dry eye dx and tx
The Conjunctiva and Dry Eye
KATHERINE M. MASTROTA, MS, OD, FAAO
In dry eye and ocular surface disease, changes in corneal surface integrity are readily recognizable. However, the conjunctiva can also suffer pathologic changes in response to surface insults. The conjunctiva serves as a nourishing support system for the cornea, and its proper functioning is critical to corneal health. It contributes to the tear film and is essential for local immune defense of the ocular surface.
Conjunctival Structure
Histologically, the conjunctiva is composed of the superficial epithelium and the underlying substantia propria, or stroma, which is richly vascularized and contains numerous different cell types for innate defense and immune protection. The conjunctival epithelium is a stratified, nonkeratinized, secretory epithelium, and its cell type varies depending on location from columnar in the tarsal and cuboidal in the bulbar area to prismatic in the forniceal area and squamous near the lid margins and limbus.
The conjunctiva is continuous with the nasal mucosa through the lacrimal puncta, with the corneal epithelium at the corneoscleral limbus and with the eyelid skin at the mucocutaneous junction, known as the Marx's Line. The conjunctival surface can be divided into six zones: starting from the lid margin these are the marginal, palpebral (or tarsal), orbital, forniceal, bulbar and limbal conjunctiva (Figure 1).
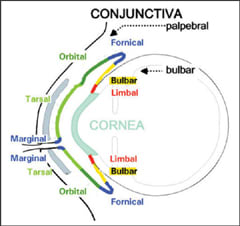
Figure 1. Zones of the conjunctiva.
Conjunctival Functions
The marginal mucosa of the conjunctiva, now referred to as the "lid wiper," is responsible for tear film spreading. In dry eye conditions, reduced tear film lubricity is thought to be responsible for damage to the lid wiper cells, which in turn causes reciprocal damage to the corneal surface.
The tarsal conjunctiva lines the inner surface of both eyelids and contains a number of infoldings of epithelium, called Henle's crypts. The crypts increase the conjunctival surface area and the conjunctiva's functional capacity, housing a high concentration of mucin-producing goblet cells. Goblet cell density is also high in the forniceal area, which is also thought to contain the majority of conjunctival stem cells.
Conjunctival-associated lymphoid tissue (CALT) is a complex mucosal immune tissue dedicated to ocular defense of exogenous antigens and is primarily located in the upper palpebral conjunctiva and in the fornix. It is involved in the allergy response as well as in giant papillary conjunctivitis.
The limbal conjunctival epithelium is unique in that it has fingerlike projections into the lamina propria, the Palisades of Vogt, which are considered to house the stem cells of the cornea. Here the conjunctiva is devoid of goblet cells, however, Langerhan's cells and melanocytes can be found in its basal layer. The limbus serves as an important barrier between the cells of the conjunctiva and those of the cornea.
As with the cornea, the apical surface of the superficial cells of the conjunctiva exhibits microplicae and microvilli that function, in part, to anchor the overlying tear film to the cell surface; interestingly, the microvilli have variable density and length depending upon conjunctival cell type. Long-term disruption of conjunctival function, as in dry eye or other disease, can lead to squamous metaplasia of the conjunctiva, the pathological transition of a secretory, nonkeratinized, stratified epithelium into a dysfunctional, nonsecretory, keratinized epithelium unable to maintain ocular surface homeostasis. CLS
Dr. Mastrota is a 1989 graduate of SUNY State College of Optometry. Currently she is center director at the New York Office of Omni Eye Services. She is also a consultant to Allergan, AMO, B&L, Inspire and Cynacon OcuSoft.



