EMPIRICAL FITTING
Empirical Fitting of GP Multifocal Lenses
Diagnostic Fitting is a thing of the past for some GP multifocal contact lens designs.
By Douglas P. Benoit, OD, FAAO

Dr. Benoit practices in a multi-subspecialty ophthalmology group in Concord, NH. He is a Diplomate of the Section on Cornea, Contact Lenses and Refractive Technologies of the American Academy of Optometry. He is currently vice-chair of the Section. |
Sometimes it takes awhile for practitioners to embrace change. I would certainly be in that group when it comes to diagnostic fitting versus empirical fitting of GP contact lenses. As anyone who knows me can attest, I have been a proponent of diagnostic fitting especially for GP multifocal contact lenses. Back in the days when I lectured on GP lenses for the Gas Permeable Lens Institute's Schools Program that was sponsored by the Contact Lens Manufacturers Association, I used to debate Dr. Keith Ames (an empirical fitting advocate) about the merits of diagnostic fitting versus empirical fitting. I went so far as to say that empirical fitting was really just a delayed diagnostic fit. But with the advent of new technology and new contact lens designs, my mindset with regard to this issue has changed.
Newer designs for both soft and GP multifocal contact lenses make fitting from diagnostic sets impractical, unnecessary, or both. A case in point from the soft lens world is the Proclear Multifocal Toric lens from CooperVision. The vast parameter range for the toric component, coupled with the various multifocal add powers available, would make a comprehensive diagnostic set essentially impractical. With the custom nature of that lens design, it makes far more sense to order a trial lens from the refraction and keratometric readings.
GP Multifocal Designs
On the GP multifocal side, new designs are so easy to fit relative to their predecessors that diagnostic sets are far less mandatory. One example is the Menifocal design from Menicon. This concentric, simultaneous image lens has a central distance vision zone, a transition zone, and then a peripheral near vision zone. It is manufactured in the Menicon Z material, which has a Dk of 163. It has base curve radii of 7.00mm to 9.00mm in 0.10mm steps, three standard overall diameters (9.8mm, 9.6mm, and 9.4mm), distance powers of +5.00D to –13.00D in 0.25D increments, and four add powers (+1.00D, +1.50D, +2.00D, and +2.50D). You can easily fit this lens by following the fitting nomogram from the laboratory, and the results are quite good. Remember that this lens needs to center in primary gaze and translate up on downgaze for best results.
Another GP multifocal contact lens that you can fit empirically with high success is the ReClaim HD multifocal from Blanchard Contact Lens. This lens is a bi-aspheric, simultaneous image design in the Boston ES (Bausch & Lomb) material. The parameter range is large, with standard parameters that the company estimates will fit the majority of your presbyopic patients.
Base curve radii range from 7.00mm to 8.30mm in 0.05mm increments, and overall diameters range from 8.80mm to 10.2mm in 0.10mm steps. Distance powers are –20.00D to +20.00D in 0.25D steps while the three standard add powers are progressive to +2.00D with a 3.5mm anterior distance zone size; up to +2.50D with a 3.0mm anterior distance zone; and up to +3.00D with a 2.5mm anterior distance zone. There are even custom parameters for the add powers and anterior distance zone sizes if needed.
You can fit ReClaim HD by using the fitting guide that is available for download from the Blanchard Web site or by using the fitting calculator on the Web site itself. This design also needs to be relatively centered in primary gaze (some lid attachment is good) to ensure proper translation on downgaze. Figure 1 shows a well-fit ReClaim HD lens.
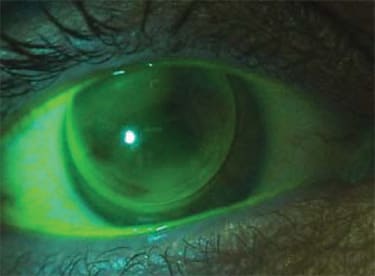
Figure 1. A well-fit ReClaim HD GP multifocal lens.
For a translating or alternating image design, you can empirically fit the MetroSeg Crescent Segment Bifocal (Metro Optics) lens with relative ease. The segment's crescent shape allows the lens to rotate up to 30 degrees without disrupting vision. The design is thin and comfortable due to the minimal prism ballast used. The parameters are basically unlimited, which makes diagnostic fitting impractical because having a diagnostic lens that is close to a patient's needs in all the areas of concern would be unlikely.
Fitting and Evaluation Pearls
As with all multifocal contact lenses, certain information must be acquired to guide you to the proper design for each individual patient. A good refraction for distance and near, plus keratometric readings is the minimum data needed. Without this information, good vision and a good fit would be impossible. Of course a thorough slit lamp examination to assess external eye health as well as tear film quality and quantity is required. It also helps to know which eye is dominant, how the lids position relative to the limbus, how tight the lid apposition is, and the size of the pupils in average room light and dim light.
The slit lamp examination will alert you to problems such as blepharitis and other lid abnormalities that could interfere with comfortable lens wear. These issues need to be managed prior to the actual fitting process.
The position of the lower lid relative to the lower limbus is also very important to know. If the lower lid is tangent to or slightly above the lower limbus, both a translating design and a simultaneous image design could be successful. However, if the lower lid positions below the lower limbus (Figure 2), lens translation on downgaze could be a problem for alternating image/translating designs. For such cases, the simultaneous image designs, both concentric and aspheric, would be the better choice.

Figure 2. A translating design may be problematic when the lower lid lies below the limbus.
How tight the lids are to the globe, also known as lid apposition, is also a consideration. If the lids are too flaccid, which they can become as we "chronologically mature," a GP lens may not move properly with downgaze, leading to poor translation and therefore inadequate near vision.
The size of the pupils can help guide you to the best design to use. Pupils that are very large (5mm or more) in average illumination will be, of course, even larger in dim light. A concentric design, and even some aspheric designs, might be inappropriate in such patients as the pupil could be larger than the distance zone size of the lens, leading to flare and glare from lights. This can be particularly problematic when driving.
That leaves the consideration of eye dominance. It helps to know which eye is dominant with most multifocal contact lens designs. The dominant eye usually needs the best distance vision to allow for easier adaptation to this type of correction. A few different methods can help you determine eye dominance. You can alternately place a +2.00D loose lens before each eye and see which eye tolerates the blur better while viewing a distant object. The one that accepts the plus power more readily is the nondominant eye. Another technique for assessing eye dominance is the "hole-in-the-hand" test. Here patients make a small opening with their hands and extends them at arms length while viewing a distant object. Each eye is then covered in turn, and the eye that still sees the object is the dominant eye.
A Representative Case
A recent patient case illustrates just how straightforward empirical fitting can be. Our patient, a 49-year-old financial consultant, presented for a routine yearly eye examination. At that time he felt that his near vision was becoming a problem and he did not want to wear reading glasses over his contact lenses. His distance vision was fine, but he noted slight comfort issues as the day progressed. His general medical health was normal. His current GP lenses were an aspheric, single vision design with the following parameters: OD 7.55mm base curve radius (BCR), 9.2mm overall diameter (OAD), and –2.75D power; OS 7.50mm BCR, 9.2mm OAD, and –2.25D power.
The results of his examination showed 20/20 distance vision OD, OS, and OU. Near vision was 20/30-2 OD, OS, and OU. Both contact lenses were slightly scratched but clean. Each had a superior central, lid-attachment fit with good movement in all positions of gaze. Fluorescein evaluation showed a trace apical clearance pattern with good peripheral clearance. The cornea was free of superficial punctate staining. The remainder of the examination was unremarkable.
The manifest refraction resulted in the following: OD –3.00 –0.25 × 104, add +1.50D; OS –2.50 –0.50 × 122, add +1.50D. His keratometric readings were OD 44.87/44.62 @ 90; OS 45.25/45.25 @ 90
The fitting calculator on the Blanchard Web site determined the following lens parameters to be appropriate: OD 7.50mm BCR, 9.5mm OAD, –3.50D, +2.00D Add/3.5mm anterior distance zone; OS 7.55mm BCR, 9.5mm OAD, –2.75D, +2.00D Add/3.5mm anterior distance zone. The add power required determines which anterior distance zone to use, as described previously.
The lenses were ordered in the standard Boston ES material with a plasma treatment. At dispensing the patient noted great initial comfort and attained 20/20 vision in each eye at distance and near. With slit lamp examination, both lenses had a superior central, lid-attachment fit in primary gaze, with good translation up on downgaze and smooth movement over the corneal surface in all positions of gaze. The fluorescein pattern was optimal with slight apical clearance and good peripheral clearance. We dispensed the lenses with Boston Simplus (Bausch & Lomb) solution and scheduled the patient for a oneweek follow-up visit. At that appointment, the patient reported great comfort and vision at all distances. Visual acuity and slit lamp examination findings were the same as at the dispensing visit.
Summary
This is but the most recent example of how successful these lenses can be when fit empirically, based on the laboratory recommended nomogram. Where once I would have never pursued a multifocal case without a diagnostic fitting evaluation, I now can be confident that these lenses will work about 75 percent of the time on the first try. Think of it as ordering a custom diagnostic lens for every patient.
Empirical fitting improves time management at the start of the fitting process as well as in the follow-up phase because fewer visits are needed. Patients are happy to obtain workable lenses more efficiently as well. This is a true win-win situation that we all should embrace. CLS



