CORNEAL DYSTROPHIES
Corneal Dystrophy and Disease: Diagnosis and Management
A good family history and clinical resources will help you properly diagnose and manage corneal dystrophies.
By Jason Jedlicka, OD, FAAO, FSLS, & Evan Veire, OD
Corneal dystrophies are a widely varied group of conditions, generally defined as inherited, bilateral, symmetric, and slowly progressive (Sutpin, 2007). While not always entirely accurate, this gives us a good working definition upon which to discuss their diagnosis and management.
In clinical practice, we may find corneal dystrophy presentation to be stark or subtle. Patients can present with discomfort, blurred vision, or neither. Our job is to make a proper diagnosis so as to properly educate patients about the genetics, prognosis, and management options.
The first part of this article will focus on making the proper diagnosis based upon current classification methods. The second part will cover the options for managing these conditions as appropriately as possible.
Corneal Dystrophy Classification
Much of the classification of these conditions has evolved over time through clinical findings and evaluation of those affected within families. While often very accurate and useful, the historical classifications were not always backed by scientific research. With the availability of gene testing and improved histopathologic studies, the need for a more scientific classification of corneal dystrophies became apparent.
In 2005, the World Cornea Congress formed a committee, the International Committee of Classification of Corneal Dystrophies (IC3D), to develop a new classification system for corneal dystrophies. These results were published in 2008 as a supplement to the December issue of Cornea (Weiss et al, 2008). The IC3D developed a system that utilizes the understanding of the genetics of each condition to categorize the dystrophies. These categories are as follows (Weiss et al, 2008):
Category 1 A well-defined corneal dystrophy in which a gene has been mapped and identified and specific mutations are known.
Category 2 A well-defined corneal dystrophy that has been mapped to one or more specific chromosomal loci, but the gene (or genes) remain to be identified.
Category 3 A well-defined corneal dystrophy that has not yet been mapped to a chromosomal locus.
Category 4 Reserved for suspected new or previously documented corneal dystrophies, although the evidence for such dystrophies being separate and distinct is not yet convincing.
The most commonly used method for categorizing corneal dystrophies is by the layer of tissue in which they are located. These categories can be broken down into Epithelial and Subepithelial Dystrophies, Bowman's Layer Dystrophies, Stromal Dystrophies, and Endothelial and Descemet's Membrane Dystrophies. Table 1 outlines the various dystrophies by layer with inheritance and IC3D categorization (Weiss et al, 2008).

Diagnosing Corneal Dystrophies
When attempting to diagnose a corneal dystrophy, carefully consider the layers involved, the age of the patient, the family history, and the type of findings. Most corneal dystrophies have an early onset and are genetic, so when you see a young patient who has the findings of a corneal dystrophy, the parents are often already aware of the familial condition.
However, in situations in which this is not the case, careful evaluation of the types of findings and their location, along with some type of resource, can help you make the proper diagnosis. Table 2 lists corneal dystrophies along with onset, symptoms, and signs to aid in differentiating the dystrophies (Weiss et al, 2008).


It is said that a picture is worth a thousand words; the best way to diagnose a corneal dystrophy is often to compare the eye that you see with images of diagnosed corneal dystrophies. This allows you to match the cornea that you are examining to a variety of images to ensure the proper diagnosis. Figures 1 through 24 can be considered good examples of many of the dystrophies listed in the tables and may be a useful reference in making a diagnosis. All of these figures except for Figure 12 originally appeared in the December 2008 supplement of the journal Cornea and are reprinted with permission of The Cornea Society, Copyright 2008, all rights reserved.

Figure 12. Granular corneal dystrophy lattice).
In the end, you can base your diagnosis of a corneal dystrophy potentially upon the patient's symptoms and certainly upon your slit lamp observation, and hopefully you can corroborate it with the patient's family history in most cases. Using tools such as the photo atlas and table of clinical signs and symptoms can direct you to the proper diagnosis.
Managing Corneal Dystrophies
Once you have made the diagnosis, you have to decide how to best manage the affected patient. How you manage patients who have a corneal dystrophy depends on the severity of their symptoms. Many corneal dystrophy patients will have little or no ocular or visual symptoms and will thus require little or no treatment. For patients who do have symptoms, treatment options again depend on the layer of the cornea in which the disease is found and the type of symptoms the patient has.
In general, we can divide the management options into three categories: medical, contact lens-based, and surgical. We will explore the types of treatment in each category and the application for various dystrophies.
Medical Treatment of Corneal Dystrophies Topical medications are often a first line of therapy for many conditions. In patients who have corneal dystrophies and experience ocular discomfort that is mild, recommending lubricating eye drops is never a bad idea. Prescribe ocular surface lubricants as you always do, with consideration of the frequency of use and tolerance for blurry vision. In patients who have significant symptoms of erosions, a higher-viscosity drop may be more useful; however if the patient cannot tolerate the blur, more frequent use of a lower-viscosity drop may be required. Non-preserved tears are usually the best option because patients who experience symptoms will likely use the lubricants multiple times per day.
Antibiotic drops may be required during episodes of erosions that are significant enough to warrant coverage. While the antibiotic drops may do little to relieve the pain, they may help increase the rate of healing by preventing bacterial processes from hindering healing, especially in instances of open epithelium. Oral antibiotics such as doxycycline (50mg, two times a day) can be used along with topical corticosteroids (three times a day) in recalcitrant cases when all else has failed to allow an erosion to heal, often with remarkable results (Dursun et al, 2001).
In addition, topical steroids can be used in situations in which chronic photophobia, redness, and watering are issues, provided that you monitor the patient for potential side effects. Additionally, it has been documented that anterior stromal infiltrates can occur in cases of recurrent erosions and that topical steroids can be useful, safe, and effective in resolving these infiltrates (Tabery, 1998). Restasis (Allergan) may also be of value in patients who have milder symptoms of ocular discomfort, although no studies have been performed to demonstrate its effectiveness in patients who have corneal dystrophies.
Hyperosmotic agents may also benefit patients who have corneal dystrophies that have resulted in corneal edema. Using 2 percent or 5 percent sodium chloride drops periodically throughout the day or ointment at bedtime can help to deswell the cornea and improve visual acuity, as well as reduce the risk of bullae formation.
Contact Lens Treatment of Corneal Dystrophies Contact lenses can have a wide spectrum of application for corneal dystrophy patients, from soft lenses for recurrent erosions to GP lenses for visual rehabilitation, to scleral lenses for both of these reasons.
It has been demonstrated repeatedly that soft lens application to recurrent corneal erosions reduces patient symptoms and allows for better healing (Kanpolat and Ucakhan, 2003; Montero et al, 2003). The prevailing recommendation for using bandage soft lenses for recurrent erosions is to utilize an extended wear material and to leave the lens in place without disturbance for extended periods (Kanpolat and Ucakhan, 2003). This gives the corneal cells the opportunity to reestablish themselves without constant disruption either from the lids or from the manual removal and replacement of a lens.
High-Dk soft lenses can also be considered in cases of endothelial dystrophies when corneal edema leads to ruptured bullae and pain. This would likely be a temporary treatment until surgical intervention can occur, but remains an option for alleviating pain short-term.
It has also been documented that in certain circumstances, soft lenses can actually reduce the severity or prevent the recurrence of some corneal dystrophies. Lisch et al (2010) described the regression of Lisch epithelial corneal dystrophy with soft lens wear in two patients. Severin et al (1998) and Roters et al (2004) also describe cases of granular dystrophy in which soft lens use prevented recurrence post-penetrating keratoplasty. While this may not be a common use of soft lenses in managing corneal dystrophies, it is certainly an interesting application that may be worth considering in certain patients.
Scleral GP lenses can also be of great value in many of these conditions. In addition to improving acuity in instances in which surface irregularity is a component of the blurriness, it can improve the symptoms that are associated with compromised epithelium by creating a fluid chamber over the cornea. When fitted with enough corneal vault, the fluid chamber can facilitate comfort, epithelial healing, and better vision (Visser et al, 2007).
Surgical Management of Corneal Dystrophies There are many options for surgical management of corneal dystrophies, and the options continue to grow. Choosing the procedure again depends on the level of the dystrophy.
Anterior Stromal Puncture (ASP) has been utilized for many years for recurrent erosions. The theory behind the procedure is that epithelial tissue invades the puncture site into Bowman's layer and creates a firm epithelial anchor to the irregular lip of the stromal puncture (Smolin and Thoft, 2004). This is accomplished by use of a 20 to 27 gauge needle and creating 50-percent-depth perpendicular punctures to the corneal tissue through the loose epithelium, approximately 0.5mm to 1.0mm apart (Figure 25). The success rate is reported to be approximately 75 to 80 percent for eliminating recurrences (Smolin and Thoft, 2004; Reeves et al, 2010). Complications from the procedure are very rare, but can include corneal perforation if carelessly performed. In general, ASP can be utilized in cases of corneal dystrophy when recurrent corneal erosions occur with a reasonable safety profile and success rate.

IMAGE REPRINTED WITH PERMISSION FROM EMEDICINE.COM, 2010
Figure 25. Anterior Stromal Puncture with fluorescein.
Epithelial debridement also is a technique for treating recurrent erosions resulting from corneal dystrophy. Removing the weak, loose epithelium and allowing the cornea to rebuild the epithelium from scratch can help reduce recurrences as well. Similar to ASP, debridement alone seems to reduce recurrences to about 20 percent (Reidy et al, 2000).
While debridement alone can be effective at times, coupling it with excimer laser corneal resurfacing, or Photo Therapeutic Keratectomy (PTK), is a more common approach to treating recurrent erosions. Most studies demonstrate that PTK is a safe and effective way to reduce recurrences of erosions and to improve acuity in some cases, although a hyperopic shift should be assumed and accounted for in advance (Orndahl and Fagerholm, 1998). Success rates for PTK are reported in the range of 75 to 90 percent (Reeves et al, 2010; Orndahl and Fagerholm, 1998). PTK can also aid visual acuity in dystrophies in which superficial corneal opacities cause blurry vision or glare (Wagoner and Badr, 1999).
Corneal transplants are always an option for treating corneal dystrophies when symptoms are severe enough to warrant the procedure. In the past, full thickness grafts were the only good option. However, with the advent of more useful lamellar procedures, corneal transplants can be an option earlier in the course of treatment for some. Since many corneal dystrophies are confined mainly to specific layers of the cornea, a lamellar graft can be successfully utilized for some dystrophy patients.
Deep anterior lamellar keratoplasty (DALK) is a lamellar graft that involves removing the epithelium, Bowman's layer, and as much of the stroma as possible, while leaving the endothelium and Descemet's membrane intact. This procedure can be useful for dystrophies in which the anterior cornea is affected but the posterior cornea is in normal health (Salouti et al, 2009; Noble et al, 2007; Park et al, 2007). DALK involves a variety of techniques for removing the anterior cornea, but the goal is always the same: to get as deep as possible. The closer the transplant gets to Descemet's membrane, the better the visual outcome. The donor tissue is cut, the posterior corneal layers are stripped off, and the remaining tissue is sutured into place. Figure 26 shows an example of DALK before and after.

COURTESY OF MARK GOROVOY, MD
Figure 26. DALK for corneal scarring (left) before and (right) after.
DALK advantages include a reduced risk of rejection, as the endothelium is not foreign to the host; a somewhat more regular corneal surface compared to a full PK in some cases; and less endothelial cell loss. The primary disadvantages include decreased best-corrected acuity in many cases and the risk of perforation during the procedure (Jedlicka and Awad, 2010).
On the opposite end of the spectrum are the posterior lamellar grafts utilized in endothelial layer dystrophies, mainly Descemet's stripping automated endothelial keratoplasty (DSAEK) and Descemet's membrane endothelial keratoplasty (DMEK). The posterior lamellar grafts are now being performed at a rate equal to or greater than that of full grafts due to their quicker recovery and lower risk.
DSAEK involves removing the diseased endothelium and Descemet's membrane by simply stripping it manually and replacing it with donor tissue, which consists of endothelium, Descemet's membrane, and a thin layer of stroma. The donor tissue is prepared by use of an automated keratome (Figure 27). The DMEK procedure removes the diseased tissue the same way, but strips the same tissue off of the donor graft manually. By not transplanting any stromal tissue, the visual outcomes are improved; however, the complexity of the procedure is greater and the risk of graft slippage is higher at this stage of its evolution.

Figure 27. Three to six months post-DSAEK. Note the clear cornea and border of the endothelial graft.
Full thickness transplants are always an option for corneal dystrophy patients when a lamellar graft is not desirable. Consider referral for corneal transplant consideration when visual acuity is reduced to levels that make the procedure worth the risk. This will depend on a variety of factors, including the patient's age, visual demands, status of the better seeing eye, and complicating factors such as other preexisting ocular disease. Recurrence of dystrophic findings in corneal transplants are common, with rates reported at approximately 70 percent for any findings and 15 to 20 percent at five years for clinically significant findings including recurrent erosions and loss of vision (Marcon et al, 2003).
Take Charge of the Situation
Corneal dystrophies can be difficult to properly diagnose, particularly those that are less common. Careful family history, when available, should be very helpful in most cases, and examination of relatives may be of value as well. Slit lamp examination considering the layer(s) of the condition and the specific findings along with a corneal atlas should allow you to make a proper diagnosis.
Managing corneal dystrophies can be difficult as well, as most conditions deteriorate over time. Oftentimes the management involves resolving the symptoms of the moment and then waiting for the next episode to occur, or simply making the best of the situation with the options available. As things continue to deteriorate, surgical options can be utilized with generally good results, though recurrences should be anticipated in many cases, given enough time. Do not shy away from providing the proper care for these patients. If you demonstrate that you are willing and capable of managing these conditions, you may have the opportunity to care for other family members who have the same condition, which can be a rewarding experience. CLS
For references, please visit www.clspectrum.com/references.asp and click on document #181.
| Figures 1 through 24 are examples of many of the dystrophies and a useful reference in making a diagnosis | |
|---|---|

Figure 1. Map changes in epithelial basement membrane dystrophy. |

Figure 2. Epithelial recurrent erosion dystrophy. |
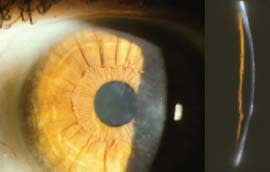
Figure 3. Subepithelial mucinous corneal dystrophy. |

Figure 4. Meesmann's corneal dystrophy in retroillumination. |

Figure 5. Lisch epithelial corneal dystrophy. |
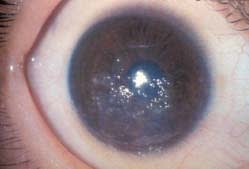
Figure 6. Gelatinous drop-like corneal dystrophy. |

Figure 7. Ries-Bucker's corneal dystrophy. |

Figure 8. Thiel-Benke corneal dystrophy. |
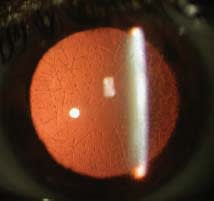
Figure 9. Lattice corneal dystrophy. |

Figure 10. Lattice corneal dystrophy, Gelsolin type. |

Figure 11. Granular corneal dystrophy type 1. type 2 (granular lattice). |

Figure 13. Macular corneal dystrophy. |

Figure 14. Schnyder corneal dystrophy early stage. |

Figure 15. Schnyder corneal dystrophy advanced stage. |

Figure 16. Congenital stromal dystrophy. |

Figure 17. Fleck corneal dystrophy. |

Figure 18. Posterior amorphous corneal dystrophy. |

Figure 19. Central cloudy dystrophy of Francois. |

Figure 20. Pre-Descemet's corneal dystrophy. |
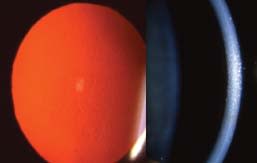
Figure 21. Fuchs' endothelial corneal dystrophy. |

Figure 22. Posterior polymorphous corneal dystrophy. |

Figure 23. Congenital endothelial corneal dystrophy. |

Figure 24. X-linked endothelial corneal dystrophy. | |

|
Dr. Jedlicka is the director of Contact Lens Services at the University of Minnesota Department of Ophthalmology and a partner at Consultative Eye Care, a referral-based practice in Wayzata, Minn. He is a clinical adjunct faculty member at the Pennsylvania College of Optometry and lectures on contact lens and anterior segment-related topics. You can reach him at jgjod@yahoo.com. |

|
Dr. Veire practices primary care optometry within a multispecialty medical group in St. Paul, Minn. He has special interests in anterior segment disease and contact lenses. You can reach him at eveire@hotmail.com. |



