reader and industry forum
Refitting Keratoconus Patients: Explaining The Missing Diopter
BY BEZALEL SCHENDOWICH, OD, FIACLE
Drs. John Mountford and Don Noack in their "Instruction Notes to The KBA Lens" (2002) describe "The Missing Diopter" conundrum in these words:
"In approximately 15 percent of cases, you will be astounded to find an ‘extra’ +1.50D (ranges from 0.75D to 2.00D) after the first week of wear."
The "extra +1.50D" they refer to is an unexpected +1.50D over-refraction with the finished lens. Let's see if we can understand why this occurs.
Monitoring Progression
One of the pathognomonic aspects of keratoconus is that it progresses. The progression fascinates and intrigues contact lens fitters as we try to keep pace with the ectating cornea. In no smaller way does the progression of keratoconus baffle and frustrate patients.
Our work as eyecare providers begins with the diagnosis of the disease; continues with the support we can provide as sources of knowledge about the condition and its treatment options; and, in the case of corneal ectasias, further continues with the fitting and modifying of contact lenses for restoring visual acuity.
From time to time even successful contact lens wearers who have keratoconus complain that their lenses have become uncomfortable or that vision with them has deteriorated. In many cases a careful examination of the "offending" lens will prove that it is, in fact, intact. What remains to be investigated is the current corneal contour.
Many keratoconus patients are quite sensitive to the fact that their corneas will change shape from time to time. They will ask at follow-up visits whether any change has occurred. My answer is that there are two ways to identify corneal change: directly and indirectly. Generally, by the time we've reached this stage of the exam, I can answer qualitatively from indirectly gleaned information such as over-refraction, fluorescein pattern evaluation, change in lens movement and position, and even from apical staining patterns.
I describe to patients what I have learned and suggest that to answer the shape-change query more quantitatively from direct evidence, we need to remap the topography of their corneas.
But wait. We are discussing shape changes in thin, malleable corneal tissue. This means that if the corneal ectasia has in fact progressed, then what we will actually be measuring by topography or even keratometry will more likely approximate the shape of the posterior side of the contact lens just removed rather than serve as a true measure of the "natural" corneal shape.
Give it a Rest
The only way around this problem is a prescribed three-day rest from contact lens wear. Performing corneal topography upon removal of the lenses and again after the rest period often quite dramatically demonstrates that the "old" lenses are much flatter than they ought to be.
Figure 1 presents a pair of topography images taken 18.5 hours apart and their difference map. The lens for this eye was so flat that it was "restraining" the cone by 17.00D. A second day without the lens before mapping might well have shown an additional 5.00D to 8.00D of relaxation.
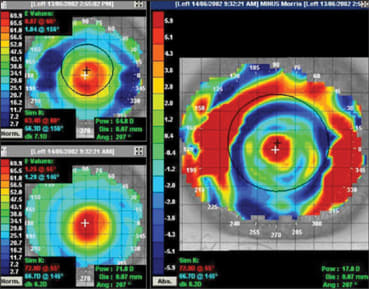
Figure 1. The effect of only 18.5 hours without a contact lens on a keratoconic cornea. The previous lens was far too flat fitting on this eye. The shape change is 17.00D (Mountford and Noack, 2002).
Three days is arbitrary. It is a period of time not so long that it is difficult to achieve, but almost long enough to allow the cornea to relax into its natural profile. I do this with the understanding that I want to avoid apical touch or bearing, and the only way to do this when fitting a corneal lens is to determine the shape of the ectasia that represents its state of most advanced progression.
Managing the Follow Up
So far, so good. Or is it? Let's review. Our patient has returned to the clinic after three days of no lens wear, and we escort him to the slit lamp to view the apex of his cornea under moderate magnification and with fluorescein. Be sure to look for grainy irregularities and traces of superficial punctate keratopathy. These remnants of signs of excessive bearing and rubbing are indicators that your topography images will be smeared at best and spotty at worst unless you instill a moderately viscous artificial tear prior to imaging. The drops will smooth the cornea and allow the mapping software to calculate contours more accurately.
Now, we map. You can compare your new results to those taken immediately upon removal of the lenses at the previous visit. You can see the effects of corneal warpage/molding and perhaps begin to appreciate how much your refitting efforts are likely to be healthful to the corneas in question. At this stage you can also access your contact lens fitting module to gain a first approximation of the lens shape for which you are now aiming.
We go through our fitting routine and prescribe new, steeper, and generally more highly eccentric contact lenses. Our patient, mean-while, will need to be wearing some contact lenses until his new ones arrive for dispensing. The choices are generally pretty specific — we typically do not have reserve lenses or loaner lenses close to keratoconus prescriptions in stock. The patient will need to use his old lenses for the interim period.
This presents a major problem in patient management. The patient's old lenses will give him great vision: they are flat and reduce much of the surface irregularities of his corneas when he wears them. They also may have a temporary orthokeratologic effect that he will miss with his new lenses.
His new lenses, when they are dispensed, will immediately show pooling centrally where they are relatively much steeper, and they will not be particularly comfortable. The pooling will result in smeary vision and (hopefully) a minus over-refraction. Sometimes, even though less than the sharp vision to which the patient had been accustomed, he will see with a plano over-refraction.
Now, let us consider what will happen as he begins to wear his new lenses. Over the first few days his corneas will once again reshape towards the curvature for which we prescribed these lenses. As that happens, the "plus" tear lens reduces; his need for a minus over-refraction reduces as his corneal shape more closely matches his new lenses.
In many cases, the refit scenario may yield a "plus" over-refraction after the eyes settle-in to the structure of the new lenses. Delay final lens alterations, therefore, until after 10 days to two weeks of lens wear.
If, on the other hand and through some accident, the new lenses provide acceptable visual acuity without over-refraction when dispensed, then as corneal molding resolves a plus over-refraction will become evident.
Perhaps we can find the solution to the Mountford-Noack riddle of "The Missing Diopter" in their excellent contact lens design and prescription technique. CLS
Dr. Schendowich is a Member of the Medical Advisory Board of the National Keratoconus Foundation, USA, a Fellow of the International Association of Contact Lens Educators, and an adjunct assistant clinical professor of optometry at SUNY-Optometry in the ophthalmology clinic at the Sha'are Zedek Medical Center in Jerusalem, Israel.



