision Care, Inc.
THIS ARTICLE IS APPROVED FOR UP TO 2 CREDITS FOR OPTOMETRY.
Alabama Allows
3 hours per year
Alaska Allows 6 hours correspondence
credit in 2 years renewal
period
Arizona Limit 6 hours of
correspondence credit per 2 years
Arkansas Allows 4 hours
per year
California Allows 20 hours
every 2 years
Colorado Allows 8 hours
every 2 years
Connecticut Does not recognize
correspondence courses
Delaware Allows 2 hours
every 2 years
Dist. of Columbia Allows
6 hours every 2 years
Florida Does not recognize
correspondence courses
Georgia Allows 5 hours
every 2 years
Hawaii Allows 6 hours every
2 years
Idaho Allows 6 hours per
year
Illinois Allows 2 hours
every 2 years
Indiana Allows 2 hours
of credit per article
Iowa Limit 10 hours of
correspondence credit per 2 years
Kansas 1/2 credit per article:
total 3 credit hours per year
Kentucky Does not recognize
correspondence courses
Louisiana Does not recognize
correspondence courses.
Maine State association
only accepts correspondence
Maryland Allows 6 hours
every 2 years
Massachusetts 1/2 credit
per article: total 2 hours per year
Michigan Allows 2 hours
of credit per article
Minnesota Allows
15 hours during each two-year cycle
Mississippi Allows 4 hours
per year
Missouri Allows 2 hours
of credit per article
Montana Limit 6 hours of
correspondence credit per year
Nebraska Allows 2 hours
every 2 years
Nevada Allows 12 hours
in renewal period
New Hampshire Allows 2
hours per article
New Jersey Allows 12 hours
every 2 years
New Mexico Does not recognize
correspondence courses
New York Allows 12 hours
per 3 years (ocular therapy and/or pharmacology only)
North Carolina Limit 4
hours of correspondence credit per year
North Dakota Allows 8 hours
every 3 years
Ohio Allows 10 hours per
year
Oklahoma Allows 10 hours
per year
Oregon Accepts up to 10
hours maximum per biennium
Pennsylvania Allows 6 hours
every 2 years
Rhode Island Allows 2 hours
per year
South Carolina Does not
recognize correspondence courses
South Dakota Allows 6 hours
every 3 years
Tennessee Does not recognize
correspondence courses
Texas Limit 4 hours of
correspondence credit per year
Utah Does not recognize
correspondence courses
Vermont Allows 1 hour per
year
Virginia Allows 2 hours
of credit per article
Washington Allows 10 hours
every 2 years
West Virginia Does not
recognize correspondence courses
Wisconsin Does not allow
correspondence course credit
Wyoming Does not recognize
correspondence courses



