Online Photo Diagnosis
By William Townsend, OD, FAAO
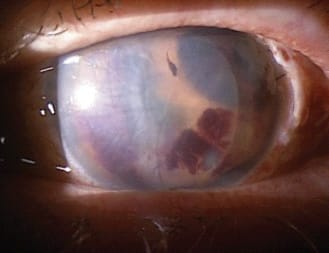
The individual in this photo suffered an intra-operative hemorrhage while undergoing Descemet's stripping with automated endothelial keratoplasty (DSAEK). In reviewing the literature, we found no reports of this specific complication. The second image shows a different patient who had a successful DSAEK procedure. DSAEK was introduced by Melles et al in the late 1990s and has been a useful and often successful alternative to penetrating keratoplasty (PK). It is particularly helpful in conditions that impair endothelial function such as Fuch's dystrophy. Advantages over PK include lower rejection rates, shorter recovery time, and reduced levels of induced astigmatism. Patients often report visual improvement within days or weeks.
As the name implies, the surgeon makes a small incision and strips a circle of the recipient's central endothelium away from Descemet's membrane. The surgeon then inserts donor endothelium attached to a thin layer of Descemet's membrane and stroma into the anterior chamber and positions it over the recipient's posterior cornea. The donor tissue is held in place with an air bubble tamponade that is gradually replaced with aqueous. In most cases the donor tissue quickly adheres to the posterior cornea and begins pumping fluid out of the cornea.
While this procedure is usually successful, complications may arise. Suh et al reported that 27 (23 percent) of 118 eyes that underwent DSAEK developed graft detachments. Twenty-five of the eyes that developed detached grafts were successfully repositioned and/or re-bubbled after surgery. Seven (6 percent) of the 118 eyes developed graft rejection, and one eye suffered from epithelial in-growth while another developed blood at the graft interface.

Our patient presented seeking a second opinion on treatment options for her anterior segment hemorrhage. The central area of the cornea had no endothelium and therefore did not stain with blood, but was very edematous with numerous stromal folds. There was blood staining of the endothelium that had not been removed during the procedure, and we also noted blood in the anterior chamber. In this situation, a PK is preferred over a second DSAEK procedure. We referred the patient to a corneal specialist with whom we had co-managed several DSAEK cases. The patient had the PK done just as few days ago, and at press time, we have not received word of the final outcome of the PK.



