Online Photo Diagnosis
By William Townsend, OD, FAAO
This 12-year-old Hispanic male presented to our office with a complaint of pain and blurred vision in his right eye. Another eyecare provider had previously told his parents that his right eye was amblyopic. They reported that he had trauma to that eye when he was 4 years of age. His recent eye history was significant for trauma; his girlfriend had thrown a pencil across the classroom, apparently as a sign of affection. The point of the pencil struck his right eye. He presented with a complaint of minimal discomfort, but he reported blurred vision in the affected eye. Presenting acuities were OD 20/100, and OS 20/20.
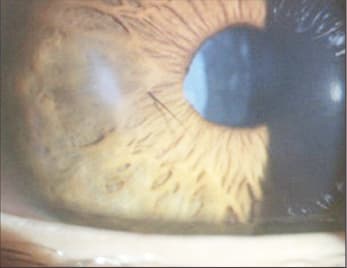
Slit lamp examination of the right eye revealed an old corneal scar inferior to the visual axis. A 3mm full thickness corneal laceration was noted in the temporal cornea. Instillation of fluorescein revealed Seidel's sign at the site of the entry wound. There was shallowing of the anterior chamber and fluffy, white cortical material floating in the vitreous. The anterior chamber also had significant flare and cells. We noted an eyelash embedded in the anterior surface of the iris. The lens showed cortical clouding surrounding the lip of the wound.
Our diagnosis was full thickness corneal laceration with Seidel sign and traumatic cataract secondary to penetrating injury. We contacted an ophthalmologist with whom we work closely. Our plan was to instill a topical antibiotic and use a soft lens to create a tapenade. Once the Night & Day (Ciba Vision) lens was in place, the flow of aqueous was significantly reduced. The following morning, the patient reported reduced discomfort; there was no evidence of endophthalmitis. Once the bandage lens was removed, the passage of aqueous resumed. We instructed the patient not to eat or drink anything and sent him to the ophthalmologist.
The surgeon sutured the wound and then performed cataract surgery with implantation of an intraocular lens. Ultimately, the best-corrected vision in the operated eye was 20/80. He has since been lost to follow up.
Penetrating ocular injuries vary in severity, from a microperforation that ultimately self seals to wounds that require enucleation. Secondary endophthalmitis may be difficult to distinguish from the injury and its sequel, but you should look for and recognize early clinical signs and symptoms of endophthalmitis such as reduced vision, hypopyon, vitritis, or retinal periphlebitis. Factors that increase risk for endophthalmitis include retained foreign body, injury in a rural setting, delay in primary wound closure, and loss of the crystalline lens.
When it is necessary to refer for surgical intervention, it is important to advise the patient to not drink or eat anything (NPO). Anesthesia inhibits the normal coughing response to aspiration of foreign material, including regurgitated stomach contents. Aspiration of solid, acidic, or gastric contents can cause potentially life-threatening pneumonia. This is much less likely to occur when the patient has not had anything to eat or drink for several hours prior to the procedure.



