Contact Lens Case Reports
A Scleral Lens Post-HSK


By Patrick J. Caroline, FAAO, & Mark P. André, FAAO
Our patient is a 48-year-old female with a longstanding history of herpes simplex keratitis (HSK) involving her right eye only. Over the years she has experienced significant symptoms of dryness and irritation despite maximum topical and systemic dry eye therapies. The patient was referred to us for possible contact lens management to address both her ocular discomfort and her vision.
A Scleral Solution
On initial presentation the patient had a faint anterior stromal haze centrally with 2+ punctate epithelial erosion centrally and peripherally OD (Figure 1). Her left eye was within normal limits. Her best-corrected visual acuity with spectacles was OD 20/60 with a prescription of +3.75 –2.00 x 85 and OS 20/20 with a prescription of +0.75 –0.50 x 065. The increased hyperopia OD is a common finding following a herpes simplex virus (HSV) infection and is the result of corneal flattening secondary to the loss of stromal tissue associated with the virus (Figure 2). Central corneal thickness was 0.42 in the right eye and 0.52 in the left.
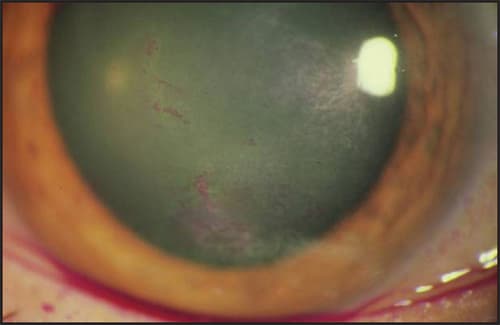
Figure 1. The patient's right eye post-HSV.

Figure 2. Corneal mapping demonstrating the topographical flattening secondary to the HSV infection.
The patient's irregular astigmatism could have been managed easily with a traditional rigid corneal contact lens design. However, the presence of the chronic corneal dryness suggested that the patient might be a better candidate for a scleral GP design. She was subsequently fitted with a scleral lens OD: base curve 7.80mm; power –6.50D; diameter 16.5mm with a corrected VA of 20/25 (Figure 3).
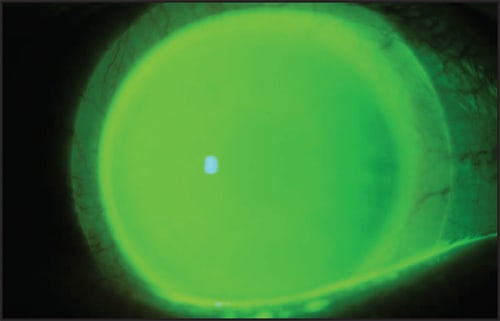
Figure 3. The scleral lens on the patient's right eye.
In fitting modern scleral lenses there are three fitting objectives:
1. The lens should clear the entire cornea.
2. The lens should clear the limbus 360 degrees around (or as much as possible).
3. The lens should “land” on the sclera with the full weight, pressure, and bearing of the lens coming to rest on the sclera (Figure 4).
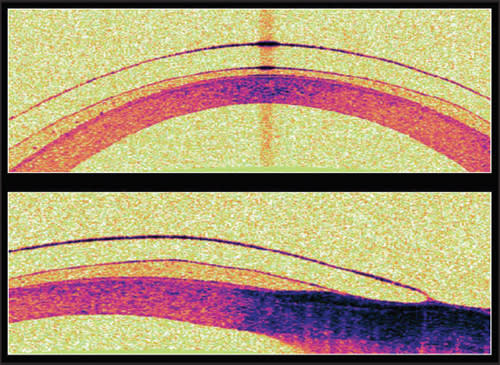
Figure 4. Anterior segment OCT demonstrates the central corneal and limbal clearance with landing of the lens on the sclera.
At dispensing the patient reported good comfort with the scleral lens, but she did report some symptoms of diplopia. We advised her that “double vision” is common for individuals who have been monocular for long periods and that her symptoms should decrease over the next week. On follow up the patient was wearing the scleral lens 14 to 16 hours a day with excellent comfort. Her diplopia had indeed resolved, and she was now enjoying the many benefits of binocular vision. CLS
Patrick Caroline is an associate professor of optometry at Pacific University. He is also a consultant to Paragon Vision Sciences. Mark André is an associate professor of optometry at Pacific University. He is also a consultant for CooperVision.



