LENSES & DRY EYE
What Influences Contact Lens-Related Dry Eye?
Understanding these factors will assist you in effectively managing contact lens patients who have dry eye.
By Lakshman N. Subbaraman, PhD, BSOptom, MSc, FAAO, & Lyndon Jones, PhD, FCOptom, DipCLP, DipOrth, FAAO (Dip CL), FIACLE

Dr. Subbaraman recently completed his PhD at the School of Optometry, University of Waterloo. Shortly, he will be joining the Chemical Engineering Department, McMaster University, Hamilton as a Post-Doctoral Researcher. |

Dr. Jones is the associate director of the Centre for Contact Lens Research and a professor at the School of Optometry at the University of Waterloo, Ontario, Canada. He has received research funding from Alcon, AMO, B&L, CIBA Vision, CooperVision, and Johnson & Johnson. |
Contact lens wear can induce ocular symptoms that are remarkably similar to those reported by patients who have various dry eye conditions. These symptoms affect almost 17 million of the 35 million contact lens wearers in the United States alone.
While contact lenses are considered a contributing factor in dry eye disease, many believe that the diagnosis and management scheme should be different for contact lens-related dry eye. The 2007 Report of the International Dry Eye WorkShop (DEWS) suggested that contact lens-related dry eye is a subclassification of dry eye syndrome.
Over the last few years, several questionnaires have been developed to identify dry eye symptoms in lens wearers. Findings from these questionnaires indicate that contact lens wearers are 12 times more likely than emmetropes and five times more likely than spectacle wearers to report dry eye symptoms. Several reports suggest that approximately 50 percent of contact lens wearers report dissatisfaction with lens wear, and 24 percent of patients permanently cease lens wear due to these symptoms.
The common symptoms associated with lens wear include dryness, discomfort, redness, burning, lens awareness, grittiness, irritation, stinging, ocular fatigue, scratchiness, soreness, blurry vision, and itching. Surveys of former wearers show that dryness and discomfort were primary reasons why a large proportion of patients ceased lens wear. In a study performed at a university-based clinic, 109 of 453 subjects with a history of contact lens wear discontinued lens wear permanently, and 119 current lens wearers expressed lens dissatisfaction. Both groups ranked dryness as their most common ocular symptom.
It is important that we understand the factors that play a role in contact lens-related dry eye. Understanding these factors will assist you in effectively managing these patients, which will help prevent contact lens dropouts. There is considerable interest in the contact lens research community in determining the impact of lens materials, rewetting agents, and care solutions on lens-related dry eye. The aim of this review is to address the various factors that are associated with contact lens-related dry eye.
Contact Lens Material-Related Factors
The U.S. Food and Drug Administration (FDA) currently classifies commercially available hydrogel lens materials into four groups, based on their charge and water content: Group 1, non-ionic, low water content; Group 2, non-ionic, high water content; Group 3, ionic, low water content; Group 4, ionic, high water content. The FDA material classification seems to be a very strong predictor of contact lens-related dry eye.
Water Content and Ionicity The odds of developing dry eye symptoms in non-ionic, high-water-content (FDA Group 2) and ionic, high-water-content (FDA Group 4) lens wearers are two-to-three times greater than that associated with FDA Group 1 lens wear. Furthermore, FDA Group 2 lens materials were more commonly associated with dry eye than were the FDA Group 4 lens materials. Efron and Brennan (1988) also showed that patients who wore low-water-content lenses that maintained their hydration (compared with low-water-content lenses that dehydrated) generally reported that their eyes "never felt dry" during wear. Thus, the evidence to date suggests that patients using lower-water-content lenses are less likely to complain of lens-related dry eye. Interestingly, the majority of silicone hydrogel lens materials are FDA Group 1.
Dehydration One of the factors to consider in contact lens-related dry eye is lens dehydration, as the subjective symptom of dryness appears to occur more frequently in soft lens wearers whose lenses undergo greater dehydration (higher-water-content lenses) during open-eye wear. Potential factors that may explain dehydration-induced discomfort include increased lid-lens interaction through alterations in lens front-surface wettability, alterations in lens fit, or the development of epithelial staining due to per-vaporation and subsequent desiccation.
All hydrogel lens materials dehydrate during wear. Dehydration is influenced by a number of factors including the environment, water content, water thickness, and wearing period. Traditional hydrogel lens materials dehydrate more than silicone hydrogel lens materials do. Efron and Morgan (1999) showed that dehydration can affect the fit of a hydrogel lens by altering the lens parameters, in addition to lowering the oxygen transmissibility. Nevertheless, the relationship between dehydration and in-eye comfort remains controversial. Although some studies have found a correlation between dehydration of hydrogel lenses and a decrease in lens comfort, others were not able to demonstrate a relationship between lens dehydration and decreasing comfort or dryness. Materials such as omafilcon A, hioxifilcon A, and hioxifilcon D that are highly resistant to dehydration can provide increased comfort. Thus, the debate regarding the influence of dehydration on comfort continues, suggesting we do not completely understand the relationship between dehydration and discomfort.
Deposition Following application, soft contact lenses rapidly absorb components from the tear film, particularly proteins, lipids, and mucins. At extreme levels of buildup, these deposits are associated with diminished visual acuity, dryness and discomfort, lid-related inflammatory changes, and contact lens-associated papillary conjunctivitis.
Differences in deposition patterns of lens materials may impact subjective comfort and dry eye symptoms by altering surface wettability and potentially altering tear stability characteristics. High-water-content materials are associated with significant tear film deposition. FDA Group 2 lenses are particularly prone to lipid deposition, whereas Group 4 lenses attract more protein than lipid species. Further, once tear proteins, such as lysozyme, firmly adsorb onto materials, the protein tends to undergo conformational changes and to denature.
The clinical relevance of protein denaturation on hydrogel lenses relates to the impact of this protein on inflammation and lens comfort. Previous studies suggest that protein denaturation is closely linked to inflammatory conditions such as giant papillary conjunctivitis. In addition, recent work from our group suggests that even over a short period of wear, protein denaturation can impact lens comfort, with little correlation to total amounts of either lysozyme or total protein. Therefore, it is important that practitioners emphasize the importance of lens disinfection and cleaning and appropriate lens replacement schedules. Moreover, practitioners should advise patients to rehydrate lenses with rewetting drops to keep the lens surface wettable, because proteins exposed to hydrophobic surfaces are more likely to denature. This could result in reduced comfort.
Wettability It is generally agreed that patient perception of comfort is linked to the ease with which the tear film spreads over the front surface of the lens. This surface layer helps to lubricate the interaction between the surface and eyelid. All hydrogel lenses exhibit a gradual reduction in comfort and wettability over time (Figure 1). Frequently replaced lenses produce enhanced subjective performance as compared with traditional materials. The reasons behind improvements in subjective performance and reduced clinical complications are potentially due to reduced material deposition and the maintenance of material front-surface wettability. However, the exact reason remains unclear. It is possible that the tear film-derived biofilm initially deposited on hydrogel lenses reduces frictional forces between the lens and ocular surface, enhancing initial comfort.
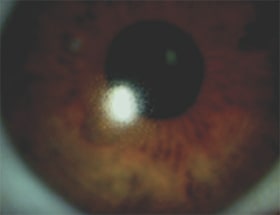
PHOTO COURTESY OF DR NANCY KEIR, CCLR, WATERLOO
Figure 1. Contact lens showing poor wettability.
Subsequent deposition of tear-film derived material serves only to reduce wettability, probably due to denatured protein or increasing accumulation of non-wetting lipid. This produces areas of hydrophobicity, resulting in further deposition and comfort problems.
If patients' lenses exhibit reduced wettability, then changing to another lens material will likely have a minimal impact. Such patients are best managed by switching to lenses that are replaced more frequently, ideally with daily disposable lenses or by prescribing rewetting drops that contain surfactants.
Reduced End-of-Day Dryness, Discomfort?
Although issues of discomfort develop soon after lens application or during the first week after switching from hydrogels to silicone hydrogels, several clinical studies have found that patients wearing silicone hydrogels report higher levels of comfort.
A recent study by Chalmers and coworkers (2009) who investigated the questionnaire responses from 699 hydrogel and 183 silicone hydrogel lens wearers found that fewer silicone hydrogel lens wearers reported dryness and discomfort at the end of the day compared to those wearing hydrogel contact lenses. Similar results were reported in previous studies by other researchers.
Chalmers and coworkers also showed that in dry air or smoky environments, comfort was significantly better for the silicone hydrogel lens wearers than for the hydrogel lens wearers. This is likely because silicone hydrogel lens materials are less prone to evaporation in typical or dry environments, possibly due to their lower water content, and they may also absorb fewer airborne pollutants compared with higher-water-content lenses. Moreover, silicone hydrogel lens wearers also reported better comfort after napping or sleeping while wearing their lenses, and silicone hydrogels appear significantly better for those younger than 30 years old. Thus, the evidence to date seems to suggest that patients wearing silicone hydrogel lenses report increased comfort and reduced dryness when compared to those wearing hydrogel contact lenses.
Patient-Related Factors
Several patient-related factors influence lens wear.
Gender Women report dry eye more frequently than men do. Previous studies indicate that women are more prone to report increased dryness potentially due to hormonal fluctuations that may affect their dry eye status. These contributing factors for hormonal fluctuations in women include monthly menstrual cycling, oral contraceptive use, menopause, and use of hormone replacement therapy. Women may also report dry eye more frequently because they are more likely to report symptoms of disease than are men.
It is also of interest to note that patients who frequently use over-the-counter pain medications, oral antihistamines, and anti-depression medications were more likely to self-report dry eye.
Tear Film-Related Factors Successful lens wear depends on a stable tear film, including the production and maintenance of the constituents in each of its layers. Several factors impact the structure of the tear film including environmental conditions, lens parameters, tear film factors, and wearing schedules. This, in turn, may have clinical consequences such as contact lens-related dry eye symptoms, lens adherence, reduced tear exchange, contact lens dehydration, corneal desiccation, and inflammatory events.
Osmolarity Osmolarity is a quantitative measure of the amount of dissolved solutes in a solution. Tear hyperosmolarity is regarded as the central mechanism causing ocular surface inflammation, damage, and symptoms, as well as the initiation of compensatory events in dry eye.
Tear hyperosmolarity arises as a result of water evaporation from the exposed ocular surface in situations of low aqueous tear flow or as a result of excessive evaporation, or a combination of these events. Therefore, osmolarity is often considered to be a gold standard diagnostic test. Gilbard and coworkers (1986) suggested that increased osmolarity is the hallmark characteristic of contact lens-related dry eye. A recent study by Nichols and Sinnot (2006) also showed that an increase in tear film osmolarity is significantly associated with dry eye status. The average osmolarity for those who have dry eye was higher than for those who do not have dry eye (307.66mOsM versus 297.06mOsM).
Pre-Lens Tear Film Thinning Time Nichols and Sinnot (2006) showed that pre-lens tear film (PLTF) thinning time was most strongly associated with dry eye, and they showed that the PLTF was faster in those who have dry eye (8.23 ± 5.67 seconds) than in those who do not have dry eye (11.03 ± 8.63 seconds). Tear film thinning times differ depending on the tangential flow or dewetting of the fluid due to surface tension gradients of the film or hydrophobic regions on the lens surface.
From a clinical perspective, it is important for the lens material to remain "wetted" with a consistent tear film over its surface to provide good comfort, vision, and lubrication and to prevent surface drying. One previous study demonstrated that a non-wet-table material shows a quicker PLTF thinning time, as a wettable film spreads uniformly without breakup. Research has also shown that the pre-lens lipid layer thickness is lower in dry eye subjects, and this correlated well with the pre-lens tear film thinning time. This, together with poor lens wettability, could be a basis for a higher evaporative loss during wear, resulting in dryness symptoms in lens wearers.
Tear Film Breakup Time (TBUT) When a lens is applied, it disturbs the tear film and significantly reduces tear film breakup time. Previous studies have indicated that the non-invasive TBUT is significantly reduced in symptomatic wearers as compared to asymptomatic contact lens wearers when evaluated over the course of a lens wearing day. This suggests that contact lens wearers who have lower TBUT are more likely to report symptoms of dry eye when compared to lens wearers who have higher TBUT.
Tear Film Composition Glasson and coworkers (2002) found that symptomatic contact lens wearers have significantly increased levels of secretory phospholipase A2, more lipocalin, increased lipases, and degraded lipids in their tears when compared to asymptomatic lens wearers. The clinical relevance of these tear film changes is that they were associated with increased dry eye history and symptom scores. In a subsequent study by the same group, it was found that tear volume (meniscus height and phenol red thread test) and tear stability (TBUT) was significantly reduced in symptomatic wearers compared with asymptomatic wearers. The symptomatic (or intolerant) wearers also reported a greater number of symptoms. The researchers concluded that intolerance was more accurately predicted by symptoms and clinical measures of the tear film, but not by protein characteristics of the tear film.
Environmental Factors In a dry environment such as hot desert-like conditions, artificially heated environments, and during winter months, humidity levels are significantly reduced. Contact lens wear in such dry conditions will most likely exacerbate dryness symptoms or may cause symptoms in patients who are usually asymptomatic. Maruyama and coworkers (2004) reported that dry eye symptoms worsened in soft contact lens wearers when environmental humidity was reduced. It is likely that the heated dry environment causes quicker and greater lens dehydration, leading to symptoms. Patients who complain of contact lens-related dry eye due to such environmental conditions would benefit by rehydrating their lenses with rewetting drops.
Rewetting Drops for Symptomatic Relief
During contact lens wear, the pre-contact lens tear film evaporates more quickly than the pre-corneal tear film does, regardless of lens material or water content. This dehydration or evaporation results in lens intolerance expressed as dryness. Patients can use rewetting (or comfort) drops to temporarily alleviate discomfort caused by dryness.
Although rewetting drops provide relief from these symptoms temporarily, currently there is no rewetting drop that can provide sustained comfort and relief from dry eye symptoms over the course of an entire wearing day.
Despite the addition of viscosity-enhancing ingredients, rewetting drops once instilled into the eye tend to have a short ocular residence time. The drops drain through the patient's nasolacrimal duct quickly after instillation, with the remainder being quickly absorbed by the cornea, conjunctiva, and nasal mucosa — with at least a 90-percent loss for each application. Therefore, rewetting drops have to be re-instilled throughout the day to provide effective comfort.
A study by Chalmers and Begley (2006) suggested that the most frequent and effective treatment used by lens wearers to relieve dryness symptoms was lens removal. Other treatments (rewetting drops, artificial tears) were used less often and did not deliver the same relief.
Currently available rewetting drops incorporate one or more wetting agents that will enhance lens surface wettability, thereby reducing the dryness sensation. These rewetting agents typically contain a wetting ingredient such as a surfactant, ocular demulcent, or sodium hyaluronate.
Surfactant-containing lens lubricants include Alcon's Opti-Free Replenish rewetting drops, which contain a variety of surface active agents (Tetronic 1304 and polyethylene glycol-11 lauryl ether carboxylic acid), and Abbott Medical Optics' Complete Blink-N-Clean lens drops, which use tyloxapol to clear away ocular precipitates that can cause irritation and discomfort.
Ocular demulcents in rewetting agents include carboxymethylcellulose (found in Allergan's Refresh Contacts comfort drops), povidone (found in Bausch & Lombs's ReNu MultiPlus rewetting drops), hydroxypropyl methylcellulose (found in Pfizer's Visine for Contacts rewetting drops), and glycerin (found in Pfizer's Visine for Contacts rewetting drops).
Impact of Lens Care Solutions
Over the last few years, multipurpose soft lens disinfecting solutions have gradually evolved toward simpler regimens that incorporate several components in an attempt to improve comfort, enhance water retention, and improve surface wetting properties of contact lenses. Currently available lens care solutions incorporate different wetting agents such as a surfactants or ocular demulcents. The most common surfactants found in lens care solutions consist of two distinct groups — poloxamines sold under the trade name Tetronic and poloxamers sold under the trade name Pluronic. Current or previous ocular demulcents found in lens care solutions include hydroxypropylmethylcellulose and propylene glycol.
Acon's Opti-Free Replenish was designed to enhance lens comfort by retaining moisture on the lens surface. It contains Tetronic 1304, a surfactant that helps lenses retain moisture, and C9-ED3A (nonanolyethylenediaminetriacetic acid), a novel surface active wetting agent. This combination of Tetronic 1304 and C9-ED3A forms the proprietary reconditioning system trademarked as TearGlyde. These components apparently work together with natural tears to retain moisture at the lens surface during the course of the day.
CIBA Vision's Focus (SoloCare) Aqua (Aquify in the United States) product includes dexpanthenol (which acts as a wetting and lubricity-enhancing agent) and sorbitol (which is used to aid lens wetting). Sorbitol, in combination with dexpanthenol, is the basis for the "Hydrolock effect" in Focus (Solo-Care) Aqua lens care solution.
Hydrogen peroxide solutions are considered as the gold standard for disinfecting lenses. However, when residual peroxide is present on the lenses in sufficiently high concentration, it can be toxic to the cornea and can cause discomfort unless neutralized to a concentration of less than 100 ppm (the subjective sensitivity threshold range being 50–300 ppm). Nevertheless, when peroxide-based systems are used at the right concentration, studies show that they can provide improved comfort in contact lens wearers.
Conclusions
A review of the literature on various factors influencing contact lens-related dry eye clearly indicates that the condition is multifactorial.
The contact lens industry has made strides in developing novel materials that provide improved comfort to patients. The industry has also developed a wide variety of lens care solutions and rewetting agents that incorporate novel ingredients that could rehydrate lenses and help alleviate symptoms. We have a range of lenses, care solutions, and rewetting agents that we can prescribe to patients who present with discomfort and dryness symptoms. CLS
To obtain references for this article, please visit http://www.clspectrum.com/references.asp and click on document #164.



