BLEPHARITIS UPDATE
Current Findings on Blepharitis
An overview of the signs, symptoms, etiology, and current and future treatments of this common disease.
By Daniel Powell, OD

| Dr. Powell is a post-doctoral fellow and is currently a PhD student in the Vision Science program at The Ohio State University following 12 years in clinical practice. His primary interests include ocular surface damage secondary to chemical exposures and dry eye diseases. He is currently supported by a grant from the National Eye Institute (EY015539). |
Blepharitis is a non-specific term to describe an array of inflammatory conditions involving the eyelid margin, and it is often overlooked or misdiagnosed (AOA, 2002). This may be attributed to its complex and multifactorial nature, the lack of an uncomplicated and formal definition, signs and symptoms that mimic eye conditions such as dry eye, and by outdated or misused terminology (Lemp and Nichols, 2009).
Blepharitis is a complicated, chronic condition that may be difficult to treat (Aronowicz, 2006) and can have an early onset with periods of remission and exacerbation (Friedlander, 2007; AAO Preferred Practice Guidelines, 2003). Even with an accurate diagnosis, the absence of a consensus on treatment may impact the progression, severity, and prognosis of the disease. Management of blepharitis can vary; however, treatment generally is comprised of both a pharmacological and a nonpharmacological component.
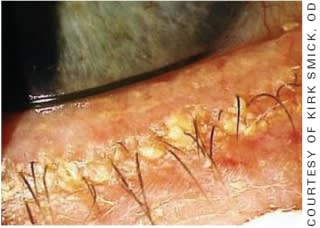
Figure 1. Anterior blepharitis demonstrating extensive crusting at the base of the eyelashes.
Epidemiology
Although blepharitis is recognized in the clinical and scientific community as one of the most common ocular disorders, minimal information exists on disease epidemiology within defined populations (AAO Practice Guidelines, 2003). To further complicate the matter, the literature over the past century illustrates the confusion and uncertainties regarding the definition of blepharitis as the various presentations of blepharitis have their own epidemiological characteristics (AOA Guidelines, 2002).
A few studies have reported on the prevalence of blepharitis with reports ranging from 12 to 47 percent (Lemp and Nichols, 2009; Hom, 1990). Most of the data available in estimating prevalence is likely inaccurate and based on a small sample size. This is further confounded by the lack of a formal blepharitis definition as well as its overlap with similar diseases such as dry eye, rosacea, psoriasis, atopy, and seborrheic dermatitis (AOA Guidelines, 2002). Also, many practitioners do not record every case of blepharitis, particularly if the condition is long-standing or the patient is asymptomatic.
Several demographic trends are evident in the occurrence of blepharitis, however. Anterior blepharitis appears to occur more often in young females who have a short history of symptoms, while meibomian gland dysfunction (MGD) more likely affects men older than 65 years, followed by women ages 46 to 65 years, and it presents with a longer history of symptoms (Bowman, 1987). Chronic blepharitis has been reported more often in fair-skinned women between the ages of 30 to 50 years (AOA Guidelines, 2002). In staphylococcal forms of the disease, scaling and crusting along the cilia, punctuated by acute exacerbations that lead to the development of ulcerative blepharitis, are common presentations that may become less severe over time.

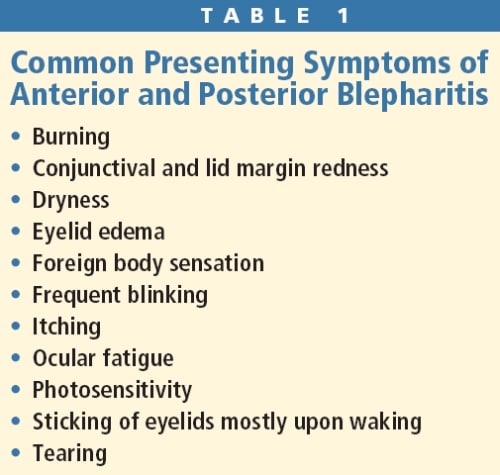
Figure 2. Posterior blepharitis demonstrating plugged meibomian gland orifices (left) and expression of thickened meibum.
A recent survey study queried 128 ophthalmologists and 84 optometrists on blepharitis frequency, the presence of coexisting conditions such as acne rosacea and dry eye, and their treatment strategies (Lemp and Nichols, 2009). Ophthalmologists and optometrists reported that the frequency of blepharitis in their patients was 37 percent and 47 percent, respectively. Both ophthalmologists and optometrists reported that men older than 65 years, followed by women between the ages of 46 to 65 years, were more likely to present with MGD compared to any other demographic. MGD was more likely to be present in patients who were light-skinned, had coexisting acne rosacea, and who demonstrated poor lid hygiene. Limiting factors with these studies include their small study sample numbers, which may not be representative of the entire patient population, and potential recall bias on the part of the respondents (the practitioners).
Disease Classification
Various attempts have been made to classify and subclassify blepharitis (McCulley, 1984; Driver, 1996; Foulks, 2003; Mathers, 2004; Smith, 2005). Some classifications have been based on clinical signs and symptoms, while others have been based on its inflammatory or infectious component (McCulley, 1981; Mathers, 1990). The complexity and the number of disease states that produce eyelid inflammation have no doubt made classification of blepharitis difficult (Smith, 1995). Perhaps the most clinically useful classification of blepharitis is a division into anterior and posterior subtypes. From a clinical standpoint, blepharitis and MGD have been used to describe the anterior and posterior forms of the disease, respectively. Mixed blepharitis is a hybrid that encompasses both anterior and posterior blepharitis. An alternate model classifies the disease based on its signs and symptoms: staphylococcal, seborrheic, a mixture of staphylococcal and seborrheic, and MGD (Jackson, 2008).
Anterior blepharitis affects the portion of the eyelid anterior to the mucocutaneous junction, or gray line (Figure 1). This anatomical line marks the point where the keratinized epithelium of the outer skin meets the non-keratinized epithelium of the tarsal conjunctiva. Anterior blepharitis can be further classified into acute and chronic forms. Posterior blepharitis, including MGD, affects the meibomian glands located posterior to the gray line (Figure 2). This form of the disease can be attributed to alteration of the lipids, called meibum, that are produced by the gland and are necessary for a functional tear film layer.
Clinical Presentation
Blepharitis often occurs in conjunction with other ocular surface conditions such as dry eye and conjunctivitis because of their contributions to the pathogenesis of the disease (Hara, 1996; Papier, 2007; Raskin, 1992). Table 1 lists typical presenting ocular symptoms that accompany both anterior and posterior blepharitis. Table 2 lists intrinsic and extrinsic factors that can exacerbate the progression of blepharitis.
Anterior Blepharitis The clinical presentation of anterior blepharitis includes collarettes, lash debris, lid margin redness, conjunctival redness, eyelid margin ulcerations, hordeolum formation, chalazion formation (rare), madarosis (whitened eyelashes), and trichiasis (misdirected eyelashes) (Lemp and Nichols, 2009). In both acute and chronic presentations of anterior blepharitis is the presence of multiple species of bacteria along with eyelid inflammation. Coagulase-negative Staphylococcus epidermidis is the most common bacterial species isolated from the lid margin of blepharitis patients, followed by Staphylococcus aureus, Proprionibacterium acnes, and Corynebacteria species (Dougherty, 1984; Groden, 1991; McCulley, 1986). As the condition becomes more chronic in nature, the skin of the outer eyelid is more likely to harbor non-pathogenic bacteria, and in greater amounts than in normals (Groden, 1991). Although the exact etiological mechanism is unknown, Smith and colleagues (1995) suggested three possible mechanisms underlying anterior blepharitis pathophysiology: direct bacterial infection of the eyelids, a localized hypersensitivity reaction secondary to the exotoxins released by the bacteria, and a localized delayed cell-mediated hypersensitivity response to the antigens that lie in the bacterial cell wall. The presence of these exotoxins in conjunction with the antigen-containing cell wall of Gram-positive bacteria may trigger an inflammatory response by releasing proinflammatory cytokines.
Besides bacterial colonization of the eyelids and their role in anterior blepharitis pathophysiology, infection by mites from the Demodex family (D. folliculorum and D. brevis) has been implicated in chronic blepharitis. Clinical presentations of these cases include keratitis and general ocular inflammation. Both their presence and waste products likely trigger an immune response similar to those in response to bacterial antigens and exotoxins. When viewed through a slit lamp under magnification, epilated eyelashes will reveal a mite within a cylindrical piece of dandruff.
Posterior Blepharitis The meibomian glands are a specialized type of gland called a holocrine gland. The cells within the gland normally manufacture a lipid product that is fluid. The cell membranes then break apart to release the lipid into the lumen of the gland where both the orbicularis oculi and Riolan’s muscle assist in expressing the lipid as meibum onto the posterior lid margin surface.
Alterations in the oily product of the meibomian glands may play a role in the onset of the signs and symptoms of posterior blepharitis (Shine, 1991; Dougherty, 1991). Normal secretions are clear while granular, turbid, or toothpaste-like expressions occur in MGD. There may be hyposecretion secondary to increased meibum viscosity or hypersecretion in seborrheic MGD. These lipid modifications can occur within the meibomian gland or following expression as a result of hormone abnormalities or toxic products produced and subsequently released by bacteria (McCulley and Shine, 2004; McCulley and Shine, 2003). Meibomian gland secretions contain mainly wax and sterol esters, which comprise the nonpolar component of the tear film’s outer lipid layer. Changes in these components can easily affect the melting point of the secretion, which will act to reduce meibum delivery and lead to meibomian gland occlusion (Figure 2 [left image]) (Driver, 1996).
In addition to posterior lid margin inflammation and thickening, hypersecretion or hyposecretion, and cloudy, granular, or toothpaste-like secretion (Figure 2 [right image]) upon expression, other clinical signs of posterior blepharitis include conjunctival hyperemia, chalazion formation, and concurrent facial rosacea (Lemp and Nichols, 2009). Chalazia frequently occur with MGD and are believed to arise from meibomian gland obstruction and resultant accumulation of lipid within the gland. Dougherty (1991) identified significant changes in these products by noting an increase in monounsaturated, longchain fatty acids. Smaller amounts of diand triesters, triglyceride, fatty acids, and free sterols also exist in these secretions. Alterations in meibum composition result in an increased melting point and viscosity of the meibum, which, in turn, negatively affects tear film stability. All of these factors play a crucial role in MGD development.
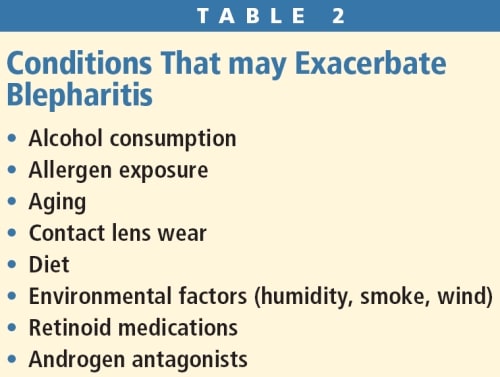
An obstructive form of MGD is associated with skin disease. It is characterized by abnormal or hyperkeratinization of the meibomian gland ducts and is a probable precursor to inflammation (Bron, 2004; Driver, 1996). Obstruction of the duct leads to reduced meibum in the tear film, resulting in dry eye from increased tear evaporation. Figure 3 shows images of the tear film lipid layer using a microscopy procedure. In addition, lipid production is reduced in the gland itself as a likely result of meibomian gland atrophy. Figure 4 shows the appearance through meibography of both partial and entire meibomian gland loss in patients who have MGD.
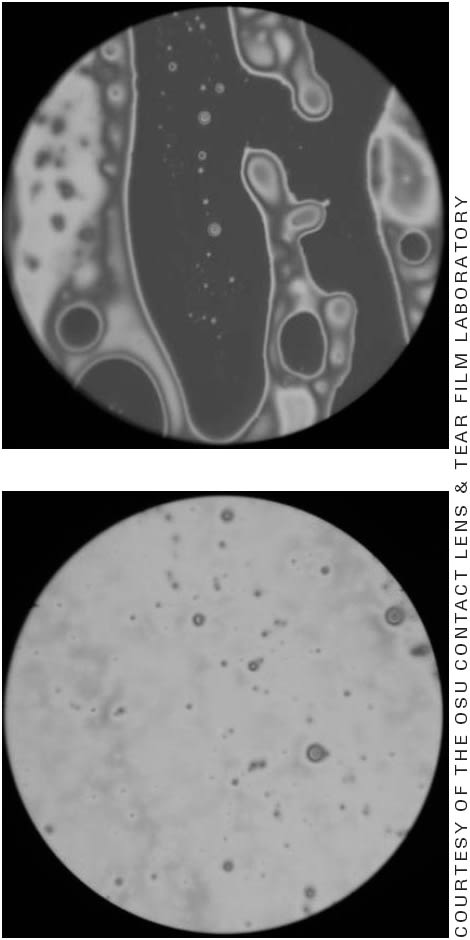
Figure 3. Tear film lipid layer microscopy. The top image represents a thinned lipid layer (as noted by the darkened areas) in a patient who has severe MGD. The average lipid thickness in this photo was 14nm. The bottom image represents the appearance of a normal lipid layer with an average thickness of 69nm.
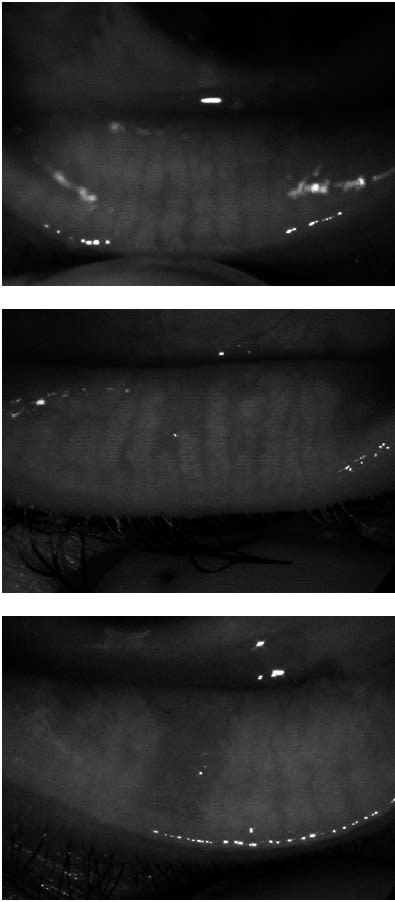
Figure 4. Meibography photos of (top) normal and (middle and bottom) abnormal meibomian gland appearance. Note the atrophy affecting the distal portion of the two center glands in the middle photo and the missing meibomian glands just to the left of center in the bottom photo.
As in anterior blepharitis, bacterial colonization can also have an effect in the development of posterior blepharitis by modifying the lipids secreted from the meibomian glands (Driver, 1996). S. epidermidis, S. aureus, and P. acnes have all been implicated in MGD by their production and release of bacterial lipases and esterases. Esterases produced by S. aureus hydrolyze cholesterol esters into proinflammatory cholesterol, which has been isolated in chronic blepharitis cases.
Unsaturated fatty acids, which are fluid at body temperature, are also a potential target of lipases and esterases. Lipases are exotoxins produced by coagulase-negative staphylococci, S. aureus, and P. acnes. These lipases are thought to break down triglycerides into monoand diglycerides, which have a higher melting point and thus will result in a lipid product that is more solid in nature. This can plug the meibomian gland and reduce the delivery of normal meibum onto the tear film, thus negatively affecting the integrity of the tear film (Foulks, 2003; Jackson, 2008; Driver, 1996). In addition, monoand diglycerides are pro-inflammatory and can trigger the production of cytokines, heightening the inflammatory reaction. Once the process is initiated, the interaction of abnormal meibum secretions, lipase production, and the inflammatory process aggravates the pathophysiology of the disease.
One of the target organs for androgens is the meibomian gland. Sufficient levels of androgens are necessary in the production and secretion of normal meibum. There may be an increased risk of MGD in cases of androgen insufficiency, which occurs with aging, menopause, androgen-blocking medications (spironolactone and prostate medications), Sjögren’s syndrome, and mutations within the androgen gene (androgen-insensitivity syndrome) (Sullivan, 2000; Sullivan, 2002).
Increased age is commonly associated with decreased meibum production, along with significant changes in meibomian gland orifice appearance. In addition, older individuals will have thickened meibum secretions. Histological examination of the meibomian glands in older individuals has revealed increased atrophy of the meibomian gland acini as well as thickening of the basement membrane where the acinar cells are produced.
Impact of Blepharitis on Contact Lens Wear
Up to 50 percent of contact lens wearers report some level of ocular dryness (Doughty, 1997; Nichols, 2002; Begley, 2001; Begley, 2000), and several mechanisms including increased ocular surface inflammation (Schultz, 2000; Pisella, 2001; Willcox, 1999), tear evaporation (Lemp, 1995; Mackie, 1985; Gilbard, 1986), and contact lens dewetting (Holly, 1975; Hatfield, 1993) have been implicated as the cause (Arita, 2009).
Several published studies have reported on the link between MGD and contact lens wear. Henriquez and Korb (1981) observed an increase in the number of obstructed meibomian glands in intolerant contact lens wearers as compared to all contact lens wearers. A recent paper by Arita (2009) concluded that not only was contact lens wear associated with a shortening of the meibomian glands distally at first followed by loss of the entire meibomian glands in the upper lid, but the degree of gland loss was also proportional to the number of years of contact lens wear regardless of contact lens prescription or contact lens material. In addition, there was a greater loss of meibomian gland numbers in all contact lens wearers compared to non-contact lens wearers. An explanation for the alteration and decrease of meibomian glands in the upper lid may be attributable to chronic trauma from the contact lens itself as the upper lid makes the largest movement during blinking (Ong, 1990).
Current and Future Blepharitis Treatments
The uncertain etiology of blepharitis, the significant overlap of symptoms between classifications, and its frequent coexistence with other ocular surface disorders has made blepharitis treatment difficult, impractical, and sometimes ineffective (AAO Preferred Practice Guidelines, 2003; AOA Guidelines, 2002; Perry, 2006). When evaluating treatment options, it is important to consider the goals of the treatment, which include improving quality of life by reducing symptoms; preventing disease progression; decreasing the potential for secondary disease states such as dry eye; and reducing the risk of adverse post-surgical outcomes. In addition to these goals, it is also important to consider issues such as onset of drug action, adverse events of the selected treatment, patient compliance, and interaction of the treatment with concomitant medications.
When weighing treatment options, it is important to consider both infectious as well as inflammatory control. A limitation with the various current blepharitis treatments is that they address either the infectious or the inflammatory component. It is, therefore, important to consider a dual treatment option that addresses both components. The pitfall with multiple treatments is that they can pose compliance issues.
Lid Hygiene Lid hygiene has been the traditional treatment for the removal of crusts from the base of the eyelashes. Warm, moistened compresses are positioned over the closed eyelids for a period of 10 minutes once to twice daily initially. This is followed by digital massage of the lid margins to increase the flow of meibum from the meibomian glands by increasing the melting point of the altered lipids. Even though this step can be eliminated in anterior blepharitis treatment, many patients will also have MGD involvement.
Patients can remove crusting using either a washcloth or cotton ball moistened in a mixture of water and baby shampoo or a commercial lid scrub product. Continuing lid scrubs following the initial treatment period is beneficial in preventing recurrences. Lid scrubs are useful in removing bacterial toxins. Drawbacks to lid hygiene include the slow improvement of symptoms, inadequate warmth of the compresses to melt the altered lipid, and the time commitment required given the chronic nature of the disease. In addition, lid scrubs are ineffective in reducing bacterial colonization of the eyelids, which requires adjunct pharmacotherapy (Smith, 1995; Jackson, 2008; Foster, 2005).
Artificial Tears Preservative-free artificial tears can help flush out bacterial toxins and inflammatory cytokines. A major drawback to this mode of treatment for blepharitis is its lack of antimicrobial and anti-inflammatory activity, which means it must be used concomitantly with another treatment. General dosing with these agents is four times daily.
Soothe XP (Bausch + Lomb) and the investigative formulation Systane Balance (Alcon) are two lipid emulsion-based artificial tears that may be beneficial in improving symptoms associated with evaporative dry eye by increasing tear lipid thickness and stability. These are also dosed four times a day.
Antibiotics Antibiotics help reduce bacterial colonization of the eyelid margin, which is important in accelerating the recovery rates from infection. Topical antibiotics are available as ointments or eye drop solutions. Bacitracin and erythromycin ointments are useful for treating Gram-positive organism such as Staphylococcus. Ointments are usually dosed one to four times daily over a two-week period and have an advantage over antibiotic solutions in their ability to remain on the eyelid for longer periods of time. However, they are quite messy to apply and have the potential to interfere with vision.
Fourth-generation fluoroquinolone eye drops are effective against a broad range of microbes. However, the increased presence of methicillin-resistant S. aureus (MRSA) and S. epidermidis (MRSE) organisms isolated from the eyelid margins poses a concern because they are becoming more resistant to these medications. Trimethroprim, a broad-spectrum topical antibiotic indicated for treating bacterial conjunctivitis in children, may show promise in treating MRSA and MRSE colonization in blepharitis patients (Epstein, 2010).
Downsides to antibiotic treatments include dosing issues, patient compliance, inconvenience, and adverse allergic reactions. Despite the antimicrobial properties of the pharmaceutical agents, they suffer from a lack of anti-inflammatory properties due to poor tissue and meibomian gland penetration.
Azasite (azithromycin 1%, Inspire Pharmaceuticals), a macrolide antibiotic in the same class as erythromycin and approved for the treatment of bacterial conjunctivitis, is undergoing clinical trials to examine its efficacy in treating blepharitis. This antibiotic also possesses anti-inflammatory properties by suppressing inflammatory cytokines such as IL-1α, TNF-β, and MMP-9 that are upregulated in ocular surface disease (Azasite package insert, 2007; Tamaoki, 2004). Following treatment in a clinical trial, subjects reported fewer symptoms including dryness, foreign body sensation, and burning (Nichols, 2009). Likewise, fewer clinical signs were noted post-treatment including reduced redness, reduced meibomian gland plugging by the return of meibum to its normal melting point, and an improved tear film breakup time (Foulks, 2009; Haque, 2010).
Oral doxycycline, a tetracycline-derivative, has been beneficial in treating MGD and acne rosacea for patients who do not benefit from lid hygiene alone. Tetracycline has also demonstrated anti-inflammatory properties by blocking bacterial lipase activity, which, in turn, decreases toxic fatty acid production (Raskin, 1992). A drawback with doxycycline is its slow onset of effect. Dosages range from 20mg to 100mg twice daily (or 250mg tetracycline four times daily) for up to nine months, although it is commonly prescribed for a three-month period. Low dosages, preferred for long-term therapy, are less likely to induce side effects including photosensitization of the skin and gastrointestinal upset. Isolated cases of orbital pseudotumor have been linked to tetracycline use.
Topical Corticosteroids Topical corticosteroids are reserved for severe inflammatory responses such as conjunctival injection, staph-sensitive subepithelial infiltrates in marginal keratitis, and phlyctenular keratoconjunctivitis. Use the lowest effective dose in these cases and taper the medication to avoid a rebound inflammatory effect. These medications do not address the infectious component, nor do they have an effect on altered meibomian gland secretions. As with all corticosteroids, prolonged use increases the risk of an intraocular pressure spike and cortical lens changes as well as secondary opportunistic infections secondary to immunosuppression.
Combination Medications Combination topical antibiotic and corticosteroid medications, available in both eye drop and ointment form, assist in patient compliance by combining both infectious and inflammatory control into one formulation. Tobradex (tobramycin 0.3%, dexamethasone 0.05%; Alcon) and Zylet (tobramycin 0.3% loteprednol 0.5%; Bausch + Lomb) are two such medications that have demonstrated roughly equal effectiveness; however, there has been some variability in Gram-positive sensitivity between the two medications. Risks associated with these medications include increased intraocular pressure, the potential for secondary latent viral infections, secondary bacterial infections, and ocular surface cytotoxicity from tobramycin. Tobradex ST (tobramycin 0.3%, dexamethasone 0.5%; Alcon), a new formulation of the original version, features a novel suspension technology containing pharmaceutical-grade xanthan gum that reduces viscosity and prevents settling within the container. This new formulation has demonstrated an increase in both bactericidal activity and tissue penetration and may prove beneficial in treating blepharitis in the near future (Scoper, 2008). In addition, this new suspension technology alleviates the need for shaking prior to instillation.
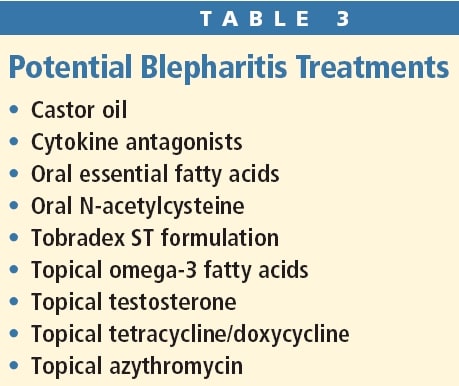
Table 3 summarizes other novel blepharitis treatments currently in the clinical trial stage.
Restasis Restasis (cyclosporine A 0.05%, Allergan), an immunosuppressant, is typically prescribed for treating dry eye and may be useful in treating cases of mixed dry eye and blepharitis. It is not recommended if an infective component is present as this may result in a secondary bacterial infection. Symptomatic relief may not be obtained despite a decrease in the number of meibomian gland inclusions (Perry, 2006; Jackson, 2008).
Oils Omega fatty acids, found in fish and flax seed oils, may improve the quality of the tear film by decreasing the levels of inflammatory cytokines. The treatment outcomes on some patients have been very successful; however, more research needs to be conducted to substantiate their usefulness in blepharitis and dry eye treatment. Tea tree oil at a 50% concentration applied to the eyelids has been shown to eradicate Demodex-related anterior blepharitis.
Conclusion
Several blepharitis treatment strategies are available. Unfortunately, multiple treatments are necessary as individual regimens only treat either the infectious or the inflammatory component of the disease. In addition, many of these treatments are slow in improving symptoms, messy, interfere with vision, require long-term use, and can lead to secondary complications such as increased intraocular pressure or bacterial or viral infections. New treatments, including topical azithromycin and a new formulation of Tobradex, may provide a major benefit as these medications address both the infectious and the inflammatory components. Future novel treatments, including topical testosterone and omega fatty acids, may prove very beneficial in the treatment of this ubiquitous eye condition. CLS
For references, please visit www.clspectrum.com/references.asp and click on document #176.



