Online Photo Diagnosis
By William Townsend, OD, FAAO
A 64-year-old female presented with complaints of foreign body sensation in her left eye that she first experienced after undergoing a facial microdermal abrasion. She had self-treated the condition with over-the-counter artificial tears for six weeks, but continued to be symptomatic. The pain was severe enough to wake her up at night. She stated that during these episodes it was difficult for her to open her eyes.
Her health history was significant for type I diabetes that was controlled by diet, Crohns' disease, and bronchitis. Her current medications included ibuprofen and multivitamins. Best-corrected visual acuities were 20/20 OU. Pupils were equal in size and reacted briskly without APD.
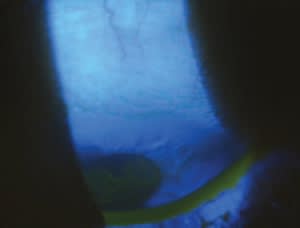
Initial biomicrocopic findings were unremarkable, but after lifting the patient's eyelid, we observed the lesion seen in the superior cornea of the left eye. We noted no change in its appearance after each blink. In the right eye were small irregular linear formations at the level of the epithelial basement membrane. No staining was apparent.
Assessment
This patient suffers from recurrent corneal erosion syndrome (RCES) in the left eye secondary to corneal epithelial membrane dystrophy (CEMD) and possibly corneal trauma. In a retrospective study of 104 individuals presenting with RCES, Reidy et al (2000) found that a history of trauma was present in 47 patients (45 percent). They also found that 30 patients (29 percent) had epithelial basement membrane dystrophy (EBMD) and 18 patients (17 percent) had a history of trauma and evidence of EBMD. The vast majority (87 percent) of lesions were located in the lower third of the cornea. Seventy percent of the subjects were females.
Trauma is the initiating factor in many patients who have RCES, especially trauma from a scratch that damages or destroys the corneal basement membrane. Ultrastructural changes identified as reducing adhesion of the corneal epithelium to the underlying basement membrane include a deficient epithelial basement membrane, the absence or abnormality of hemidesmosomes, and loss of anchoring fibrils extending from the basement membrane into the anterior stroma. Nocturnal lagophthalmos is reportedly associated with RCES (Sujata, Seitz, 2008).
The superior location of our patient's lesion is somewhat unusual, and the upper lid initially hid it. In cases in which patients present with symptoms suggestive of RCE, elevate the lids "just in case."

Managing RCE
Management of RCE ranges from conservative measures such as hypertonic drops and ointment at bedtime to procedures such as stromal micropuncture and phototherapeutic keratectomy (PTK). We treated this patient with Muro 128 5% ointment (Bausch & Lomb) at bedtime and artificial tears during the day. She continues to be free of symptoms. Most cases respond to conventional therapy, but in recalcitrant cases more aggressive measures are justified. The FDA labeling for the excimer laser specifies EBMD and irregular corneal surfaces as two of multiple indications for PTK.
Recurrent erosion is a painful condition that typically occurs in the inferior quadrants of the cornea and may be secondary to trauma or corneal dystrophy. As this case demonstrates, it may lie hidden beneath the upper eyelid.
References
- Reidy JJ, Paulus MP, Gona S. Recurrent erosions of the cornea: epidemiology and treatment. Cornea. 2000;19:767�771
- Sujata S, Seitz B. Recurrent Corneal Erosion Syndrome. 2008 Surv Ophthalmol 53:3-15.



