GP insights
Fitting Front-Surface Toric GPs
BY ANN LAURENZI, OD, FAAO
When a patient's refractive astigmatism is greater than his corneal astigmatism, residual astigmatism (RA) is present. RA can also be measured by applying a spherical contact lens to correct the ametropia and then performing a sphero-cylindrical over-refraction.
One option to correct RA with a spherical GP contact lens is with an astigmatic spectacle prescription worn over the lens. However, you can also fit unsuccessful soft lens wearers or patients who want freedom from spectacles in a front-surface toric GP lens.
The GP Option
The structural stability of GP contact lenses makes them a valuable alternative for front toric lens design. Although this type of GP is not fit often, recognizing and properly fitting RA with a front-surface toric benefits patients who need full correction for optimal vision.
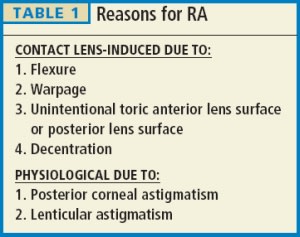
We refer to RA as having a physiological etiology from the posterior cornea or the crystalline lens. However, the contact lens itself can induce RA (Table 1).
You can check flexure by overkeratometry readings and usually correct it by increasing center thickness and making sure the lens is not too steep or too flat.
A front-surface toric GP contact lens has the patient's RA correction ground onto the front lens surface. The following are some considerations for optimizing the fit.
Fit requirements should include a well-centered lens. Adjust the base curve radius (BCR) until you achieve this, which may be with a slightly steeper BCR than in a traditional spherical GP contact lens. A slightly smaller overall diameter with a larger than average optic zone can also aid in centration.
The rotational stability of the lens is also important. Prism ballasting (adding a small amount of prism) helps the orientation of the anteriorly ground-in cylinder correction.
Typically the prism requirement for moderate-to-high minus lenses is 0.75PD to 1.00PD, and it's up to 1.50PD for low minus and plus lenses. Adding prism increases lens thickness, so a use a higher-Dk material.
The rotational stability of the lens is mechanically influenced by the lid/lens interaction. The blink usually rotates the lens 10 degrees to 15 degrees nasally in a prismballasted lens. You can incorporate the rotation into the lens order if you use a spherical lens and perform a cylindrical over-refraction. However, a more accurate way to determine the exact rotation and power is to order a spherical lens with the appropriate sphere power and prism ballast and have the laboratory mark the prism-base apex.
Apply the contact lens and let it settle. I usually let it settle for more than 15 minutes and try to verify the rotation several times. Approximate the rotation, perform a sphero-cylindrical overrefraction and use this to order the lens with the correct astigmatic power. Apply the LARS rule to adjust for rotation. If the lens is rotationally unstable with prism ballasting, truncation can be added.
Remember to Check for RA
If a patient comes to you wearing a spherical contact lens prescription and has less than 20/20 VA or has asthenopic complaints, fatigue, or ghosting, remember to do a sphero-cylindrical over-refraction to check for RA. If you find RA, use the proper contact lens to fully correct the prescription. CLS
Dr. Laurenzi currently has a staff position at NorthShore University Hospital in Glenbrook, Illinois.



