readers' forum
Summing Up Piggybacking of Contact Lenses
BY BEZALEL SCHENDOWICH, OD, FIACLE
A standard keyword search of the archives on the Contact Lens Spectrum Web site for the word "piggyback" quickly yields more than 60 references from the past 11 years. A Medline search finds another pertinent hit that published in 1985 in another journal. This first reported instance of cushioning a rigid lens with a soft contact lens could not have occurred before soft contact lenses became an important tool in our profession.
While it's not certain who first considered using an early generation soft contact lens to ease the suffering of a rigid contact lens patient who had keratoconus, it's clear that today's contact lens professionals are realizing the potential of piggyback systems to increase wearing time by improving GP lens comfort on distorted, ectatic or post-keratoplasty corneas.
I've found several important reasons to use piggyback systems in my growing clinic population of patients with suffering corneas. The most important is the bandage effect of the soft lenses, which protects corneas that tend to erode as well as protecting the tip of proud nebular wounds from the physical effects of constant contact with a flat GP lens.
Initial Considerations
Fitting a piggyback lens system is not really the most challenging part of contact lens practice, though it may be quite rewarding from a practitioner-patient relationship point of view: you become a hero by improving comfort and stretching wearing time nearly instantaneously.
Piggyback fitting requires you to answer for yourself and your patients basic questions relevant to the choices of contact lenses and materials. Lens material choices revolve around the necessity of providing vision and comfort while not compromising ocular health.

Ocular health in turn depends upon the hygienicity and oxygen permeability of the contact lens system. As the ophthalmic world has learned so dearly over the past two years, keeping contact lenses properly cleaned and disinfected is not so easy as solution manufacturers would have contact lens wearers believe. GP contact lens care is pretty clear: patients must clean in a recommended solution and soak in a recommended disinfecting/conditioning solution.
Similarly, soft contact lenses, if they are to be reused, require a thorough rubbing step before rinsing and soaking/disinfection in totally fresh solution every time (no topping off). The propensity of the hydrogel or silicone hydrogel matrix to absorb/adsorb solution components and later release them when the lens is in situ can in some cases cause corneal insult.
An elegant and simple way to avoid both the problem of an improperly or incompletely cleaned and disinfected lens and the problem of solution toxicity is to use daily disposable soft contact lenses. To date this lens modality is not available in a silicone hydrogel material, so oxygen permeability with these lenses could be an issue in a two-lens combination.
Meanwhile, GP lens materials have become ultra-permeable. This, in addition to the well-established characteristics of GP lenses (ease of cleaning, length of useful lifespan and quality of vision) helps GPs maintain their primary position in the toolbox of specialty fitters. To some extent the ultra-permeability of newer GP lenses allows adequate corneal oxygenation even in combination with a relatively low-Dk hydrogel lens.
For the soft contact lens portion of my piggyback combination, I've learned that a daily disposable lens satisfies my requirements for a clean, thin lens that is not so expensive that patients will balk at the cost of the piggyback system.
Fitting Techniques
From a technical standpoint, there are two methods to fitting a piggyback contact lens system:
- Applying a soft contact lens under an existing GP.
- Fitting a GP to the new surface created by the soft contact lens on the distorted cornea.
When you have labored industriously to find a best fitting (or as good as can be expected) GP lens for a particular cornea and there is still occasional erosion or insurmountable discomfort, you can apply a soft contact lens to protect the cornea and reapply the GP on top. There are both pluses and minuses with this technique. On the plus side, it's quick and easy and utilizes existing resources. On the other hand the fitting relationship between the two lenses is likely to be less than optimal (Table 1).
In the event that a patient presents with an existing corneal insult, such as a large erosion or superficial fibroplastic nodule formation on the apex of a cone, and he needs to be fit with a GP lens to achieve usable vision, fitting the soft contact lens first adds a new dimension to the fitting process while significantly reducing the irritation felt by the patient upon application of the GP lens.
The soft lens may help provide useful topography information as well. Topography devices can't interpret many irregular corneas to any useful degree other than to help recognize their distortions. Some can be interpreted, but the information gleaned does not render usable fitting data; the curvature and eccentricity data aren't reliable. By applying a soft lens and then repeating the topography, it may smooth out the distortions to allow a more accurate evaluation of the new corneal/lens surface we are fitting. (Figure 1).
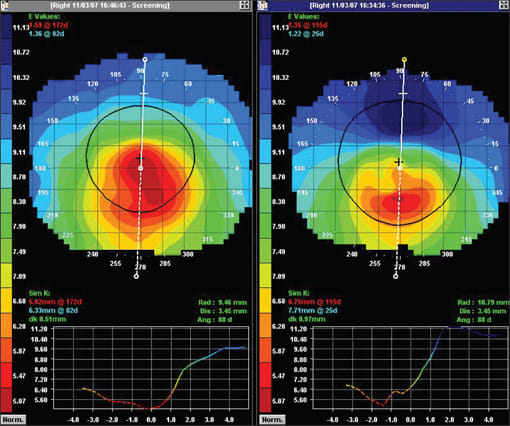
Figure 1. Two axial maps of the same eye. The first, on the right, is without a soft contact lens while the left image shows the soft lens in situ. The smoothing of the distortion with the soft lens is evident.
Using the topographically new surface, we can begin the GP fitting process. The goal when fitting the soft lens first is to search for a piggyback system with a better fitting relationship between the two lenses. Ideally the soft lens should demonstrate some movement over the cornea, and the GP should have some freedom of movement over the surface of the soft lens.
Binding and Fluting
Two potential problems associated with piggyback systems are edge binding of the GP lens through the soft lens and fluting of the inferior edge of the soft lens. Binding frequently occurs when using the fitting technique of applying a soft lens under an existing GP lens. Because the new surface is flatter overall than the cornea to which the GP originally fit, any edge lift that previously existed is likely to be lessened. This is especially apparent in the midperiphery and periphery of the lens, where the keratoconic cornea flattens much more quickly than for what standard GP lens designs allow.
Binding indicates a necessity to redesign the edge profile of the GP lens, if piggybacking is to succeed. On the other hand, fluting of the soft lens just above the lower lid margin begs a steeper soft contact lens.
Soft Contact Lens Power
Piggybacked GP and soft lens powers when in situ are not additive. An elegant proof of this fact appeared via the Internet portal Optcomlist several years ago in a fascinating discussion of the optics of piggyback systems between Drs. Charles McBride and John C. Heiby. The bottom line from the exchange is that the soft contact lens component will contribute about 20 percent of its power in air. Practically, this means that a thin soft lens of labeled power between +1.00D and –1.00D will make only a negligible change in the power of the lens pair on the eye.
Care of Piggyback Lenses
Lens care of single lens systems has been a cause for concern since the first contact lens was applied to a cornea. As we all know, care systems today are important — and it's our role to describe, prescribe and even provide the appropriate care for the lenses we recommend. The problems involved in caring for single lens systems may well be even greater for piggyback systems.
GP care is straightforward, but you must review it at each follow-up visit, especially because in a piggyback system we are obligated to alter our instruction set. When we apply a GP lens over a soft contact lens, we must restructure our instructions for care and the choice of solutions that we will employ.
You need not change the cleaning and storing regimen for GP lenses because patients perform these steps at the end of the wearing day. However, rinsing and conditioning solution use prior to lens application needs revision:
| Lens material choices revolve around the necessity of providing vision and comfort while not compromising ocular health. |
- Never with tap water — or with any other liquid not designed for use with soft contact lenses.
- Standard GP solutions may not work well with soft lenses.
So, it seems that the best bet is rinsing and applying the GP lens with the same solution used for the soft contact lenses.
Practical Advice Through experience, several points are evident:
- Both the soft and GP lens must be clean when applied.
- I allow removal of the whole set of lenses for a mid-day cleaning with both a rub and soak treatment with a multipurpose solution for disposable soft contact lenses.
- Weekly protein removal for the GP lens.
- More frequent follow up with fluorescein staining.
Conclusion
My contact lens fitting goals have not changed. I primarily seek a healthy physiological relationship between the lens system and the external eye and its adnexa. I then try to achieve optimal visual acuity, comfort and cosmesis — in that order. Patients, on the other hand, generally position their goals in a different order: comfort, cosmesis and then vision.
When we as fitters and healthcare providers realize the need to use a piggyback system for health or comfort reasons, we find that our patients seem to benefit greatly. Nevertheless, we must exercise vigilance in caring for our piggyback lens wearers. It's vital to the well being of our patients that we are extremely careful in our instructions and questioning about lens care during follow-up sessions. The major battle here is not in the analysis of the cornea, in the contact lens fitting or in the selection of materials, but rather the battle is against noncompliance. CLS
Dr. Schendowich is a Fellow of the International Association of Contact Lens Educators, an adjunct assistant clinical professor of optometry at SUNY-Optometry in the optometry clinic at the Sha'are Zedek Medical Center, Jerusalem, Israel, and he is a Member of the Medical Advisory Board of the National Keratoconus Foundation.



