FITTING MULTIFOCALS
Growing Our Graying Contact Lens Practice
Fitting presbyopes in multifocals requires commitment, but it can provide significant revenue to our practices.
By John M. Rinehart, OD, FAAO

Dr. Rinehart is a graduate of Pacific University College of Optometry. After graduation he served 2 years as a Navy Optometrist at the Naval Aerospace Medical Institute, Naval Air Station, Pensacola, Florida. Since 1976 he has been in private general practice, with primary interest in GP contact lenses, in Peoria, Arizona. |
There are anywhere from 90 million to 100 million presbyopes in the United States. They are concerned with their appearance and don't want to do anything that makes them look older. These presbyopes have children who are grown up and, therefore, they may have extra disposable income. These factors combined mean they'll likely have an interest in multifocal contact lenses. This group can provide significant revenue to our practices if we're prepared to meet their contact lens needs.
Successful multifocal lens fitting, both soft and GP, requires that the contact lens fitter understands the lenses to be fit.
For GP lenses, fitting characteristics are different for translating and simultaneous designs. To achieve optimum performance with GP lenses, you must know how to get the most out of each lens design and match the best lens to each patient's visual needs.
Setting Expectations
You can achieve the greatest success with multifocal contact lenses by using diagnostic lenses. It's best to have at least two soft multifocal diagnostic lens sets as well as three GP sets. The GP multifocal sets should include a back aspheric design, translating design (possibly more than one design) and posterior annular bifocal.
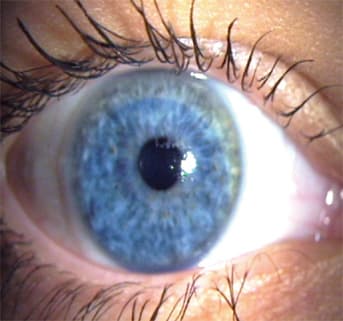
Figure 1. The lower lid is tangent to the lower limbus, the ideal position for a translating multifocal.
During case presentations make specific recommendations, including multifocal contact lenses when appropriate.
Just because your patient doesn't broach the subject of contact lenses doesn't mean he's not interested. He may have been told that he couldn't wear contact lenses or he may believe because of his age he's not a good candidate.
With the materials and designs available today, the success with multifocal contact lenses should be similar to the success with toric contact lenses. To achieve this success, both you and your patients must be committed to the process, have realistic expectations and understand the limitations to this means of vision correction.
Potential multifocal patients must realize that the goal is to minimize the need for supplemental corrections. It's realistic to expect well designed multifocal lenses to satisfy at least 80 percent of a patient's visual needs.
Patients should consider supplemental glasses, either for near or distance, as a special tool for specific tasks.
Who Are Good Candidates?
Moderate uncorrected hyperopes (+2.00D or greater) who think they see well at distance may be ideal candidates. In reality they don't see well at distance, so their vision will improve at all distances.
Low hyperopes and low myopes may not be great candidates — the former see well unaided at distance and the latter see well unaided at near. They may experience a slight degradation of vision that they don't want to tolerate.
Whether fitting soft contact lenses or GP multifocal lenses, diagnostic fitting produces the greatest success. However, this can be a time consuming process, and you should charge an appropriate fee whether or not you ultimately fit the patient with contact lenses.

Figure 2. The upper lid is in perfect position to allow a simultaneous multifocal to suspend and provide good centration.

Figure 3. In this case the upper lid is well above the limbus and is not in a good position for any simultaneous design multifocal.
Starting the Process
Select the initial soft multifocal diagnostic lens according to the manufacturer's recommendations. Many lens manufacturers provide extensive diagnostic lens sets, which means it's easy to determine at this initial fitting session the likelihood of success.
After the lens has settled on the eye for several minutes, determine if the lens moves and centers properly. Next determine distance acuity with the lens in place. If the lenses provide adequate distance acuity, test the near or intermediate acuity.
Simulate, as best as possible, the work environment for each particular patient and, using loose lenses or flippers, adjust the powers by ±0.50D. If you and the patient are pleased with the outcome, have the patient wear the lenses for about one week. This allows for evaluation in the "real world."
At the return visit determine, based on the patient's experience, if any fine tuning is necessary to achieve optimum vision. You can now prescribe this lens.
Remember that your goal here isn't perfection. Your ultimate goal is to limit the patient's need for supplemental correction over the multifocal contact lenses.
The diagnostic fitting process for GP multifocals is somewhat different. Most likely the diagnostic set won't have a wide variety of lens powers. Here the goal is to achieve ideal fitting characteristics for any particular design and to determine the best possible acuity for both near and far. Unlike the soft lens diagnostic fitting, it's not practical to send patients home to "test drive" the lenses in their own environments.
GP Lens Features
Next we'll look at features of GP multifocal lenses, both translating and simultaneous design.
When determining whether to use a translating multifocal or a simultaneous multifocal, you need to consider pupil size, lid position and vision tasks.
Large pupils may create a problem with translating designs causing ghost images because the pupil may extend into both the distance and near zones simultaneously.
Very small pupils may create the opposite problem with a simultaneous multifocal design and not allow sufficient exposure to all of the optics.
The ideal lower lid position for a translating design is tangent to the lower limbus with sufficient tension to support the lens (Figure 1). The lower lid should keep the contact lens in position while the pupil slides beneath the lens and into the area of near optics.
A simultaneous multifocal is suspended from the upper lid. The ideal upper lid position crosses the limbus at 10 o'clock and 2 o'clock (Figure 2). Figure 3 shows a case where the upper lid is well above the limbus and is not in a good position for any simultaneous design multifocal.
Generally speaking, a simultaneous multifocal will provide good distance acuity and good intermediate vision but may not provide ideal near vision, especially for very close work or very small detail.
For those patients who have very high near demands or need an add greater than +2.00D, you may need modifications such as biasing the distance power into the plus on the non-dominant eye. A translating contact lens will usually provide the best possible vision.

Translating Designs
The base curve for any translating lens should allow the lens to rest lightly on the lower lid and translate easily on downward gaze. The seg must be level within 15 to 20 degrees (Figure 4) and of course the lens must not compromise corneal health.

Figure 4. Here the top of the seg is nearly horizontal and just barely into the pupil.
When using diagnostic lenses to determine the initial base curve selection, first verify the lens. Select a lens approximately 0.50D flatter than flat K. Assess lens position, translation and seg orientation. If all appears satisfactory, over-refract, demonstrate the vision to the patient with a trial frame and have him simulate his work or hobby environment, then order the lens.
• Fitting Pearls For a lens to translate properly, it must not be steeper than the superior cornea.
Lens diameters for translating designs will be 2.0mm to 2.5mm smaller than the corneal diameter.
Position the top of the seg in the lower quarter of the pupil in dim illumination or at the bottom edge of the pupil in bright illumination.
The amount of prism necessary for a lens to orient properly will vary depending on the distance power of the lens. Table 1 is a good guideline to determine the initial amount of prism.
Most translating lens designs are available in both front and back toric and in virtually any base curve and power that's needed. Add powers typically range from +0.75D to +3.50D.
Troubleshooting Translating Lens Designs
When problem solving, first verify that the lens is as ordered and on the correct eye. You may need to resurface soiled lenses or replace them. Warped lenses need to be replaced. Evaluate the lens fit for seg position and lens movement as well as lens-to-cornea relationship (whether the lens fit is steep, flat or near apical alignment).
Poor distance acuity may result from an incorrect power, in which case an over-refraction and power change will solve the problem. The seg may be too high into the pupil resulting in the near zone power interfering with the distance acuity. In this case, truncate the lens to lower the seg.
• Fitting Pearl When truncating the lens, do so parallel to the lower lid, not necessarily parallel to the seg line.
Let's look at some common problems and their solutions.
Poor near acuity may be caused by poor lens translation, which requires a flatter base curve or an in-office reduction of the optical zone diameter (OZD). Other causes would include the seg being too low, which requires ordering a new lens with a higher seg position. Don't overlook the need for more near power.
Flare at night may result from the seg being too high; again, in this case, truncate the lens. Also, the optical zone may be too small, which requires a new lens.
Poor rotational stability can be solved by steepening the base curve or increasing the OZD. Increasing the amount of prism may solve this problem and/or truncating the lens may help.
When the lens is rotated but stable, truncate the lens, increase the prism or order a new lens.
When the lens slides beneath the lower lid, the lens may not be translating. If this is the case, flatten the base curve or decrease the OZD. You may also increase either or both the amount of prism or truncation.

Figure 5. Note the steep portion of the lens is not centered over the pupil.

Figure 6. The fit of the lens was steepened to cause the lens to center over the pupil.
Posterior Designs
Simultaneous multifocals include aspheric (front and back surface) and annular (anterior and posterior) designs. Here we'll discuss the back or posterior versions of these popular multifocals.
Posterior annular multifocals require near perfect centration to achieve the best possible distance acuity (Figure 5 and 6).
This design is available in virtually any base curve and distance power. Add powers will range from +1.00D to +3.00D. Distance OZDs range from 3.0mm to 6.0mm, but usually 4.5mm to 4.8mm is used. The near zone is approximately 1.5mm wide and the overall diameter is 2.0mm to 2.5mm less than the corneal diameter.
The near power zone is the area of the lens that controls the lens fit. You must calculate the radius of the distance zone so as to have the desired near power. The base curve of this lens will measure very steep, but because the OZD is small there shouldn't be any significant corneal steepening.
This is a relatively easy design to fit on current GP wearers whose lenses center properly. In this case, order the near zone radius the same as the base curve of the well fit lens. It's probably easier to have the lab calculate the radius and power of the distance zone.
To verify that the patient's current lens centers properly, color the center 4mm to 5mm with a red marker. Figure 7 shows it's easy to verify the position of the distance optical zone.
Aspheric multifocals are the design of choice for computer users. This lens provides great distance and intermediate acuity, but may not be ideal for those who have a very high near vision demand.
The following parameters have the most influence on the potential add power of an aspheric lens design.
Index of Refraction A high index of refraction will create more add power when all other parameters are left unchanged.
Eccentricity The higher the "e" value the greater the add effect.
Base Curve Radius Steeper base curves will result in greater add power compared to a flat base curve using the same eccentricity.
Optical Zone Diameter A larger OZD allows for more flattening and therefore more add power. There are limits to this effect depending on the size of the patient's pupil.
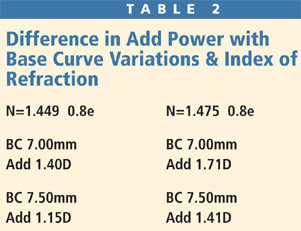
The example in Table 2 shows the difference in add power with variations of the base curve and index of refraction.
Fitting Pearls More add will be generated with a steep base curve and a lens material with a higher index of refraction. The greater the eccentricity, the greater the potential add power.
Select the initial base curve based on the amount of add desired. Remember the greater the add needed, the greater the eccentricity required.
Keep in mind that each manufacturer's fitting guide will vary slightly from these guidelines, but as a general rule if using 0.8e, fit 2.00D steeper than flat k; if using 0.9e, fit 2.50D steeper than flat K; and if using 0.99e, fit 3.00D steeper than flat K.
The lens diameter for an aspheric multifocal contact lens will tend to be large. As a general rule, choose a diameter that's 2.0mm smaller than the corneal diameter.

Figure 7. The red area shows where the distance optical zone will position using the patient's current lens fit.
Troubleshooting Simultaneous Multifocal Lenses
Poor distance acuity is most frequently caused by poor lens centration; adjust the base curve to achieve optimal centration. There can also be excessive lens interaction with the upper lid. This may require you to decrease the lens diameter or modify the lenticular flange.
Poor near acuity can result when the lens doesn't translate. If this is the case, flatten the base curve or decrease the lens diameter. Other solutions are to increase the eccentricity, increase the index of refraction of the material or add a small amount of eccentricity to the front of the lens.
Poor near and distance acuity can result when there is excessive residual cylinder. These designs are not ideal in this situation.
Flare at night can occur when the pupils are too large for the distance zone diameter. When using an annular design, increase the size of the distance zone. When using an aspheric design, incorporate a small spherical distance zone into the lens design, usually 3.0mm.
Commit to Fitting Success
Multifocal contact lens fitting requires a high level of commitment from both the practitioner and patient. Remember that no one multifocal lens design will accommodate all the needs of all patients.
It's important that both you and your patients have realistic expectations throughout the fitting process and understand that the ideal lens may not satisfy all of the visual needs.
Any multifocal design may create some compromise of acuity either at distance, intermediate or near. Finally, fit the lens to the patient, not the patient to the lens. CLS



