treatment plan
Treating PMD with Contact Lenses
Pellucid marginal degeneration is a corneal degenerative ectasia. Although rare, a prevalence rate for PMD is unknown. It's likely under-diagnosed owing in part to its similarities with keratoconus. It occurs mostly between ages 20 and 40 with no prevalence differences between gender and race/ethnicity.
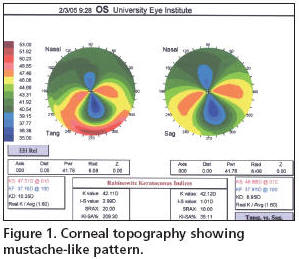
Mostly an inferior corneal disease, one study found that a small percentage (14.7 percent) may demonstrate superior PMD. This increases the diagnosis complexity by mimicking, at least by location, Terrien's marginal degeneration. PMD is usually characterized by a band of thinning inferior to the steepest protrusion that's apparent with either ultrasound pachymetry or a scanning slit topographer. Corneal topography will typically show a characteristic mustache-like steepened against-the-rule corneal pattern (Figure 1).
Unlike keratoconus, PMD doesn't exhibit Vogt's striae or a Fleischer's ring. Keratoconus and keratoglobus can be associated with PMD, with a small percentage showing other associated conditions such as vernal keratoconjunctivitis and Marfan's syndrome. Histopathology has demonstrated breaks and missing anterior limiting lamina similar to keratoconus patients.
Fitting PMD Patients
At the initial visit prepare your patient for the sometimes arduous process of achieving a satisfactory fit. Finding a lens that provides good vision and comfort is the goal and depends on the severity of the PMD. Fit options include lenses for keratoconic patients, GP lenses with and without special back surface designs, bitoric, bitoric aspherics, piggyback lenses and hybrid designs such as the SynergEyes lens (SynergEyes, Inc).
GP lenses tend to position inferiorly, aligning with the placement of the inferior steepened banded cornea. Liu et al (2005) reported on a reverse geometry lens (Reverse Aspheric Orthofocus, RAOF) to achieve satisfactory fit and vision. Others use large diameter lenses to increase lens/lid interaction and move the lens superiorly. Most patients wear lenses with good visual outcomes and sufficient lens tolerance.
A 2003 study by Raizada and Sridhar indicated that like keratoconus, the initial base curve depends on the disease severity. Base curves in this cohort ranged from 7.3mm to 6.3mm, the latter representing more severe PMD. They used an average of 3.5 diagnostic lenses to achieve a good fit.
Long-term Outlook
When contact lenses are no longer a viable option, a peripheral lamellar crescent keratoplasty with simultaneous or subsequent central penetrating keratoplasty may be performed. Intrastromal ring segments also work by flattening the corneal protrusion and decreasing the irregular astigmatism. Tzelikis et al found that surgical intervention is more likely in patients who have a best corrected visual acuity of worse than 20/100 and a follow-up period of greater than eight years.
Dr. Miller is the Director, Cornea and Contact Lens Service, at the University of Houston College of Optometry. He is a member of the American Optometric Association and serves on its Journal Review Board. You can reach him at wmiller@uh.edu.



