SOLUTION-INDUCED STAINING
Practical Applications of the Staining Studies
Recommendations for how to use data from recent research on corneal staining in clinical practice.
By Mile Brujic, OD

Dr. Brujic is a partner in a multi-location group practice where he sees patients in Bowling Green and Lima, Ohio. He lectures nationally on contemporary topics in eye care. He is a member of the Alcon Speakers Alliance and has worked in an advisory capacity for Vistakon. |
There are many factors that clinicians need to consider when fitting patients with contact lenses. Initially, you need to determine the lens power to correct a patient's refractive error. Then select a material that is most appropriate for the patient. If the lenses aren't daily disposable, then you must select an appropriate lens care system.
But what designates an appropriate care system? I believe an ideal lens care system kills all ocular pathogens, reconditions the lens surface to provide long-lasting comfort and is minimally disruptive to the corneal epithelium.
Recently, some important reports have published in the literature concerning solution-induced corneal staining during contact lens wear. I would like to review some recent research in this arena and discuss how I apply it to my practice.
What is Corneal Staining?
Fluorescein can occupy intercellular spaces of the corneal epithelium when cell junctions have been disrupted. It may also pool in depressed areas as well as stain injured corneal epithelial cells. Staining is optimally viewed with a cobalt blue light and a Wratten #12 filter as pooled fluorescein will fluoresce.
Corneal staining may be present for many reasons. As normal epithelial cells turn over on the cornea, small amounts of staining may become visible. Certain disease states such as dry eyes may cause significant staining. Recent research has also shown that interactions between some brands of contact lenses when used with certain multipurpose solutions may cause corneal staining.
From a clinical standpoint, it's often difficult to interpret and assimilate information and data from many different studies. This is especially true for the various studies evaluating multipurpose solutions and their effects on the cornea. Differences in the lens/solution combinations tested, grading scales, color-coding criteria and study controls such as masking and observation times make direct study-to-study comparisons difficult.
Two recent studies on this topic, although somewhat different in the details of their methodology, provide valuable information for clinicians. Let's examine these studies to understand how they can be useful in both decision-making and patient education efforts.
The Staining Grid Study
One of the most extensive studies to date investigating solution-induced staining was undertaken by Gary Andrasko, OD, MS, and Kelly Ryen, OD, in a private research practice. In this ongoing study initiated in 2005, both examiners and subjects were masked to the contact lens and care systems tested. Lenses were soaked overnight in the solution being tested and then placed on the eyes of adapted lens wearers. After two hours of wear, examiners removed the lenses, instilled fluorescein and examined the cornea with a cobalt blue light and a Wratten #12 filter. They then reapplied the lenses and repeated the same procedure after two additional hours of lens wear. Andrasko chose these examination times based on independent research demonstrating that solution-induced corneal staining reaches its peak levels between two-to-four hours after lens application.
The study examiners reported the severity of staining by dividing the cornea into five regions (central, temporal, superior, nasal and inferior) and grading the level of staining in each zone as a percentage of corneal area stained. The staining in each zone was then averaged to determine the overall corneal staining for each eye.
Andrasko presents the results of 30 subjects for each lens/solution combination in a format which he terms the "Staining Grid" (Figure 1), which is also available at www.StainingGrid.com. By viewing the results at the intersection of the lens row and solution column, you can see the level of corneal staining for each lens/solution combination tested.
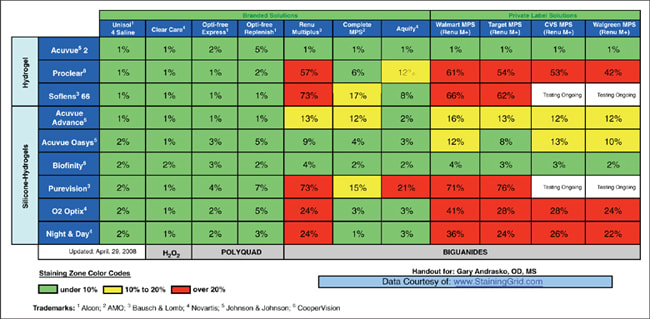
Figure 1. Andrasko Staining Grid showing average corneal staining at two hours.
The Staining Grid is color-coded using three colors to allow visualization of staining patterns among the lens materials and solutions tested. To date, the examiners have tested more than 90 different combinations including several generic (or private-labeled) solutions.
The Staining Grid may serve as a tool for selecting an appropriate care system for use with a contact lens brand prescribed. Examination of the color-coding of the Staining Grid (with red representing greater than 20 percent of the cornea occupied by micropunctate staining) reveals that combinations involving group II lenses and silicone hydrogel lenses seem more likely to develop higher levels of staining at two hours with certain biguanide-based care systems including private-label solutions. Both the polyquad and hydrogen peroxide-based systems showed relatively low levels of staining with all of the contact lenses tested.
The IER Matrix Study
The Institute for Eye Research (IER) has recently published a corneal staining matrix that examines the number of patients experiencing what the researchers' term solution-induced corneal staining (SICS) of patients wearing different contact lens/solution combinations over a three-month period. SICS describes a cornea that experiences any level of staining in four out of five corneal zones. This study was an open-label evaluation to both subjects and examiners of both the lenses and solutions tested. Figure 2 shows the results.

Figure 2. The IER Matrix showing solution-induced corneal staining per month with each combination*. Courtesy of Carnt et al. Originally printed in March 2008 issue. Reprinted with permission.
Patients in this study were evaluated at baseline, two weeks, one month and three months after they began wearing the lenses. The IER reports the percentage of subjects experiencing SICS on its matrix as opposed to magnitude of corneal staining as presented in the Staining Grid. Researchers examined subjects for staining anytime between 8 a.m. and 7 p.m. These non-standardized staining observation times may result in variability of the staining response, even within a particular lens/solution combination.
The IER Matrix uses a color-coding based upon quartiles. Combinations falling in the lower quartile of staining are colored green, the middle two quartiles are yellow and combinations in the upper quartile are colored orange. One consequence of using a quartile system is that the color assigned to any combination is strongly influenced by which products are tested. Additionally, future testing may result in a change in color of previously tested combinations. To date, the IER Matrix study has tested 20 lens/solution combinations, with the vast majority yielding low percentages of subjects exhibiting staining.
A data analysis of the IER Matrix reveals some definite patterns. Clear Care (CIBA Vision) demonstrates little SICS. The PureVision (Bausch & Lomb) and Aquify (CIBA Vision) combination exhibits the highest level of staining among all lens/solution combinations. Interestingly, all other combinations show relatively low amounts of SICS.
Applying the Information Clinically
As a practitioner concerned with recommending the most compatible care system for each lens brand, I find both studies extremely useful. The Staining Grid gives me a broad overview of the staining results of many multipurpose solutions when combined with several popular lens materials. The color-coded Staining Grid allows me to quickly determine the relative compatibility of more than 90 lens/solution combinations after two hours of wear. Additionally, I find the Staining Grid useful as an educational tool when explaining to my patients the importance of continuing to use the care system that I've prescribed. Patients appreciate that my recommendations are based upon research, and fortunately this has dramatically decreased the occurrence of inadvertent care system switching.
While the Staining Grid gives a short-term snapshot of lens/solution compatibility, the IER Matrix provides a more long-term view. Keep in mind that the IER Matrix measures the number of patients using each lens/solution combination experiencing SICS (again, SICS is defined as those patients experiencing any corneal staining in four out of five corneal zones and does not measure the magnitude of staining). The IER Matrix tested those solutions that demonstrated the least amount of corneal staining on the Staining Grid. Other than the Aquify/PureVision combination in the matrix, all other combinations show relatively low rates of SICS.
Conclusion
Many factors contribute to a successful lens wearing experience. Hygienic practices and proper compliance with prescribed wearing regimens is crucial. Adequate disinfection and lens surface reconditioning are also important considerations. In our efforts to minimize disruption of the corneal epithelium, we now have two significant studies on this topic that provide valuable tools to ensure an optimal lens care system recommendation. Through further research and understanding in this area, we will continue to add to our current knowledge base of corneal staining and its effects on our lens wearers. CLS
I would like to acknowledge Dr. Gary Andrasko for graciously offering insights into the Staining Grid.
For references, please visit www.clspectrum.com/references.asp and click on document #153.



