SIHY LENSES AND THE TEARS
Short-Term Effects of Silicone Hydrogel Wear on the Tears
This study evaluated the effects on the tear film of wearing a silicone hydrogel versus a hydrogel lens.
By Jiang Zhenying & Qu Xiaomei, MD

Jiang Zhenying is an ophthalmologist at Eye & ENT Hospital Affiliated to Fudan University in Shanghai, China. |

Dr. Qu is the Deputy Chief Doctor at Eye & ENT Hospital of Fudan University. She is a member of the International Association of Contact Lens Educators and in 2002 was appointed as the China Coordinator of the organization. She is also the Chief Assistant of the Myopia Key Lab of the Ministry of Public Health; Commissary of the Optometry Association of China; and Deputy Team Leader of the Optometry Group of the Shanghai Ophthalmology Association. |
Corneal disease, such as microbial keratitis, is the most threatening complication for contact lens wearers associated with the use of hydrophilic soft lenses. In recent years, the occurrence of several contact lens complications has been reduced because of improved lens care solutions, improved contact lens materials, and the development and recognition of standard of care procedures for contact lens wearers.
However, some complications that have received less attention have been on the rise in frequency. Dry eye is one of the most common problems related to contact lens wear (Fonn, 2007; Lorentz and Jones, 2007), so the influence of contact lenses on the functions of the tears and the tear film has been of significant interest.
Most research in this area has suggested that contact lens-related dry eye may result from the loss of tear film stability. This instability results from increased tear evaporation secondary to lens dehydration and alterations to the lipid layer of the tear film. The severity of dry eye can depend on the lens material (higher material water content) or on patient factors (female gender) (Nichols and Sinnott, 2006; Ramamoorthy et al, 2008). One recent report (Guillon and Maissa, 2008) indicates that the effects of contact lens wear on the tear film's properties may last for 24 hours after lens removal. Naturally, dry eye is also related to the personal actions of the wearer, such as overwear of lenses, inappropriate care etc. (Nichols et al, 2005; Grus et al, 2005).
A Need to Further Evaluate Silicone Hydrogel Lenses
Since silicone hydrogel (SiHy) lenses with higher oxygen permeability entered the market, a great number of clinical trials have been performed globally with these lenses. One study demonstrated that signs and symptoms associated with corneal hypoxia in long-term wearers of traditional soft contact lenses are often effectively alleviated after switching to a SiHy lens that has high oxygen permeability (Riley et al, 2006). Other reports (Chalmers et al, 2005; Dumbleton et al, 2006) also indicate that refitting patients from a lens with low oxygen permeability to one with a high oxygen permeability can significantly mitigate the symptoms and signs of bulbar conjunctival congestion, corneal vasculariza-tion, and dryness and discomfort.
Although there is a close relationship between the sufficient oxygen supply to the cornea and the health of corneal tissues, it may not be optimal to use materials simply for their high oxygen transmissi-bility. Doing so may neglect the influence of other important parameters such as good tear exchange, which is also necessary for optimal and safe contact lens wear. Few clinical trials using SiHy contact lenses to date have shown that there is a relationship between high oxygen permeability and subjective comfort (Dillehay and Miller, 2007), and this class of materials represents a growing trend in material development and usage by practitioners (Stapleton et al, 2006). Therefore, this study was designed to determine the impact of a SiHy material compared to a traditional hydrogel lens material on the clinical tests associated with features of the tears.
Methods
Subjects The subjects provided Informed Consent, approved according to the tenets of the Declaration of Helsinki, and volunteered to wear the contact lenses provided according to the study requirements. The inclusion criteria for the study were as follows:
- 18 to 40 years old, male or female
- Spherical equivalence (SE) –0.50D to –9.00D
- Astigmatism <−1.00DC
- Best spectacle-corrected visual acuity (BSCVA) of 20/20 or better
The exclusion criteria for the study were as follows:
- Eye diseases, except for ametropia, that might influence the observation of this clinical research.
- Systemic diseases that might cause dry eye or that would complicate normal contact lens wear.
- Use of systemic or local drugs that might influence the study results.
- Rigid contact lens wear in the past six weeks.
- Ocular surface trauma or a history of surgery in the past eight weeks.
This study was conducted from October 2008 to January 2009 and included 30 volunteers—eight males and 22 females (mean age ± standard deviation = 26.9 ± 0.95 years). The spherical equivalence (SE) range was −1.50D to −6.00D (mean SE ± standard deviation = −3.57D ± 0.48D). Twenty-five subjects had myopic astigmatism <−1.00DC. The BSCVA of all subjects was 20/20 or better. We found no obvious diseases during routine examination of the anterior segment. There were no contact lens contraindications, dry eye symptoms or signs, or corneal staining.
Study Design One SiHy lens design and one hydrogel lens design from the same company were used in the study. Both were monthly replacement lenses and had been used in clinical practice with the same daily wear indications. The SiHy lens was balafilcon A (PureVision, Bausch & Lomb) with a water content of 36 percent and oxygen permeability of 110 (for a –3.00D lens). The traditional hydrogel lens used as a control was hilafilcon B (SofLens 59, B&L) with a water content of 59 percent and oxygen permeability of 22 (for a −3.00D lens). This was a prospective, controlled, randomized, investigator-masked clinical trial. Every volunteer was randomized to first wear one of the lens types on a daily wear schedule for eight hours each day over a wearing period of one month. Spectacle wear was not allowed during this period. A one-month washout period followed the first month of wear, then subjects switched to the other lens type for one month on the same wearing schedule. B&L provided ReNu MultiPlus as the study care solution.
The following examinations were performed on all the wearers before they wore the soft contact lenses and again at one week, two weeks and one month after wearing: uncorrected visual acuity (UCVA), BSCVA, refraction, slit lamp examination on the anterior segment and ocular fundus, and tear and tear film function examinations. At the end of each wearing period, the volunteers were asked to complete a subjective symptom rating form about the lens type worn during that wearing period. All of the subjects came from the same hospital, and all of the examinations were performed during the same time period to reduce any errors caused by other environmental factors.
Examination Methods We obtained study measurements both during lens wear and after removing the study lenses. All of the examinations were performed by the same examiner. Before the study, the examiner measured the tear meniscus area (TMA) using the anterior segment OCT (RTVue-100, Optovue Inc.) with the fourth-generation Fourier Domain technique. During the study, the TMA with lens wear was measured at each follow-up visit after subjects had worn the contact lenses for a period of eight hours.
Following the TMA measurement, the examiner removed the lenses and measured tear breakup time (TBUT) and corneal staining using fluorescein under the slit lamp. The examiner measured TBUT three times and calculated the mean value. For fluo-rescein staining, the cornea was divided into four quadrants (superotemporal, inferotemporal, super-onasal, inferonasal) and each quadrant was scored as follows: 0 points for no staining; 1 or 2 points for punctate and small patchy staining; 3 points for coalesced staining. The quadrants were summed (0 to 12) for analysis. After that, the examiner used Schirmer's test without anesthesia to measure the basic tear secretion. Both the test and control lenses were examined under the same conditions.
Subjective Evaluation After the first one-month test period, the volunteers completed the subjective symptom rating form about the lens type worn for that time period. The subjective symptoms fell into two groups—subjective comfort and vision—and the detailed evaluation items included foreign body sensation, sensation of dryness, asthenopia, and blurred vision. The subjects completed the rating form again after completing the second one-month test period with the other lens type. The evaluation form was scored on a 0 to 4 scale: 0 = no discomfort symptoms; 1 = between 0 and 2; 2 = there are mild symptoms sometimes, which can be mitigated in a short time; 3 = between 2 and 4; 4 = there are serious discomfort symptoms, which are frequent or persistent and influence daily life.
Statistical Analysis Stata10.0 software was used for statistical analysis. We used pairwise t-tests to compare the two groups and Wilcoxon symbol rank test for the data not meeting the assumptions associated with a t-test. A p-value of <0.05 was considered statistically significant.
Results
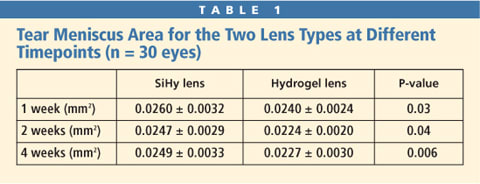
Comparison of TMA Our comparison of the TMA with the two lens types showed that there was a statistically significant difference in TMA between the SiHy lens and the hydrogel lens after one week, two weeks, and one month of wear (Table 1). The results showed that the tear meniscus height associated with the SiHy lens was significantly greater than that of the hydrogel lens at each timepoint.
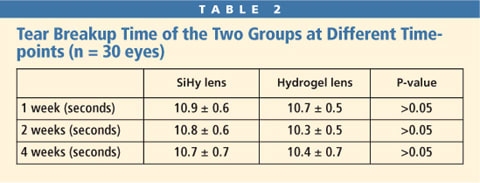
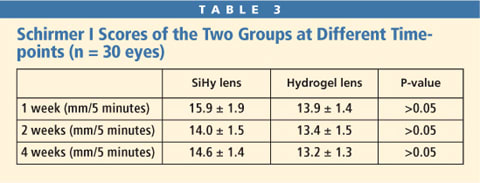
Comparison of Tear Film Breakup Time We compared the TBUT measured after the lenses had been removed at the different timepoints. There was no statistically significant difference in TBUT after lens removal between the SiHy lens and the hydrogel lens after one week, two weeks, and one month of wear (Table 2). Comparison of the Basic Tear Secretion The basic tear secretion of the two groups after lens removal at different timepoints was compared. There was no statistically significant difference in Schirmer I test results after lens removal between the SiHy lens and the hydrogel lens after one week, two weeks, and one month of wear (Table 3).
Comparison of Corneal Staining There were some cases of corneal fluorescein staining at the one-month timepoint in both groups. After wearing the SiHy lens, one subject developed corneal staining with a score of 3; after wearing the traditional hydrogel lens, two subjects had corneal staining with scores of 3 and 2, respectively. According to Wilcox-on test, there was no statistically significant difference between the two lens types.
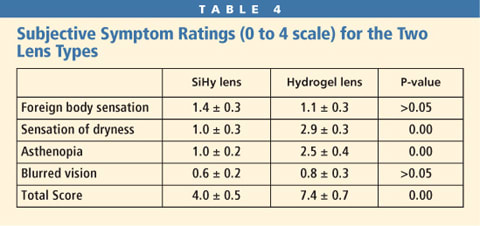
Comparison of Subjective Symptoms After wearing the two types of lenses, the volunteers completed the subjective symptom rating form, which evaluated four items including foreign body sensation, sensation of dryness, asthenopia and blurred vision (0 to 4 points for each item, 0 to 16 points total). The total score associated with SiHy wear was significantly lower than that associated with hydrogel lens wear (Table 4). The comparison results showed that the scores for sensation of dryness and asthenopia associated with the SiHy lens were significantly better than those for the hydrogel lens.
Discussion
A good tear film during contact lens wear is necessary for reduced ocular surface compromise, and evaluating the tear meniscus may be an important method for measuring the tear film. Since the anterior segment OCT with the fourth-generation Fourier Domain technique has been used in clinical practice, it has enabled clinicians to observe changes in the physiological values of the tear menisci in front of the lens during soft lens wear. Recent studies have demonstrated that OCT can effectively measure the height, depth, and cross-sectional area of the upper and lower tear menisci (Wang et al, 2009).
Another study (Chen et al, in press) reported that among subjects who wear contact lenses, regardless of whether they were wearing their lenses at the time, the tear menisci area of the subjects who experienced dry eye symptoms was significantly less than that of the subjects who did not have dry eye symptoms, and the level of difference is correlated with the dry eye symptoms. The results of our research showed that the lower TMA was larger during wear of the SiHy lens than it was during wear of the traditional hydrogel lens at one week, two weeks and one month. The difference in the TMA of the two lens types might be correlated with the water content of the lens materials. The content of the balafilcon A silicone hydrogel lens is 36 percent, while the water content of the control lens is 59 percent. Because the higher water content may be associated with more dehydration, the normal tear meniscus might have been absorbed by the lens and reduced in volume.
The loss of soft lens water content can influence not only the tear volume in front of the lens, but also the thickness of tear film on the corneal surface (Nichols and King-Smith, 2004), so the larger tear meniscus area with the SiHy lens indicates that it can provide a wetter ocular surface environment. At present, anterior segment OCT technique is insufficient to measure the thickness of the tear film over the lens surface and over the corneal surface, but as a non-contact examination, its advantage is that it can directly observe the tear meniscus distribution during lens wear. If progressive development of the technique eventually allows the tear film thickness to be measured, then we will better know the tear condition under the lens.
The widely used tear volume measurement method in clinical practice is the Schirmer I test, which is also the routine examination index of dry eye. In this research, we used the Schirmer I test as the auxiliary means for measuring tear volume, and the results showed that there was no statistically significant difference between the two lens types. Because the Schirmer I test measures the basic tear secretion functions and because the effect of contact lens wear on tear secretion during short-term wearing is not significant, longer wearing times may be required to demonstrate the difference in the influence between the two lens types. According to the results of this research, the sensitivity and applicability of anterior segment OCT were better than those of the Schirmer I test when used to measure the tear volume of contact lens wearers.
Measurement of tear film properties is widely used for the clinical examination of dry eye. For contact lens wearers, alterations to the tears and tear film remain detectable even after the lens is removed due to the long-term exacerbation caused by tear evaporation. The stability of the tear film is measured using tear film breakup time during clinical examination. The goal of our research was to observe the influence of contact lens wear on the properties of the tear film.
The TBUT after wearing the hydrogel lens was shorter than that after wearing the SiHy lens at each timepoint, but the difference was not statistically significant. In theory, because the water content of the SiHy lens is lower, it may be associated with less changes to the aqueous tear film; but the wearing time of the two lens types in this study was too short to determine whether there is a significant difference in the degree of lens-induced tear film instability between the two lens types. Therefore, even if the influence still exists after lens removal, the sensitivity is not high. If we could directly measure the tear film stability during lens wear, the difference may be more significant. However, there are few objective reports about the long-term effects of SiHy lens wear on the normal tear exchange on the ocular surface and tear film functions (Santodomingo-Rubido et al, 2006).
The quality and amount of tear film on the ocular surface are directly connected to the health of corneal and conjunctival epithelia. Corneal epithelial staining is a common complication in contact lens wearers, and moderate-to-serious corneal epithelial staining could possibly lead to even more serious complications such as corneal inflammation or susceptibility to corneal infection (Szczotka-Flynn and Diaz, 2007; Santodomingo-Rubido et al, 2007). For this reason, we also observed whether there was corneal epithelial staining and its degree when wearing the two lens types in this study.
The final results showed that one case exhibited positive corneal fluorescein staining within one month after beginning wear of the SiHy lens (sporadically diffused punctate staining in the two nasal quadrants) while two cases exhibited corneal staining within one month after beginning wear of the hydrogel lens (sporadically diffused punctate staining in the two temporal quadrants in one case and sporadically diffused punctate staining in the nasal inferior quadrant in the other case). All corneal epithelial staining was dispersed and punctate, and returned to normal within one week after stopping contact lens wear.
Wearing the hydrogel lens was more prone to result in tear abnormity on the ocular surface, epithelial hypoxia, and corneal epithelial injury, but the difference was not statistically significant in this short-term daily wear study. However, the influence of the contact lens on the volume and properties of the tears as well as the oxygen permeability capability of the lens are closely related to the health of ocular surface epithelial tissues.
Compared with hydrogel lenses, SiHy lenses have demonstrated advantages in subjective symptoms of dry eye. Chalmers et al (2008) showed that when a traditional hydrogel lens was replaced with a SiHy lens, the proportion of wearers who experienced dry eye symptoms decreased by 50 percent. Schafer et al (2007) had similar results at only one week after switching to a SiHy lens, and these symptom improvements were stable during the three-year follow-up period.
The results of this research also suggest that SiHy lenses may be beneficial for dry eye symptoms. The subjective scores associated with dry eye symptoms with silicone hydrogel lens wear were almost half that of the scores with hydrogel lens wear. The only individual symptom with higher frequency after SiHy wear was foreign body sensation, which was probably due to the increased modulus of the study lens. However, the aspheric design of the front surface and the lower elastic modulus technique has made the lens more comfortable, and there was no statistically significant difference in the score of foreign body sensation between the two lens types.
The scores of the other three symptoms for SiHy wear were significantly better than those for hydrogel lens wear. This was especially true for the dryness and asthenopia symptoms when comparing the two lens types. The score of blurred vision associated with SiHy wear was lower, but the difference was not statistically significant. Therefore, the SiHy lens may provide better vision quality and comfort than the hydrogel lens can under the same conditions, and the SiHy lens is a good choice for patients not accustomed to long-term contact lens wear (Bergenske et al, 2007; Stern et al, 2004).
It should be mentioned that when comparing the subjective symptom scores with other objective examinations, there was no close relationship between the TBUT and the Schirmer I tests, which were also the main evaluation criteria for dry eye and subjective rating scores. Many subjects who had significant subjective symptom reactions had normal examination results. There was correlation between corneal staining and subjective symptoms in that the subjects who developed corneal staining had significantly higher subjective rating scores. These results indicate that the dry eye symptoms did not agree well with the objective signs in this contact lens-wearing sample. The wearers who had subjective symptoms but not signs could not be ignored in clinical practice, because the health and comfort of wearers is what we should pay most attention to.
Conclusion
To conclude, the tear menisci of the ocular surface when wearing this particular SiHy lens appears to be greater than that when wearing this particular hydrogel lens, and the subjective comfort when wearing this SiHy lens was better than that with the hydrogel lens. However, further studies are required to determine the effects of SiHy contact lens wear on other functions of the tears and tear film, tear exchange, tear film thickness and properties during long-term contact lens wear. CLS
The authors acknowledge Eye & ENT Hospital Affiliated to Fudan University for the funding support and test instrument. Professor Dai Jinhui is also acknowledged for the valuable suggestions and instructions on the design and implementation of this research. The authors thank Bausch & Lomb for the test materials.
For references, please visit www.clspectrum.com/references.asp and click on document #170.



