IRREGULAR CORNEA
Corrective Options for Irregular Corneas
This article discusses contact lens and surgical options for several irregular cornea conditions.
By Jeffrey Sonsino, OD, FAAO, & Mark D. Ewald, MD
Today's modern cornea and contact lens practices rely on input from both surgical and contact lens consultations. Using all of the tools available is the best way to help our patients who have complicated and irregular corneas. To accomplish this task, there must be a tight coordination of care between cornea specialists and contact lens specialists. Both specialists rely on each other to maximize outcomes.
For example, fitting a Salzmann's Nodular Degeneration patient with GP lenses may become much easier after phototherapeutic keratectomy (PTK) smoothes the corneal surface. Likewise, a cornea specialist's careful work with a penetrating keratoplasty (PK or PKP) will be apparent to the patient only after a GP lens maximizes the vision. This article discusses the most relevant ideas in surgical and contact lens management of some of the most common irregular cornea conditions in a specialty practice.
Keratoconus
Keratoconus is a condition that is very familiar to contact lens specialists. It accounts for the majority of patients in most specialty contact lens clinics. There are many emerging technologies for managing keratoconus.
Contact Lens Correction The Collaborative Longitudinal Evaluation of Keratoconus (CLEK) study led to significant changes in our fundamental understandings of keratoconus. It also taught us that measuring corneal curvature was possible by finding the first definite apical clearance lens and then flattening to achieve a three point touch or mild bearing on the apex of the cone (Edrington et al, 1996). Many practitioners use this process today as a strategy for fitting corneal GP lenses in keratoconus.
Aspheric posterior surface lenses have more recently emerged as great lens options for patients who have keratoconus (Kok and Cheng, 1991). Details about aspheric lenses are often proprietary by each company, but recent examples of such lenses include AKS (Art Optical, Figure 1), Dyna Z Cone (Lens Dynamics), Rose K2 (Rose K Ltd./Menicon), and S-Cone (Essilor).

Figure 1. Sodium fluorescein pattern of an Art Optical AKS lens on an extremely steep keratoconic cornea (base curve of 69.50D/4.86mm). There is a three point touch pattern with a dense midperipheral pattern. The lens did not dislodge and provided 20/25 vision.
It is critically important to consider all contact lens options for these patients including corneal GP lens fits as discussed above and scleral lens options. Modern scleral lenses no longer have the physiological limitations of their lower-Dk predecessors from many years ago because they are now available in many different materials of much higher oxygen permeabilities.
Surgical Correction Even with all of these fantastic contact lens options, a smaller number of keratoconus patients will need surgical correction. Surgical options should be explored only when all non-surgical options are exhausted. Surgery might be considered when patients are no longer able to tolerate their GP contact lenses, when a successful contact lens fit is no longer possible, when vision is poor despite a well fitting contact lens (due to a central corneal scar, for example), or because of unresolving corneal hydrops.
There are several surgical options for correcting irregular astigmatism due to keratoconus depending on the patient's presentation, previous ocular history and surgeon preference. Available options include PK, deep anterior lamellar keratoplasty (DALK), intrastromal corneal ring segments (ICRSs), and corneal collagen crosslinking (CCR).
Penetrating Keratoplasty A PK, or full-thickness corneal transplant, historically has been the most common surgical correction for irregular astigmatism resulting from keratoconus. Given the excellent eye-banking system in place in the United States, the availability of high-grade corneas suitable for transplantation makes this procedure readily available in all urban and suburban areas.
A PK has several advantages that have made it the surgery of choice for many corneal specialists. After almost a century of practice with good results, PK is dependable, reliable, and well studied. Performing a PK is not as technically difficult as other surgical options and it can be performed using a retrobulbar block if the patient is unable to be placed under general anesthesia.
There are challenges with PK as well, which is why corneal surgeons have sought other surgical options for correcting irregular astigmatism. While performing a PK the eye is "open-sky," meaning that it is open to the outside world. This increases the risk of infection and expulsive choroidal hemorrhages—both potentially sight-threatening complications—during surgery. The PK-graft is secured to the host cornea using free-hand sutures, leading to postoperative astigmatism in the newly transplanted corneal graft. Frequently, the post-surgical astigmatism is significant enough to require a GP contact lens for best-corrected vision (Figure 2). In fact, one study on 23 post-PK eyes showed a mean spherical equivalent of –7.58D ± 4.42D and a mean cylinder of 3.64D ± 1.72D (Donnenfeld et al, 1999).

Figure 2. Post-PK contact lens fit with a Lens Dynamics Dyna Intra-Limbal design. The large diameter of this lens allows for complete pupil coverage and does not contact the graft-host junction.
The surgical sutures themselves can cause problems for patients if they break postoperatively and cause pain or become the nidus for infection. The corneal graft is susceptible to epithelial, stromal, and endothelial forms of inflammatory rejection from the host's immune response. The full-thickness nature of a PK places the cornea at a lifetime risk for traumatic wound dehiscence which, at minimum, requires surgery to repair and, if the trauma is severe enough, may lead to traumatic expulsive choroidal hemorrhage and vision loss.
There are other disadvantages in treating keratoconus with PK. The "cone" of ectasia is often located inferiorly, meaning the PK either must be displaced inferiorly or be large and centrally located to successfully correct the irregular cornea. Also, the host cornea to which the PK is secured will still exhibit progressive keratoconic thinning, which leads to wound irregularity and progressive astigmatism, especially inferiorly.
Deep Anterior Lamellar Keratectomy Many of the disadvantages with PK have led to alternative surgical procedures. Most recently, corneal surgeons have developed DALK. Although the exact procedure may vary somewhat from surgeon to surgeon, the basis of the surgery is to remove all host corneal tissue anterior to Descemet's membrane and place a donor corneal graft stripped of Descemet's membrane and endothelial cells into the surgically created defect. The purpose of DALK is to preserve host Descemet's membrane and endothelium. Because the ectasia in keratoconus is a stromal ectasia, not an endothelial dystrophy, the host endothelium does not have to be removed to correct irregular astigmatism from keratoconus. Leaving host Descemet's membrane intact during surgery reduces the complications of an "open-sky" technique. DALK also eliminates endothelial rejection, since the endothelium is still host tissue. This may decrease overall graft rejection episodes, including stromal and epithelial rejection, although research investigating this topic is ongoing.
A DALK procedure has its own disadvantages as well. DALK is technically more difficult compared to PK. Free-hand sutures are placed, making postsurgical irregular astigmatism possible, and there is still a lifetime risk of traumatic corneal wound dehiscence and expulsive choroidal hemorrhages due to the circular corneal wound.
Intrastromal Corneal Ring Segments Another recent intervention for correcting irregular astigmatism is the placement of ICRSs, commercially available as Intacs (Addition Technology). ICRSs can be placed manually or with channels created with the assistance of a femtosecond laser. In keratoconus, ICRSs are used to "flatten" the "cone" of the ectatic cornea, improving vision. ICRSs also can improve corneal astigmatism and allow a contact lens specialist to refit the cornea with a contact lens, improving vision.
ICRS disadvantages include extrusion of the ring segments anteriorly through the cornea, infection, technical difficulty in placement, and a difficult contact lens fit—if needed—post-insertion.
Collagen Crosslinking Although not yet approved by the U.S. Food and Drug Administration (FDA), corneal CCR is an exciting technique for improving irregular corneal astigmatism, including astigmatism associated with keratoconus. Riboflavin and ultravioultraviolet light are applied to an ectatic cornea to increase the crosslinking between stromal collagen fibers. The increased collagen bonds act to stabilize a cornea from becoming more ectatic and may even lead to improvement in the irregular astigmatism.
Promising results from CCR trials in Europe and Asia have led to current ongoing FDA trials. Some studies have shown that refractive surgery, such as photorefractive keratoplasty (PRK) or laser-assisted in situ keratomileusis (LASIK), can be performed on ectatic corneas following CCR because the stromal collagen is reinforced and at decreased risk of post-refractive ectasia. Once it is FDA-approved, many keratoconus patients in the United States may be able to postpone or avoid PK through CCR.
Post-Trauma
Open globe injuries with corneal lacerations may result in retinal damage when the trauma is severe. Oftentimes, these injuries are unilateral. In a case series of 19 patients fit with contact lenses after posterior segment trauma, 12 patients discontinued their lenses an average of one year post-discharge from the contact lens service (Kehler et al, 2009). This indicates that despite our best efforts at using the best technology lenses, other options need to be discussed.
Post-traumatic irregular astigmatism usually results from irregular healing of the cornea or from sutures placed following emergent surgical repair. If a traumatic corneal wound is within the visual axis, causing decreased vision, and is due to a perforating (full-thickness) wound, PK is often needed to excise the corneal scar and remove the irregular astigmatism associated with the scar.
Decreased vision associated with astigmatism from a penetrating (non-full-thickness) traumatic wound can be repaired using PK, DALK (assuming Descemet's membrane and the endothelium are intact), or possible PTK.
Phototherapeutic Keratoplasty PTK uses the excimer laser to remove anterior stromal scars and irregularities. When PTK is used to both remove opacities and to correct for refractive error, it is referred to as PRK or PTK/PRK. PTK and PRK have possible pitfalls, including corneal ectasia similar to post-LASIK ectasia, corneal haze, and dry eye.
Corneal Neovascularization
Induced corneal neovascularization (NV) can result from many inciting events, including alkaline and acidic chemical ocular injuries, hypoxia from contact-lens abuse, and infections such as herpes simplex, trauma, rheumatologic conditions, and chronic iritis. The first line of therapy is often GP lens correction for maximizing visual potential (Figure 3).

Figure 3. Scleral contact lens fit on a patient who has severe corneal neovascularization due to neurotrophic keratopathy. The fellow eye is occluded with a full tarsorrhaphy. Best-corrected vision prior to scleral lens fit was 20/100. With a scleral lens, she achieves 20/30 vision.
Surgically removing and preventing recurrence of NV can be challenging, as the underlying etiology must be controlled for the surgical intervention to be successful. Most commonly, PKs are performed to excise the affected cornea. But since the neovascularization vessels abut the corneal graft, the donor cornea is at a much higher risk of rejection. DALK can be considered as well, if the host endothelium is unaffected, but there is still an increased risk of rejection due to abnormal host corneal blood vessels.
If NV is due to a corneal limbal stem cell (LSC) deficiency, such as occurs following acidic or alkaline ocular chemical injuries, a surgeon may perform an LSC graft. LSCs can be procured from a patient's fellow eye if the fellow eye has an adequate supply. LSCs can also be transplanted from a cadaveric donor, although the postoperative course after cadaveric-LSC grafting includes systemic anti-inflammatory and immunosuppression medications to reduce rejection.
If the above procedures have failed, a corneal prosthesis can be considered. Although there are several different types, all keratoprostheses involve the placement of a clear, synthetic, artificial cornea either directly into the host cornea or within a donor vehicle cornea that is sutured to the host cornea to restore vision. Keratoprostheses are often used in extreme circumstances, such as monocular patients who have failed multiple previous visual rehabilitation procedures. The placement of a keratoprosthesis can be complicated by postoperative endophthalmitis, retroprosthetic membrane formation, and glaucoma. Patients who have a keratoprosthesis typically experience disabling glare following the procedure due to the translucent periphery. A recently published study indicated that vision and glare reduction could be improved with prosthetic pupil-control contact lenses (Sayegh et al, 2010) (Figure 4).
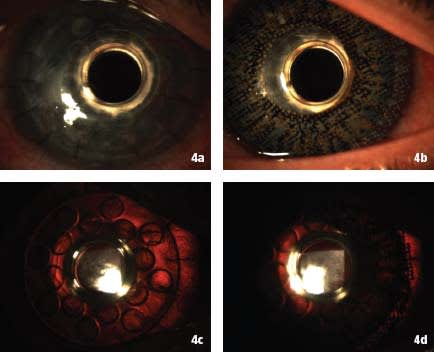
Figure 4a. Color anterior segment photograph of Boston KPro keratoprosthesis. 4b. Color anterior segment photograph of pupil-control prosthetic contact lens (Ciba Vision D3 ColorBlends blue with 6mm black underprint). 4c. Retroillumination of naked Boston KPro. 4d. Retroillumination of Boston KPro with pupil control contact lens.
Salzmann's Nodular Degeneration
Salzmann's Nodular Degeneration is often one of the most challenging contact lens fits. Elevations on the cornea create irregular astigmatism but are poorly suited to corneal GP correction. Corneal GPs tend to abrade the elevations and result in poor comfort and infection risk due to corneal epithelium barrier function loss. In cases of relatively little irregular astigmatism, soft toric silicone hydrogel lenses often function well. In more advanced cases, piggyback strategies provide both optical correction from the GP and corneal protection from the silicone hydrogel lens (Figure 5). Scleral lenses are now commonly used to vault the corneal surface; they must have adequate chamber diameter to accommodate the peripheral nodules and are usually non-standard in design.
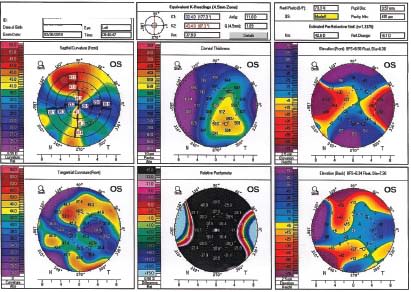
Figure 5. Topography of a patient who has severe Salzmann's Nodular Degeneration. This highly irregular toric shape was most amenable to a bitoric GP piggyback fit. Vision was 20/25, but end-of-day comfort was a chronic problem for this patient.
The initial surgical treatment for Salzmann's Nodular Degeneration is PTK or PTK/PRK because it is an anterior degeneration of the cornea. PTK is quite effective in removing the irregular cornea and, when combined with PRK, can improve vision. The downside to PTK and PTK/PRK is that nodules often recur if the underlying etiology that led to their formation is not addressed and corrected.
If multiple PTK/PRK procedures have been performed, precluding further thinning of the cornea, or if corneal scarring is more extensive than can be corrected with PTK/PRK, consider a PK or DALK procedure to remove the nodules and improve corneal astigmatism.
Post-LASIK Ectasia
Correcting post-LASIK ectasia optically with GP contact lenses is often successful. Aspheric posterior surface lenses and keratoconic lenses are the most common designs. Lens centration and comfort can be difficult to achieve. Further, patients who were seeking correction-free vision through LASIK in the first place are often very challenging to accommodate with contact lenses.
Ectasia due to refractive procedures often results from corneal thinning. For this reason, further PTK, PRK, and LASIK for visual rehabilitation are often avoided. Surgeons consider an ICRS if enough residual stroma is present to allow placement. If ICRSs are not possible, PK or DALK is used to surgically correct the post-refractive surgery ectasia. Once FDA approval is obtained, CCR may be used to prevent progression and may possibly reverse the ectasia. CLS
To obtain references for this article, please visit http://www.clspectrum.com/references.asp and click on document #180.

Dr. Sonsino is an assistant professor at Vanderbilt Eye Institute where he is the chief of the optometry section. He is a fellow of the American Academy of Optometry and is currently a candidate for Diplomate in Contact Lenses. He is also the chair of the American Optometric Association's Anterior Segment Committee and co-editor of the Contact Lens Section Newsletter. |

Dr. Ewald is an assistant professor in Ophthalmology specializing in corneal and external diseases at the Vanderbilt Eye Institute in Nashville, Tenn. His interests include corneal ectasias, corneal infections, and cataract extractions. |



