ORTHO-K AND MYOPIA CONTROL
Orthokeratology for Controlling Myopia: Clinical Experiences
Two practitioners observe results similar to that in the literature for controlling myopia with ortho-k.
By Peter E. Wilcox, OD, & David P. Bartels, OD

A graduate of the University of Alabama at Birmingham School of Optometry, Dr. Wilcox completed a Primary Care residency at Pennsylvania College of Optometry. He is in private practice in Hayes, Va. He can be reached at doc@wilcoxeye.com. 
A graduate of Illinois College of Optometry, Dr. Bartels is in group practice in Buffalo, N.Y. He can be reached at visioncare@roadrunner.com. |
For more than 30 years, researchers worldwide have been studying myopia in children and experimenting with modalities to slow or stop its progression. Some of the tactics employed have been unpredictable and, at times, inconvenient.
For example, the use of atropine eye drops is one of the most successful forms of intervention, but the side effects greatly outweigh the outcomes (Gimbel, 1973; Lee et al, 2006). Spectacles with bifocal or progressive lenses have only minimal effect, and they are cumbersome for active children (Paluru et al, 2005; Leung and Brown, 1999). GP lenses worn during the day may slightly reduce myopia progression but at rates that are of limited value to patients (Walline et al, 2004; Katz et al, 2003). More recently, researchers have turned their attention to the potential of orthokeratology to control myopia in children.
Why Ortho-k Shows Promise
Patients undergoing overnight orthokeratology, also known as corneal molding and corneal reshaping, wear custom-made GP contact lenses that reshape the cornea and provide clear unaided vision during the day.
What makes ortho-k a promising treatment for childhood myopia? Researchers feel that hyperopic blur in the equatorial and peripheral retina may be a significant stimulus for increased axial length, which results in myopia progression (Hung et al, 1995; Smith et al, 2005).
Smith and colleagues reported exciting findings and provided intriguing images of axial lengthening (Figure 1) in their 2009 study of monkey eyes, designed to determine whether refractive development in primates is mediated by local retinal mechanisms. They reported:
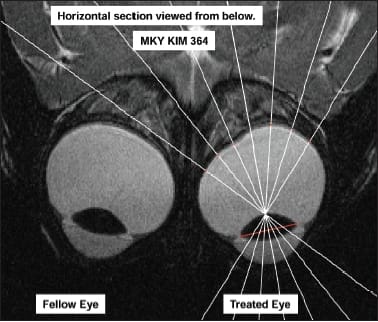
Figure 1. Hemiretinal form deprivation in infant monkey eyes resulted in myopia development in the treated areas. Photo courtesy of Dr. Earl Smith III. Reproduced with permission of Investigative Ophthalmology & Visual Science, Copyright 2009.
"The main findings of our study were that hemiretinal form deprivation altered refractive development in a regionally selective manner, typically producing myopia in the treated hemifields of infant monkeys, and that these treatment-induced changes in refractive error were associated with local, region-specific alterations in vitreous chamber depth in the treated hemiretina."
In our opinion, the clinical significance of this study is powerful, suggesting that eyes may become more myopic due to local deprivation of properly focused light. In the case of a myopic eye, conventional spectacles and contact lenses focus light at the fovea with hyperopic defocus in the midperipheral retina. This relative hyperopia may act as a local signal to stimulate axial elongation of the globe. The axial elongation results in a more myopic condition, which, when corrected, recreates the hyperopic midperiphery. The cycle ensues and the eye continues to become more myopic.
It could be theorized that a child who becomes myopic may have had a hyperopic peripheral refractive error that caused the eye to lengthen locally and become myopic. The rationale for the uncorrected myopic eye to progress is that the blur in the macula causes the local lengthening to occur in the macula. Studies are underway to explore these theories.
Interrupting this blur-lengthening cycle may be a key factor in the myopia stabilization effect attributed to orthokeratology.
Following ortho-k treatment for myopia, the typical molded cornea is flattened centrally and remains unchanged outside of the central 7mm or so. The annular zone, located between 5mm and 7mm, must, therefore, be relatively steeper to align with the unaffected cornea outside of the 7mm zone. This steeper zone results in more clearly focused light in the previously hyperopic midperiphery. Thus, the central zone of flattened cornea provides excellent Snellen acuity, and the red ring (Figure 2) may provide stability in the absolute refractive error.

Figure 2. Corneal topography images after ortho-k treatment for myopia. Note the red ring, which facilitates stability in absolute refractive error.
The panretinal stimulation of focused light from orthokeratology may slow myopic eye growth, whereas the spherical and/or aspherical focusing from spectacles and traditional daytime contact lenses is linked with progressing refractive errors from advancing axial lengths. These factors have been the impetus for recent studies of ortho-k for myopia control in children.
Promising Initial Study Results
The Longitudinal Orthokeratology Research in Children (LORIC) study (Cho et al, 2005), a twoyear pilot study conducted in Hong Kong, suggests that ortho-k can have a corrective and preventive/control effect in childhood myopia. The researchers cautioned, however, that predicting the effect for individual patients is impossible because of substantial variations in eye length changes among children.
In 2007, Walline reported myopia stabilization via ortho-k in the Corneal Reshaping and Yearly Observation of Nearsightedness (CRAYON) two-year results. In a subsequent study, Walline and colleagues (2009) confirmed previous reports of slowed eye growth following corneal reshaping lens wear.
Also in 2007, Eiden and Davis initiated the Stabilization of Myopia by Accelerated Reshaping Technique (SMART) trial, a five-year ortho-k/myopia control study of 300 children, ages 8 through 14. Interim results are being prepared for publication.
Clinical Findings
As we followed the literature and read about researchers' promising results, we began to take a closer look at our own practices, specifically at our young ortho-k patients. Interestingly, we found that our outcomes did more than mirror what the researchers were reporting. Ortho-k seemed to stop the progression of myopic refractive error in our young patients, although other controlled investigations have reported only a slowing (not stopping) of eye growth and unpredictable results for individuals.
We retrospectively evaluated five patient cases ages 9 to 15 who were myopic with or without astigmatism for periods ranging from 19 to 62 months. During this period, their myopic/astigmatic spherical equivalent had progressed by 0.46D per year. Their pretreatment spherical refractive errors ranged from −1.00D to −4.25D, and their cylindrical refractive errors ranged from plano to −1.00DC. Before ortho-k lens fitting, the mean spherical equivalent of the 10 eyes was −2.57D. During their 13 to 37 months of ortho-k wear, these patients either remained in their initial contact lenses or wore duplicate replacements for lost or broken lenses. All five patients achieved 20/20 vision during ortho-k treatment.
We wanted to find out whether there had been any progression in their baseline refractive error. Therefore, we asked them to cease lens wear until their topographies had returned to baseline or for a maximum of 14 days. Because corneal curvature may not return completely to baseline after long-term ortho-k in children (Wu et al, 2009), corneal unmolding was considered complete when patients' flat simulated K readings were within 0.50D of their pretreatment simulated K readings. A study by Hiraoka and colleagues (2009) confirmed that "the effect of orthokeratology is completely reversible in light of optical quality of the eye and quality of vision as well as refraction and visual acuity."
During the regression process, we performed noncycloplegic refractions at three- to seven-day intervals until reversal was complete or 14 days had elapsed. The results showed that the patients had essentially returned to their pretreatment refractive error, as the rate of progression of their spherical equivalent refractive error was only 0.03D per year (Figure 3). These are encouraging although anecdotal outcomes, and we are now designing a study to validate them.
Topography is Key to Ortho-k Success
Given the promising results of our pilot study, we will continue to recommend our ortho-k for myopia control program (see "Marketing the CANDY Plan") and to use the following ortho-k technique.


Figure 3. This graph of our case patients shows that in our practices, ortho-k treatment of myopia has successfully controlled the progression of myopia.
We fit our ortho-k patients in custom Wave (Wave Contact Lenses) ortho-k lenses. These lenses are software-designed based on topography data, with the Wave Design Software currently optimized for the Keratron family of topographers including the Scout Topographer (EyeQuip), which was used to generate the maps in Figure 1.
Before proceeding with contact lens fitting, we educate and inform all patients and parents about the associated pros/cons and risks/rewards of ortho-k treatment. Patients/parents sign the appropriate consent forms once they have read and comprehend the process and the variables. We also inform patients/parents that although the Wave lenses are similar in design and material to FDA-approved lenses, they are in fact used in an off-label manner (although the lenses we use are now approved for overnight wear under FDA guidelines for ortho-k).
Once we decide to pursue orthokeratology, capturing baseline topography is extremely important. Topography data are the foundation for the custom software-designed Wave ortho-k lenses, so patience and thoroughness are imperative for precise image capture. The lens material used for these patients was Boston XO (Bausch + Lomb). Other considerations when designing an accurate ortho-k contact lens include: refractive error, horizontal visible iris diameter, pupil size, pachymetry, tear quality, and interpalpebral fissure opening. We electronically submit the Wave corneal mold design data to the lab's CN lathe to manufacture each unique contact lens.
At the dispensing visit, we teach patients proper lens care and handling, including how to apply and remove the lenses. After this training, we apply the lenses and measure unaided visual acuities. Then we have patients recline with their eyes closed for 20 to 30 minutes. At the end of that time, we measure visual acuities and assess the fit with both white light and fluorescein (Figure 4). We then remove the lenses, measure unaided visual acuities and perform topography.

Figure 4. After having the patient recline with his eyes closed for 20 to 30 minutes, we assess the fit of the contact lenses with both white light and fluorescein.
Our patients and their parents have been satisfied with this experience. Any doubt or resistance disappears as the unaided visual acuities improve after lens removal, despite the brief period of closed-eye wear. We've had patients with unaided visual acuity of 20/200 read the 20/40 line after this brief wearing time.
We then ask patients to initiate nighttime wear. We've found that they routinely enjoy great unaided vision after their first night of wear. Repeating the nighttime wearing process provides them with daytime non-surgical freedom from glasses and contact lenses. We typically schedule follow-up visits at one week, one month, and six months, scheduling any additional visits as needed.
Conclusion
Many clinicians are familiar with the benefits of orthokeratology for adults. A significant added value of orthokeratology for young patients, which is supported by a growing number of initial studies, is the possible reduced rate of myopic progression. A recent study (Vitale et al, 2009) reported a 66 percent increase in myopia prevalence over a recent 30-year period. These facts address one of the oldest concerns that parents have held for their children: how to keep their eyes from getting worse every year. We may now have an answer. Learn it, promote it, and provide it. CLS
For references, please visit www.clspectrum.com/references.asp and click on document #174.



