IRREGULAR CORNEAS
Contact Lens Options for Irregular Corneas
The latest technologies can restore visual function to irregular cornea patients who can't tolerate GP lenses.
By Marsha M. Malooley, OD, FAAO, & Charles A. Faron, OD
As contact lens fitters, we are fortunate to be able to impact patients' lives by giving them spectacle independence and offering them, in some instances, their only means of optimal visual correction. We are also fortunate to have a variety of contact lens options at our disposal. Most patients will have normal corneas, but we will all encounter a subgroup of patients who have irregular corneas. These patients may have naturally occurring diseases such as keratoconus or pellucid marginal degeneration (PMD). Others may suffer from iatrogenic ectasias, have corneal transplants, or have traumainduced corneal scarring.
Patients who have irregular corneas are traditionally managed with corneal GP contact lenses. While GPs are very useful in providing patients with good vision, they are not always successful. Today's technologies provide a variety of alternatives to manage our patients. Older contact lens designs have been improved, redesigned, and reintroduced. Diagnostic equipment, lens materials, and manufacturing techniques have evolved. The number of specialty contact lens options is expanding exponentially, and as primary eyecare providers we have an obligation to be aware of those options appropriate for our patients. This article will explore contact lens alternatives including piggyback lenses, hybrid lenses, custom soft lenses, and mini-scleral/scleral lenses.
Piggyback Lenses
Perhaps the most efficient fitting option is the use of piggyback contact lenses. A piggyback lens system consists of a soft contact lens fit under a GP lens. Piggyback fitting is underutilized and is often thought of as a last resort. With the advent of singleuse lenses, silicone hydrogel disposable lenses, and high-oxygen-permeable (high-Dk) GP materials, piggybacking is gaining popularity.
Piggyback fitting can improve GP lens comfort and protect the cornea. Certain areas of the cornea such as a very steep apex of a keratoconus patient or nodules on a Salzmann's Nodular Degeneration patient may be prone to abrasions. Patients who have monocular keratoconus, excessive 3 o'clock and 9 o'clock staining, and cases of recurrent corneal erosions may also benefit from piggybacking. Piggyback lenses can improve patient comfort in cases of GP intolerance when the fit of the current GP lens cannot be further modified.
In addition to dramatically improving comfort, piggyback lenses can improve GP centration and fit. For post-surgical oblate corneas, a high-plus powered lens can bulk up the center of the cornea to facilitate GP fitting. For patients wearing a cosmetic or prosthetic soft lens, the addition of a GP lens may enhance optical quality and improve vision while maintaining cosmesis.
There are two distinct fitting approaches. The most common scenario is that of an otherwise satisfied GP lens wearer who over time develops intolerance. In such cases you can apply a soft lens under an existing GP lens and evaluate the fit (Figure 1). In other instances you can fit the soft lens first and perform keratometry or topography over the soft lens. The resulting measurements determine the GP fit.
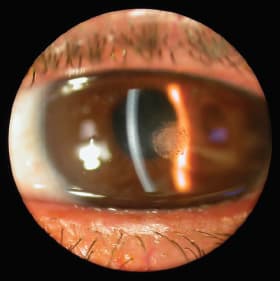
Figure 1. Calcium-like deposition at apex of cornea of a keratoconus patient who suffered from recurrent corneal erosions and was fit with a soft lens under an existing GP lens.
A successful piggyback lens fit is largely determined by the patient's comfort and tolerability of the lenses. Avoid GP lens binding on the soft contact lens—the soft lens and the GP lens should move independently of one another. When possible, increase GP peripheral clearance; this increases tear flow between the two contact lenses. Traditionally, only high-molecularweight sodium fluorescein has been used to evaluate piggyback lenses, but now 0.6mg sodium fluorescein strips are becoming more accepted (Figure 2). Observe the fitting relationship for bubbles between the soft and GP lenses. Central bubbles indicate a steep fit while peripheral bubbles can indicate a flat fit.
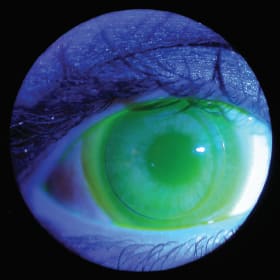
Figure 2. Piggyback lens evaluation with sodium fluorescein and a Wratten filter.
When selecting a soft lens, there are a number of factors to consider. Soft lenses, especially in advanced keratoconus patients, may exhibit edge standoff or fluting (Figure 3), which will decrease patient comfort. Soft lenses that have steeper base curves are necessary in these more advanced cases. Using higher-Dk materials for both the soft and the GP lens can minimize hypoxia issues such as corneal edema and neovascularization. The power of the soft lens does not affect the overall power of the piggyback system. In most instances, a low-powered plus or minus lens is chosen. In cases of extremely flat or steep corneas, using higher lens powers provides a flatter or steeper fitting surface and enhanced GP fitting.

Figure 3. Soft lens on a post-penetrating keratoplasty patient with a piggyback fit that shows edge fluting.
In cases in which standard silicone hydrogel lenses fail to provide an adequate fit between the soft and GP lenses, a specialized soft carrier lens may be beneficial. The Flexlens (X-Cel Contacts) piggyback has an anterior cutout that holds the GP lens and is now available in a silicone hydrogel material. Another specialized soft lens is the Recess Pillow Lens System (Fusion Contact Lens, Inc.) Although not yet commercially available, the design holds the GP within the soft lens pillow, aiding centration and minimizing GP movement.
Hybrid Lenses
While piggyback lenses are generally successful, patients may find using two lenses cumbersome or they may continue to experience problems with lens comfort or fit. In these instances, a hybrid lens—a GP lens with a soft skirt—can provide another alternative. The soft skirt can aid in patient comfort and lens fit. First- and second-generation hybrid lenses, the Saturn (Precision-Cosmet) and SoftPerm (Sola/Barnes-Hind Inc., Ciba Vision) respectively, were useful but had a number of potential problems such as hypoxia, issues with junctional splitting, and limited parameter selection. Additionally, their design of one soft base curve and one corresponding GP base curve limited their fitting success on highly irregular corneas.
SynergEyes, Inc. has developed a platform of hybrid lenses that incorporates new technology in both lens design and material. These hybrid lenses differ from their predecessors in that they have a more durable soft/GP junction and an expansive choice of lens parameter fitting options.
The company's newest design, Duette, also offers a silicone hydrogel skirt with improved oxygen transmission. The standard SynergEyes A lens is made primarily for normal corneas, but can be used with some levels of corneal irregularity or early keratoconus patients. The KC lens is designed for patients who have more advanced keratoconus. It is most successful with central nipple cones or very central prolate corneas but is not recommended for patients who have decentered or peripheral ectasia.
To address these concerns, SynergEyes introduced ClearKone in 2009. The ClearKone lens incorporates a reverse geometry design and is fit based on corneal vault. The center of the lens is fit on alignment while the steeper curve of the lens is positioned more peripherally on the GP portion of the lens. The reverse geometry design improves fitting on patients who have inferior displaced cones, decreases the build-up of a high-plus tear lens under the GP portion, and aids in lens removal.
Topography or keratometric measurements are useful but not necessary in fitting this lens; however, a fitting set is mandatory. A 10mm corneal vault is optimal (Figure 4), and corneal touch should be avoided (Figure 5). The bowl of the lens is filled with preservative-free saline solution and Fluoresoft (Sigma Pharmaceuticals) or swirled with a 0.6mg fluorescein strip. Failure to fill the lens bowl fully may result in air bubbles under the lens. Massaging or manipulating the lens on the eye cannot eliminate these bubbles; the contact lens must be reapplied. Thus, proper application techniques are critical. Allow the lens to sit for three to five minutes for optimal fluorescein evaluation. Early evaluation may give a false steep reading, while waiting too long often yields fluorescein washout and an artificially flat pattern.

Figure 4. An optimum ClearKone fitting relationship on a very steep keratoconic cornea. This patient was unsuccessful with GP lenses because of discomfort and frequent lens dislodgement and loss.
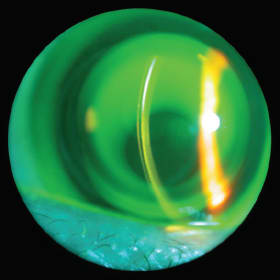
Figure 5. ClearKone hybrid lens that exhibits an excessively flat fitting relationship requiring a steeper vault.
When trial fitting, patient comfort is critical in predicting fitting success, unlike traditional GP lenses. The best-fitting lens will be the most comfortable lens for the patient. Be aware when refitting a patient from a GP lens to a hybrid design—a corneal remodeling effect may take place. The cornea may steepen after discontinuing GP wear, therefore necessitating a steeper vault than what trial fitting initially predicted. The ClearKone lens is adaptable to a variety of patients including PMD, corneal transplant, or post-refractive surgery patients (Figures 6a and 6b), but may not be successful for more oblate corneas.

Figure 6a. A post-refractive surgery patient who had a poor outcome after several enhancements. This patient was GP intolerant and was unsuccessful in a piggyback combination but was refit successfully into the ClearKone hybrid design.

Figure 6b. Topography of patient in 6a.
SynergEyes also has a reverse geometry PS (postsurgical) lens design for cases in which the central cornea curvature is very flat compared to the midperiphery and periphery of the cornea. The PS design has a large number of lens parameter combinations and can be the most difficult of the SynergEyes lenses to fit. The PS lens, like the KC and ClearKone lens designs, requires a fitting set that includes a range of base curves, skirt curves, and three levels of reverse curves.
Mini-Scleral, Semi-Scleral, and Scleral Lenses
Modern day semi-scleral and scleral contact lenses are gaining in popularity as diagnostic fitting, lens designs, and materials have improved. Patients who experience problems with comfort or who are unable to achieve proper fit with other contact lens alternatives can benefit from going beyond the limbus. Although scleral lenses are recognized for therapeutic purposes in patients who have compromised corneas and/or scleras (Stevens-Johnson syndrome, graft verses host disease, neurotrophic keratitis, etc.), more practitioners are using them on irregular corneas for vision correction (Romero-Rangel et al, 2000; Segal et al, 2003).
Mini-scleral and scleral lenses align and land on the scleral conjunctiva; therefore, they do not rely on the cornea for stabilization and support. Large amounts of corneal irregularity and fragile, more delicate corneas can be bathed in a reservoir of fluid beneath the central portion of the lens vaulting over the corneal surface. With the growing number of manufacturers producing mini-scleral and scleral designs, accessibility to new scleral technology is better than ever.
There are three primary objectives in fitting a mini-scleral/scleral lens: the lens must vault the cornea, clear the limbus, and land evenly in alignment with the scleral conjunctiva (Figure 7). Diagnostic fitting determines the amount of corneal vault necessary to avoid any corneal touch. Depending on the design, whether the lens is fenestrated, and the lens diameter, corneal clearance recommendations can vary from a minimum of 10 to 30 microns up to 200 to 350 microns. Limbal clearance appears as a bright fluorescent band. Bubbles in either the central or limbal zone indicate excessive clearance or poor application technique. The lens should rest evenly on the scleral conjunctiva. It is important to check for vessel impingement or compression as a sign that the peripheral zone needs to be modified.
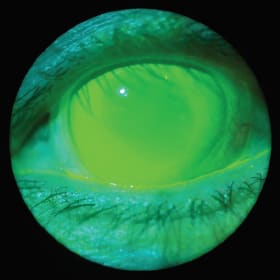
Figure 7. Post-penetrating keratoplasty patient who exhibited GP intolerance, successfully fit into the Jupiter (Visionary Optics) mini-scleral design.
Scleral lens designs are evolving, and manufacturers are able to offer more advanced design options including toric peripheral curves, front toric correction, and reverse geometry designs within a variety of lens diameters.
Patients are often intimidated when seeing scleral lenses for the first time, especially if their experience is limited to corneal GP lenses. Once introduced to the comfort and vision benefits of mini-scleral and scleral lenses, the intimidation factor disappears.
Custom Soft Lenses
In clinical practice most soft contact lenses are not an option for patients who have irregular corneas; however, specific custom soft lens designs are available for exactly these patients. The center thickness of the lens is increased and is significantly thicker compared to a standard soft lens to mask corneal irregularity. There is a vast range of both spherical and cylindrical powers encompassing most prescriptions in addition to a multitude of base curve and diameter choices. Proprietary designs with varying peripheral curves and optical zone diameters can be used for both prolate and oblate corneas. Four of the current custom soft designs for irregular corneas include Kerasoft IC (UltraVision CLPL), Flexlens (XCel Contacts), and HydroKone and RevEyes (both Visionary Optics, formerly Medlens Innovations).
The Kerasoft IC (irregular cornea) has an eightlens fitting set and is manufactured in both a hydrogel and a silicone hydrogel lens material. It has a unique Sector Management allowing for individually customized steeper and flatter sectors in the lens periphery. Although this contact lens is not yet available in the United States, it will be available in the future through distribution by Bausch + Lomb.
The Flexlens has both a tri-curve keratoconus design and a post-surgical design. As a lathed custom lens, it is fit based on a patient's keratometry measurements and refraction. An empirically designed lens serves as the first trial lens in the fitting process. These lenses are also available in both hydrogel and silicone hydrogel materials.
The HydroKone and RevEyes lenses both have diagnostic fitting sets available. HydroKone has three designs: standard, globus, and pellucid, depending on the area of ectasia or irregularity (Figure 8). RevEyes is designed for post-refractive surgery or oblate corneas. It has a flatter central curve and a steeper paracentral curve to match the contour of the cornea.
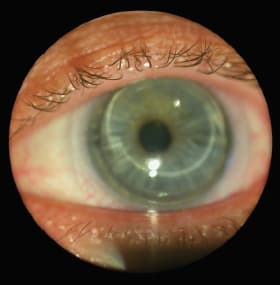
Figure 8. Pellucid marginal degeneration patient who could not wear GP or hybrid lenses, fit successfully into the HydroKone soft keratoconic lens design.
Conclusion
In our clinical practice, GP corneal contact lenses play a vital role in providing good vision for our irregular cornea patients. Unfortunately, not all patients achieve successful contact lens wear with corneal GPs. Contact lens alternatives such as piggybacking, hybrid lenses, custom soft lenses, and mini-scleral/scleral designs can help our patients who have corneal irregularity succeed where they have previously failed. These patients require their contact lenses to attain functional vision and therefore require our special attention. We owe it to our patients to utilize the latest contact lens technologies to help them succeed in their quest for good, comfortable vision. CLS
To obtain references for this article, please visit http://www.clspectrum.com/references.asp and click on document #186.

| Dr. Malooley is part of a group MD/OD practice and serves as adjunct assistant professor of the Illinois College of Optometry in the Department of Community Based Education. She is a GP Lens Institute Advisory Committee member. |

| Dr. Faron is part of a group MD/OD practice and serves as adjunct assistant professor of the Illinois College of Optometry in the Department of Community Based Education. |



