THERAPEUTIC LENSES
Therapeutic Applications of Contact Lenses
A look at the current uses of therapeutic lenses and possible applications for the future.
By Gregory W. DeNaeyer, OD, FAAO

Dr. DeNaeyer is the clinical director for Arena Eye Surgeons in Columbus, Ohio. His primary interests include specialty contact lenses. He is also a consultant or advisor to MedLens Innovations, Inc. Contact him at gdenaeyer@arenaeyesurgeons.com. |
Contact lenses provide millions of people with glasses-free vision correction. However, since their inception, contact lenses have also served as a way to therapeutically manage anterior segment disorders (Hurwitz, 1974; Citon and Dyer, 1975). Most commonly, practitioners may use soft disposable lenses as temporary bandages for abrasions, but technological advances are quickly increasing the therapeutic scope of both GP and soft contact lenses. This article will explore the current therapeutic role of contact lenses in modern clinical practice, as well as future medically related applications.
Therapeutic Soft Contact Lenses
Indications for using soft contact lenses therapeutically include protecting a compromised ocular surface, pain management, and promoting epithelialization or wound closure (Coral-Ghanem, 2008; Rubinstein, 2003). At one time, pressure patching was a clinician's only available option for these indications, but soft contact lenses are now primarily used because they offer the following advantages: vision, continuous application of medication, and improved cosmesis. Therapeutic soft contact lenses are usually worn on an extended wear or continuous wear basis, and so silicone hydrogels are often the material of choice to minimize hypoxic-related complications (Dillehay and Miller, 2007; Dumbleton et al 2006) (Table 1). As well, there is evidence that re-epithelialization is faster with silicone hydrogel as compared to hydrogel lenses. One 2008 study by Gil-Cazorla et al that used soft contact lenses as bandages after laser epithelial keratomileusis (LASEK) showed that corneal epithelial status after five days was statistically better in the eyes that wore a silicone hydrogel lens (PureVision, Bausch + Lomb) as compared to the patients' other eyes wearing a non-silicone hydrogel (Equis 60; Mark'ennovy).

Numerous studies have been performed that demonstrate the effectiveness of silicone hydrogel lenses for managing a wide variety of anterior segment disorders (Ozkurt et al, 2005; Kanpolat and Uçakhan, 2003). A 2001 study by Lim et al used PureVision therapeutically for patients who had bullous keratopathy, chemical burns, corneal perforations, neurotrophic ulcers, corneal abrasions/erosions/lacerations, and post-surgical indications. Improved healing was noted in 96 percent of the eyes, with full healing occurring in 83 percent of eyes (Lim et al, 2001). Another study in 2006 by Bendoriene and Vogt showed that bandage contact lens wear with Night & Day (Ciba Vision) lenses was 93 percent effective for treating various anterior segment disorders in children.
The most common way that soft lenses are used therapeutically is as a bandage for an epithelial defect, which may be an abrasion secondary to trauma, surgery, corneal dystrophy, or persistent epithelial defect (PED) (Figure 1). A soft contact lens significantly reduces pain secondary to exposure and prevents the lid from disrupting epithelial migration during the healing phase. As discussed, silicone hydrogel lenses are in most cases the best choice because re-epithelization may occur faster as compared to with hydrogel lenses. Lens modulus does not appear to be a factor except in cases in which a soft contact lens may be worn chronically in patients who have corneal dystrophy (Grentzelos, 2009). In these cases, a silicone hydrogel lens material with a higher modulus may provide patients with better vision because it is able to mask some surface irregularity (Simard and Bitton, 2008).

Figure 1. Persistent epithelial defect (PED).
Patients wearing soft lenses as bandages for PEDs may heal more effectively with the addition of autologous serum eye drops. A 2006 study by Schrader et al showed that all six eyes of patients who had a PED and who were previously unsuccessful with conventional therapy, two of which had tried bandage soft lenses, healed with a soft lens bandage in combination with serum eye drops.
Anterior segment wound leaks can also be managed with bandage soft contact lenses. Wound leaks to the cornea can be secondary to trauma, surgery, or thinning and perforation. Wound leaks may also result from a thin bleb that perforates after trabeculectomy. A continuously worn bandage contact lens serves two functions with respect to wound leaks. First, a lens helps to decrease or stop aqueous from flowing through the wound that disrupts the healing process. Second, it protects migrating epithelial cells from the blinking lids. In some cases this is only a temporary fix and surgery is later required.
Finally, soft contact lenses may also be used therapeutically for protection from exposure in cases of bullous keratopathy and ocular graft versus host disease (GVHD). Bullous keratopathy results in blisterlike lesions of the epithelial surface that are secondary to severe corneal edema (Figure 2). These lesions can erupt and cause severe pain. Ocular GVHD can create a severe and disabling dry eye state and secondary keratitis. In both of these cases, the contact lens protects the compromised ocular surface from exposure and can alleviate patients' symptoms. Russo et al (2007) showed that patients who have refractory dry eye disease secondary to GVHD who wore Night & Day contact lenses on a seven-night continuous wear basis had significant improvement in subjective dry eye symptoms and visual acuity.

Figure 2. Bullous keratopathy.
Patients wearing soft lenses for therapeutic purposes will need frequent follow-up visits, especially because most of these patients will be wearing these lenses on an extended or continuous wear basis, to monitor for contact lens-related complications such as lens deposits, contact lens-related papillary conjunctivitis, and neovascularization. Most patients who have an epithelial defect and are wearing soft bandage contact lenses should be on concurrent antibiotic therapy to prevent secondary opportunistic infection. Educate them about the clinical signs and symptoms of a corneal inflammatory event or microbial keratitis and that they should immediately contact your office if these should occur.
Soft Lens Clinical Case Examples
Case #1 A 60-year-old female patient reported to the office emergently complaining of severe pain and photophobia of her right eye one day after undergoing a selective laser trabeculoplasty. She stated that her right eye began to hurt shortly after the procedure. The patient was not a contact lens wearer and had no other significant history. A slit lamp examination revealed a small central abrasion (Figure 3) of her right eye. All other findings were unremarkable.

Figure 3. Small central corneal abrasion.
We applied a spherical Acuvue Oasys (Vistakon) 8.4mm base curve plano power soft contact lens on her right eye to quell her symptoms and to promote healing. We prescribed tobramycin ophthalmic drops q.i.d. At her one-day follow-up visit she reported that her symptoms were completely resolved. After removing the bandage soft lens, a slit lamp examination revealed the surface to be completely epithelialized, but it still had a roughened appearance. She was instructed to continue the antibiotic drops for one week and to use Genteal (Novartis) ointment in her right eye every night for two months to prevent recurrent erosions.
Case #2 A 41-year-old male reported for consultation because he was suffering from severe dry eye symptoms secondary to ocular GVHD. He was using Tears Naturale (Alcon) every 15 minutes for modest relief. The patient was emmetropic and had no history of contact lens or glasses wear. Anterior slit lamp examination showed no corneal staining, and all other findings were unremarkable. We fit him in scleral lenses, but he eventually failed because of application issues secondary to having small apertures. We refit him into Acuvue Oasys (Vistakon) bandage soft lenses. Although he did have some difficulty with applying the soft lenses, he found them to provide significant relief and he was able to reduce his use of artificial tears to q.i.d. dosing while wearing these lenses on an extended wear basis.
Case #3 A 51-year-old male patient who had a corneal transplant after suffering a chemical injury developed an area of inferior temporal thinning and eventual perforation of his cornea (Figure 4). We initially fit him with an Acuvue Oasys (Vistakon) bandage soft lens and prescribed a fluoroquinolone antibiotic. He had to be refit one month later into a Westcon 20mm bandage lens because the Oasys lens eventually exhibited excessive fluting. He wore the Westcon lens for one month, but after little progress an attempt was made to glue the wound and the 20mm lens was reapplied. Finally, one month later without significant progress he had another corneal transplant.

Figure 4. Peripheral corneal thinning and secondary wound leak.
Drug-Eluting Soft Contact Lenses
The idea of a soft contact lens delivering ophthalmic medications has been around for 50 years (Wichterle, 1960). Currently, 90 percent of ocular drug delivery is applied via topical ophthalmic drops (Bourlais, 1998; Saettone, 2002). Unfortunately, ophthalmic medical management with eye drops can fail secondary to both noncompliance and a patient's inability to self-administer. Noncompliance by glaucoma patients has been estimated to be between 24 percent and 59 percent (Gurwitz, 1993; Rotchford and Murphy, 1998). Additionally, tearing and blinking after instillation results in a low bioavailability that has been estimated to be less than 5 percent (Kapoor and Chauhan, 2008).
Ideally, an ophthalmic device that could deliver a medication with zero order kinetics (constant release) could help to eliminate the therapeutic management challenges that noncompliance, unsuccessful drop administration, and bioavailability pose. Ocusert (Alsa Corp) once delivered pilocarpine to glaucoma patients; however, it is no longer commercially available (Ciolino et al, 2009). Collagen shields have been used for drug delivery, but because they are not optically clear, are cumbersome, and degrade quickly, they are not commonly used (Ciolino et al, 2009).
A drug-eluting soft contact lens would not only have the potential to effectively administer ophthalmic medications, but could also provide patients with vision correction. Drug-eluting contact lenses could be used to help manage a wide variety of ocular conditions such as dry eye, ocular allergy, inflammation, infection, and glaucoma. Considerations for this type of device include optics, safety, toxicity, and lens deposition of the drug.
Research has been conducted to see whether currently available contact lenses would be able to effectively uptake and release an ophthalmic medication. A study by Hui et al (2008) concluded that balafilcon A soft lenses that were saturated with ciprofloxacin-HCL released the drug too quickly to be effective. In 2009, Boone et al had similar results using silicone hydrogel and group I, II, and IV hydrogel lenses with the uptake and release of dexamethasone. However, Schultz et al (2009) concluded from data obtained from a limited number of study patients that hydrogel lenses could elute timolol and brimonidine to lower and maintain patient's intraocular pressure (IOP) as effectively as previous treatments could.
Current research is focusing on developing lenses that would be specifically manufactured and prescribed as drug-eluting contact lenses. Ciolino et al (2009) reported on a designed prototype contact lens that consists of a thin drug-PLGA (poly[lactic-co-glycolic acid]) film coated with pHEMA (poly[hydroxyethyl methacrylate]) that could be a platform for ocular drug delivery that follows zero order kinetics. In vitro results demonstrated sustained release for up to four weeks, and the release could be controlled by varying the PLGA-to-drug ratio. In another study, Ali and Byrne (2009) reported that they were able to use molecular imprinting strategies to create hydrogel lenses that release hyaluronic acid at a controlled rate. Currently, Vistakon Pharmaceuticals has a lens under investigation by the Food and Drug Administration (FDA) that would release ketotifen-4 to treat allergic conjunctivitis.
MEMS Technology
Micro-machined electro-mechanical systems (MEMS) have the potential to revolutionize the way that we use contact lenses. Sensimed Triggerfish, currently under investigation, is a silicone disposable contact lens embedding a MEMS sensor and a telemetry microprocessor that continuously monitors and records a patient's IOP for up to a 24-hour time period. The contact lens is available in three base curve radii, and all of the MEMS elements are eccentric (Figure 5). With the contact lens in place, a strain gauge detects changes in corneal curvature that are related to IOP changes. Information is picked up by a receiver that is worn proximal to the eye, and a data cable transfers the information to a recorder. This recorded cycle of IOP measurement includes overnight readings, which allows for a more complete assessment of diurnal IOP variation. According to Sensimed, up to 50 percent of IOP peaks occur outside of office hours.
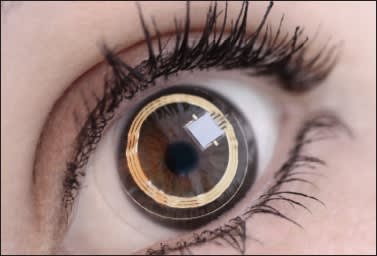
Figure 5. Sensimed Triggerfish.
A study by Leonardi et al (2009) showed that the wireless contact lens sensor had good correlation with cannulated enucleated pig eyes. For humans, possible factors that could affect precision and calibration in vivo include diurnal changes in corneal thickness secondary to stromal hydration, biomechanics, keratometry, corneal diameter, scleral thickness, and rigidity (Leonardi et al, 2009).
Twa et al (2009) explored the use of a piezoresistive pressure sensor mounted on a GP contact lens. A wire extended from the anterior surface of the lens was attached to a standard dynamic contour tonometer. Although their results were favorable, the downside of this set-up is that it is limited in use because it is not wireless.
Therapeutic GP Contact Lenses
Scleral contact lenses are not used exclusively for masking corneal irregularity; they are also used therapeutically to manage severe ocular surface disease (OSD) by protecting the fragile anterior surface. Scleral lenses semi-seal to the eye, which allows them to hold a fluid reservoir that can continually bathe the anterior ocular surface like a liquid bandage. Scleral lenses are thus able to provide pain relief, prevent exposure keratitis, and enhance epithelial wound healing.
The amount of reservoir that a scleral lens can hold increases with increasing diameter; therefore, scleral lenses that are generally 18mm in diameter or larger are needed, as they support sufficient fluid to be therapeutic. A study by Romero-Rangel et al (2000) described the therapeutic benefits of scleral contact lenses. Patients included had OSD secondary to Stevens-Johnson syndrome, ocular cicatricial pemphigoid, exposure keratitis, toxic epidermal necrolysis, post-herpetic keratitis, congenital deficiency of meibomian glands, superior limbal conjunctivitis, Sjögren's syndrome, and inflammatory corneal degeneration. Improvement in quality of life as a result of a reduction in photophobia and discomfort was reported by 92 percent of the patients studied.
Patients who have OSD usually take a host of ocular therapeutic medications. Dosing of these medications must occur before application or after removal of the lenses as bioavailability will be significantly reduced secondary to slow reservoir turnover. Patients who have severe OSD have a fragile epithelial surface, and it is imperative that you prescribe lens care products that will have the least risk for toxicity. Hydrogen peroxide systems work well for lens care, and non-preserved artificial tears are a good choice for application and lubrication. Patients may have to remove their lenses during the day to rinse and rewet them if debris builds up underneath the lens. Visser et al found in a 2007 study that patients who had keratoconjunctivitis sicca required these breaks around 66 percent of the time.
After successful fitting, these patients should be followed, at minimum, every six months to monitor the lens fit and anterior surface integrity.
Scleral Lens Clinical Case Examples
Case #4 A 64-year-old man reported for evaluation complaining of severe disabling dryness secondary to ocular GVHD. He had been unsuccessful using Restasis (Allergan) and non-preserved Refresh (Allergan) drops. His symptoms were so severe that they prevented him from working as an engineer. Slit lamp examination showed his anterior corneal surface to have moderate coarse superficial punctate keratitis (SPK) in both eyes. After discussing the options, he was fit into scleral GP lenses, 18.8mm in diameter. After dispensing the final lenses he was able to see 20/25 in both eyes and was symptom free while wearing the lenses. The patient was able to return to a normal work routine.
Case #5 A 62-year-old female patient reported complaining of severe dry eye syndrome that was preventing her from performing daily activities. She was on Restasis (Allergan), and Genteal (Novartis) drops every one to two hours during the day, and Genteal ointment (Novartis) at night. The patient also reported at times having to wear swim goggles for relief. She was eventually fit into scleral GP lenses 18.8mm in diameter. The patient experienced immediate relief with the lenses in place and was able to resume all of her activities.
Conclusion
Although the primary application of both soft and GP lenses continues to be providing our patients with vision correction, their scope of utilization is increasing. Both soft and GP modalities are now commonly used as bandages or protective shields for patients who suffer from acute traumatic abrasion or OSD. Technological advances will allow contact lenses to become both vehicles for ocular therapeutic medications and state-of-the-art diagnostic instruments. Ultimately this will enhance our practices and patient care. CLS
For references, please visit www.clspectrum.com/references.asp and click on document #174.



