GPS & KERATOCONUS
Case Grand Rounds: GP Keratoconus Patients
How to successfully manage these sometimes difficult contact lens cases.
By Bruce Anderson, OD, Scott Edmonds, OD, & Edward Bennett, OD, MSEd
| Dr. Anderson is currently in private practice in Tampa, Fla., and is the director of the Contact Lens Clinics at the University of South Florida, College of Medicine, Department of Ophthalmology. Dr. Edmonds owns and manages the Edmonds Eye Associates at Wills Eye Hospital. He is Co-Director of the Contact Lens and Low Vision Service at Wills Eye Hospital. Dr. Bennett is an associate professor of optometry at the University of Missouri-St. Louis and is executive director of the GP Lens Institute. |
Managing contact lens keratoconus patients can be challenging but very rewarding. Certainly, improving a keratoconus patient's quality of life is a primary benefit. At the same time you can achieve professional satisfaction as well.
Practitioners ask numerous questions when fitting keratoconus patients. What diameter to select: small versus large versus mini-scleral? What material to use: low-Dk versus high-Dk versus hyper-Dk? What design to use: reverse geometry? Piggyback? How to manage an inferior-decentered cone?
Improved contact lens manufacturing technology has created options that will likely result in an improved lens-to-cornea fitting relationship and patient success. These innovations include larger diameter lenses, variable peripheral geometries and corneal topography as an aide in the manufacturing of a specific lens to a given corneal shape.
The goal of this article is to address these specific questions using challenging cases presented by the primary authors (SE and BA) as part of the Gas Permeable Lens Institute (GPLI) online symposium series.
Case One (SE)
History A 28-year-old male was diagnosed with keratoconus 10 years prior. He was refit from a standard GP design in June 2003 into the MacroLens (C&H Contact Lens, Inc.)
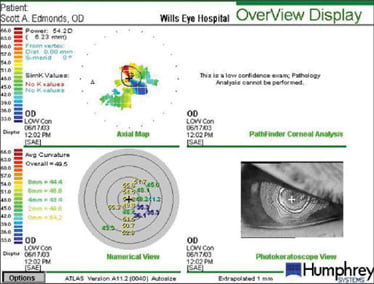
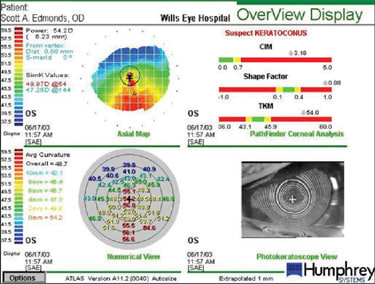
Figures 1a and 1b show the patient's baseline topography information. It's clearly evident that the right eye is more advanced as the image quality of the map is quite low and no simulated K readings were provided. The left eye exhibits an inferior-displaced apex.
The original fit OD was overall/optical zone diameter (OAD/OZD) base curve radius (BCR) 6.89mm; Power –10.00D. The OS fit was BCR 7.18mm; Power –10.00D.
During his visits from 2003 through 2007, several complications resulted from tight lenses OU. These included corneal edema, superficial punctate keratitis (SPK) and iritis. The inflammation responded well to short-term antibiotic steroid combination (TobraDex, Alcon).
In-office cleaning and patient education on proper care as well as flattening the peripheral curve radii temporarily helped re-establish lens movement and tear exchange. However, when evaluated in March 2007 he presented with marked 360-degree neovascularization, diffuse scarring and best-corrected visual acuity of 20/50 (OD and OS).
Management We refit him into the ABB♦ConCise ABB custom reverse geometry PMD lens in the following parameters. OD: OAD/OZD 10.0mm/6.6mm; power –11.50D; BCR 6.89mm; reverse geometry radius width (RGR/W) 6.70mm/0.35mm; intermediate curve radius width (ICR/W) 8.80mm/0.9mm; peripheral curve radius width (PCR/W) 10.5mm/0.45mm. The OS refit was: OAD/OZD 10.0mm/6.6mm; power –10.00D; BCR 7.18mm; RGR/W 6.95mm/0.35mm; ICR/W 9.00mm/0.9mm; PCR/W 10.7mm/0.45mm.
|
|
| Figure 1: The topography images of the patient in Case One are shown for the right eye (1a) and the left eye (1b). | |
Upon subsequent follow-up visits, the patient was achieving 20/25 OD corrected visual acuity and 20/25-1 OS. With slit lamp evaluation, both lenses decentered slightly inferiorly but there were no signs of adherence or peripheral sealoff. No clinical signs of corneal edema were present and the neovascularization had regressed.
Discussion The use of a consultant was valuable in this case, and ABB♦Con-Cise's Jim Slightom is one of the best. He recommended a reverse geometry design in this case even though that design is typically recommended for post-surgical cases, notably post refractive surgery. The small size of the reverse curve width (0.35mm) also assisted in enhancing lens movement.
In the case of an inferiorly displaced apex, several options are recommended. A large diameter lens, usually an intralimbal (10.0mm to 12.5mm), is often successful. Although a mini-scleral (13mm to 17mm) such as the MacroLens (C&H Contact Lens) or the Jupiter lens (Innovations in Sight) wasn't successful in this case, it is recommended when an intralimbal design is decentering inferiorly.
SynergEyes A (mild keratoconus) or SynergEyes KC (moderate-severe cases), both from SynergEyes, Inc., represents another option in this case. Likewise, the use of an O2Optix Custom (CIBA Vision) lens in a high plus power (+8.00D) will help "push up" the apex and allow the GP lens to center well in a piggyback design.
Every laboratory has multiple keratoconus lenses; one of the participants found the I-Kone (Valley Contax) beneficial as the GP lens in this piggyback combination. This is especially important in advanced keratoconus for which the steepest SynergEyes design (59D) isn't steep enough to provide a satisfactory fit.
In cases of relatively mild keratoconus or cases in which you can't achieve a good fitting relationship with a GP lens because of adaptation difficulties, use a specialty soft lens. These designs include the HydroKone lens from Dr. Rob Breece at Medlens Innovations and Soft-K, imported from Israel by Keith Parker for Advanced Vision Technologies.
Case Two (BA)
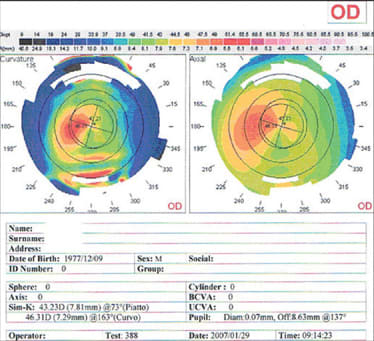
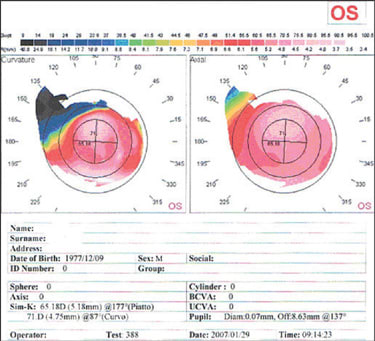
History A 29-year-old male presented in January 2007 for a contact lens fitting for keratoconus. He stated that in previous fitting attempts a comfortable right lens was never achieved and the left eye was never successfully fit into contact lenses. He was seriously considering pursuing a corneal transplant for the left eye. His vision with his current spectacle prescription was 20/70 OD and count fingers at 3 feet OS. Slit lamp evaluation revealed slight corneal thinning OD but no other obvious clinical signs. The left eye exhibited 3+ corneal thinning with 2+ corneal scarring and an obvious Fleischer's Ring. Figures 2a and 2b show the baseline corneal topography.
Management The initial diagnostic lens OD had a prescription of BCR 7.54mm; OAD/OZD 8.67mm/7.2mm; power –3.00D; SCR/W 9.00mm/0.5mm; PCR/Width 12.2mm/0.2mm
|
|
| Figure 2. The topography images of the patient in Case Two are shown for the right eye (2a) and the left eye (2b). | |
The fluorescein pattern showed that the diagnostic lens fit slightly flat and positioned centrally with minimum edge clearance. With an over-refraction of +0.75D, the vision was corrected to 20/20.
For the left eye, we used a fitting lens with a prescription of BCR 5.63mm; OAD/OZD 8.6mm/6.0mm; power –8.00D; SCR/W 6.22mm/0.3mm; ICR/W 7.42mm/0.3mm; PCR1/W 9.22mm/0.3mm; PCR2/W 11.22mm/0.4mm (Maguire Cone Design).
The left contact lens wouldn't stay on the eye any longer than a few seconds before displacing. With fluorescein, we observed that the lens fit extremely flat centrally with significant edge lift off. With the aid of corneal topography and the parameters of the fitting lens as a guideline, the initial contact lenses ordered were OD BCR 7.54mm; OAD/OZD 9.8mm/7.8mm; power –2.25D; SCR/W 9.00mm/0.4mm; ICR/W 11.0mm/0.3mm; PCR1/W 13.0mm/0.3mm. For the left eye we ordered BCR 64.50D; OAD/OZD 8.6mm/6.0mm; power –22.00D; SCR/W 6.10mm/0.3mm; ICR/W 7.40mm/0.3mm; PCR1/W 9.25mm/0.3mm; PCR2/W 11.50mm/0.4mm. The material was Boston XO (Bausch & Lomb).
We dispensed the lenses in February 2007. The vision in the right eye was 20/20 and the left eye was 20/30-. The right contact lens centered well with a slight upper lid attachment. The left lens fit inferiorly with central bearing and excessive edge clearance; upon a forced blink it would displace from the eye. Over the next four weeks we made two additional exchanges with the left lens that were progressively steeper in both base curve radius and peripheral curve radii. However, at the ensuing follow-up visit, excessive edge clearance was still evident and the patient complained that the lens often displaced off of the eye.
With the use of diagnostic fitting lenses and evaluation of the fluorescein pattern and position of the lens on the eye, we then refit this patient into the following Dyna Intralimbal (Lens Dynamics) lens OS: BCR 55.00D; OAD/OZD 11.2mm/9.4mm; power –11.25D; Periphery STD.
This lens stayed well in place and exhibited approximately 0.5mm to 0.75mm movement with the blink. There was a slight flat central region and slightly excessive edge clearance. With an over-refraction of –3.00D, he was able to read 20/50+. We ordered a new contact lens for the left eye with the following parameters: BCR 55.00mm; OAD/OZD 11.4mm/9.4mm; power –14.25D; Periphery STD. We used a Dyna Intralimbal design (Menicon Z material).
At subsequent follow-up visits, both the original right lens and the intralimbal left lens have demonstrated an acceptable fitting relationship and the patient is quite satisfied with the vision.
Discussion This case represented a contrast between mild keratoconus (OD) and severe keratoconus (OS). The topography for the right eye demonstrates a notable temporal cone that was only moderate in steepness.
We ordered a lens with a larger diameter than that of the initial diagnostic lens in an attempt to vault over the cone and obtain an upper lid attachment. A multiple peripheral curve design allowed flaring of the lens edge with a fairly flat third peripheral curve to ensure that the lens would obtain proper movement and edge clearance. As this lens was not steep by keratoconic standards, a larger OZD, as compared to the fitting lens, allowed this lens to vault over the cone and result in good centration and movement.
By contrast, the patient's left eye had an advanced cone and, with all attempts to design a standard cone design, the lens would not stay in position on the eye. An intralimbal such as the Dyna Intralimbal design is a viable option when a small diameter lens does not fit optimally. It's important, however, to monitor these patients to ensure that significant bearing does not occur on the apex, resulting in punctate keratitis and possibly a corneal abrasion.
When excessive edge clearance is problematic in a keratoconic design, many new designs have variable peripheral curve radii and eccentricities such that the periphery can be flatter in one meridian than the other or, in the case of the Quadra-Kone (Tru-Form Optics), the peripheral curvature can vary by quadrant. This is especially invaluable in eliminating bubbles, as well as in improving centration. These designs are especially valuable in cases such as Case Two, in which edge clearance is excessive. It's not uncommon to observe this problem inferiorly in advanced keratoconus.
Several new quadrant-specific designs should be forthcoming in the near future. One such design was presented at the Global Keratoconus Congress in January. In this case, the lowest eccentricity was inferior (due to excessive edge clearance) and the highest was superior.
There is some controversy as to what would be the optimum material for a keratoconic design. The rigidity of lower Dk (25–50) materials should provide for less flexure and better astigmatic correction. However, many keratoconic patients over wear their lenses due to the absence of satisfactory vision with their spectacle correction (if they, in fact, own spectacles). Most designs in common use today utilize high/hyper-Dk lens materials such as Boston XO and Menicon Z.
The issue of whether bitoric designs should be used in keratoconus is also challenging. Although most of these patients are highly astigmatic, when moderate irregularity is present, as is often the case, bitoric lens designs wouldn't provide optimum vision or a satisfactory lens-to-cornea fitting relationship. The exceptions would pertain to those early or subclinical keratoconic patients who have relatively symmetrical astigmatism.
Summary
It's evident that several options exist to manage any particular keratoconus patient. Nevertheless, Contact Lens Manufacturers Association (CLMA) laboratory consultants are an important component in successfully managing these patients. The availability of diagnostic lens fitting sets, the type of lens diameter and periphery for a given topography and the effective troubleshooting of these patients are among the benefits that experienced, knowledgeable consultants provide.
Another resource is available online. Gpli.info has a new online book titled, "GP Lens Case Grand Rounds Troubleshooting Guide," which includes the management of eight distinctly different keratoconus cases and eight other irregular cornea and post-surgical cases. Attending meetings such as the Global Keratoconus Congress and utilizing the educational services, including educational pamphlets for patients and reimbursement forms for practitioners, provided by the National Keratoconus Foundation are invaluable aides in managing these challenging but very rewarding patients.
Any practitioner can successfully manage these patients if willing to carefully evaluate the lens-to-cornea fitting relationships and utilize the lens selection pearls and consultative and educational resources discussed here. CLS
The authors would like to acknowledge the following for their contributions: Steven Mathews, Steve Byrnes, Ray Brill, Derek Louie, Bruce Williams, Terry Scheid, Alex Crinzi, Bob Maynard, John Rinehart and Jon Kendall.



