SURGICAL COMANAGEMENT
Surgical Comanagement and Contact Lens Fitting
Contact lenses can help some postoperative patients achieve their best potential vision.
By Gregory W. DeNaeyer, OD, FAAO
Advances in surgical instrumentation, devices, and techniques continue to improve outcomes for patients who undergo ocular surgery. A significant percentage of postoperative patients will require contact lenses to maximize their vision potential. Specialty contact lens designs are often needed to be successful with this patient population. This article will review contact lens strategies, materials, and designs that will help you fit or refit your patients who have undergone one or more ocular surgery procedures.
Corneal Refractive Surgery
Millions of patients worldwide have undergone corneal refractive surgery to correct their ametropia in the past 30 years. Although numerous surgeries have been utilized, the primary procedures have included radial keratotomy (RK), astigmatic keratotomy (AK), photorefractive keratectomy (PRK), laser epithelial keratomileusis (LASEK), and laser assisted in-situ keratomileusis (LASIK). Many of these patients require at least part-time refractive correction after their surgeries to address residual ametropia, regression, presbyopia, and corneal irregularity. For this patient population, contact lenses are a preferred corrective option.
Patients who have undergone hyperopic corneal procedures will have corneas that are prolate (relatively steeper in the center and flatter toward the periphery). Post-surgical corneas that are prolate are often successfully fit using standard soft or GP designs because the normal eyes that they are designed to fit are prolate in shape. However, aspheric designs are a good choice for an exaggerated post-surgical prolate shape. Spherical, toric, and multifocal contact lenses—in either soft or GP materials—would all be available options for these post-surgical patients.
For those patients who have undergone myopic refractive corneal surgery, their corneas are now oblate (relatively flatter in the center and steeper toward the periphery). Oblate corneas can be more difficult to fit with standard soft and GP lens designs. If the patient had 1D to 5D of myopic treatment, then his cornea will be only mildly oblate. In these cases, standard geometry soft lens designs that have a low modulus may adequately drape the corneal surface, and the lens should theoretically provide the patient with acceptable vision and comfort. If 6D or more of myopia was treated, then standard geometry soft lenses—especially lenses that have a relatively higher modulus—may not conform to the central cornea. This can leave such patients with fluctuating vision that is exacerbated as the upper lid blinks across the lens, which causes it to initially flatten only to have it trampoline back between blinks. If this is the case, then fit a reverse geometry soft lens design to adequately conform the soft lens to the oblate corneal surface. For corneal GP lens designs, patients who have oblate corneas of any degree will be most successful with a reverse geometry design because GP contact lenses are unable to drape the surface like a soft contact lens.

Figure 1. Corneal topography of the police officer's left eye.
Unfortunately, some post-refractive surgery patients can develop corneal irregularity secondary to a surgical complication or ectasia. Corneal GP lenses can successfully manage many of these patients if their cornea maintains a prolate contour. For corneas that have a more oblate shape or for extreme ectasia, a hybrid or scleral lens design is often a more successful GP alternative. Generally, these relatively larger lenses have better centration and stability compared to their corneal GP counterparts. In the case of an oblate cornea that has irregularity, reverse geometry scleral or hybrid lens designs will provide the best fit. Additionally if the irregularity is mild, then a specialty soft lens with an increased center thickness may adequately return patients to their best potential visual acuity.
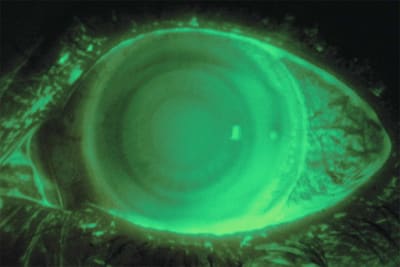
Figure 2. Reverse geometry soft toric contact lens.
Case Examples
• A 40-year-old police officer who had previous bilateral, eight-cut RK surgery 16 years prior to examination complained of decreasing vision. She was especially concerned because she was due to take a vision test to qualify for shooting. The patient's distance uncorrected acuity measured 20/50 OD and 20/30 OS. Refraction was OD +4.25 –2.75 x 163 20/20 and OS +1.25 –1.25 x 016 20/20. Topography (Figure 1) showed severely oblate corneas. We successfully fit the patient into soft reverse geometry toric lenses (RevEyes [Visionary Optics], hioxifilcon material [59 percent water]) with the following parameters: base curve 9.1mm, secondary fit curve 8.6mm, and diameter 14.5mm. The final power and vision was OD +2.50 –2.75 x 158 20/20 and OS +2.25 –1.75 x 044 20/20.
• A 45-year-old male patient complained of decreasing vision seven years after bilateral myopic LASIK surgery. The right eye had been originally targeted for near vision, and he reported having an enhancement surgery of this eye one year after the original treatment.
Manifest refraction was OD –1.50 –7.50 x 140 20/40 and OS –2.75 –0.25 x 99 20/20. Topography showed severe ectasia in the right eye and mild ectasia in the left eye. The patient's right eye was successfully fit with an 18.2mm diameter scleral contact lens (Jupiter [Visionary Optics], Boston XO [Bausch + Lomb]) that gave him 20/25 vision. His left eye achieved 20/20 vision with a standard geometry silicone hydrogel lens (Acuvue Oasys [Vistakon], senofilcon A [38 percent water]), with a base curve of 8.4mm and a power of –3.00 D.
• A 49-year-old female patient complained of decreased distance visual acuity since her myopic LASIK surgery 12 years prior. She had also undergone a limbal relaxing procedure of her right eye two months before her evaluation. The patient's right eye refraction was –1.50DS 20/20 and left eye was –0.75 –1.00 x 076 20/20. Because the patient was presbyopic, we fit a standard geometry silicone hydrogel toric contact lens to correct the left eye to distance. Unfortunately, the standard lens was unstable, so she was refit into a soft toric reverse geometry contact lens design (RevEyes, methafilcon material [55 percent water]) (Figure 2) with the following parameters: base curve 9.1mm, secondary fit curve 8.6mm, and diameter 14.5mm. The final power of –0.50 –0.75 x 080 gave the patient 20/20 distance vision through the left eye, and she was successfully able to use her uncorrected right eye for near vision.
Cataract Surgery
Although the primary purpose of cataract surgery is to remove vision-obscuring lens opacities, it has also become a secondary refractive surgery technique that can lessen a patient's dependency on glasses or contact lenses. Toric and multifocal intraocular lens implants are available for select patients. However, some postoperative patients may be able to enhance their surgical outcomes with contact lenses. Possible indications include correcting for residual ametropia, anisometropia, and presbyopia. Multifocal contact lenses can be an excellent alternative for those patients who have received monofocal implants or a multifocal implant in only one eye. Because most modern surgical techniques use small incisions for routine cases, the anterior ocular surface is rarely altered enough that it affects contact lens fitting.

Figure 3. Prosthetic aphakic soft toric contact lens.
Patients who are left aphakic can benefit from the optical and cosmetic benefits that contact lenses offer. Aphakic contact lenses have increased center thicknesses; therefore, using high-Dk materials is recommended when fitting either GP or soft lenses to decrease hypoxic-related complications. The thicker centers of aphakic lenses allow more superior lid interaction and lens movement. Choosing a slighter steeper base curve may be necessary to prevent excessive on-eye lens movement.
Patients who had a traumatic cataract may also have traumatic mydriasis secondary to their injury. Unfortunately, this may result in poor vision, glare, and photophobia even if an anterior or posterior chamber lens is successfully implanted. Prosthetic lenses are an ideal choice to improve symptoms and vision of these patients.
Case Examples
• A 47-year-old female patient who developed significant lens opacity of her right eye had a diffractive multifocal IOL (Tecnis [Abbott Medical Optics]) implanted during cataract surgery, which had an effective +3.00D add power. Her myopic left eye was without a cataract and she was successfully wearing a soft contact lens for distance vision. The patient's right eye postoperatively had uncorrected 20/20 distance acuity and 20/20 vision at 35cm. The patient was thrilled with her results except that she was having some difficulty seeing her computer at a working distance of 65cm. After discussion, we refit her myopic left eye with a multifocal soft contact lens (Acuvue Oasys for Presbyopia [Vistakon]), base curve 8.4mm, diameter 14.3mm, power –6.50D with a +1.50D add power. With this arrangement, she maintained her excellent distance and near acuity, but now was able to clearly see her computer screen at an intermediate distance.
• A 53-year-old male patient developed aphakia and traumatic mydriasis of his right eye after vitrectomy, lensectomy, and retinal reattachment surgery. He reported for contact lens evaluation four months postoperatively. After assessment and discussion, a soft toric prosthetic tinted contact lens (Figure 3) was ordered with the following parameters: base curve 8.2mm, diameter 14.5mm, and power +11.25 –1.25 x 007. The patient was able to achieve 20/50 vision of his right eye with the contact lens in place.
• A 37-year-old male patient was left aphakic in his right eye after a vitrectomy/pars plana lensectomy following ocular trauma. The patient had undergone 4D of myopic LASIK six years prior. We originally fit him with a standard geometry hydrogel contact lens with the following parameters: base curve 8.3mm, diameter 14.2mm, and power of +12.00D. The patient reported blurry and fluctuating vision with this lens at dispense with no improvement with over-refraction. A fluorescein pattern showed excessive central pooling. We switched the patient to a reverse geometry soft lens (RevEyes, methafilcon) with the following parameters: base curve 9.1mm, secondary fit curve 8.6mm, diameter 14.5mm, and power +12.50D. This lens dropped significantly, so we changed the secondary fit curve to 8.3mm, which improved lens centration. After an updated over-refraction that changed the lens power to +13.50D, the patient had 20/20 stable vision with comfortable lens wear.
Corneal Transplant
Patients who have severe corneal disease or scarring may require a corneal transplant to regain visual function. Corneal transplants can be subdivided into lamellar or penetrating keratoplasty (PK). Lamellar grafts replace only a partial thickness of the cornea and usually require only a few sutures, thus preventing large topographical changes or irregularity. A PK is a full-thickness transplant that initially requires 360 degrees of suturing to secure the graft to the host tissue. Unfortunately, for some successful PK grafts, the healing process can induce significant regular and/or irregular astigmatism. Additionally, the post-surgical resultant power after a PK can create intolerable anisometropia. These side effects may necessitate a contact lens to maximize the patient's visual results.
You should obtain consent of the corneal surgeon, and the eye should be stable without medically related complications, before beginning the fitting process. Waiting a minimum of six months postoperatively before contact lens fitting is prudent for most patients. Additionally, any exposed sutures that are broken or loose should be removed prior to contact lens fitting.
Soft contact lenses are an option for patients who have ametropia, regular astigmatism, or mild irregular astigmatism after corneal transplantation. Standard designed disposable soft contact lenses can be used for patients who have a normalized postoperative topography and little to no irregularity. However, specialty soft lens designs are often necessary for optimal results. Up to 30 percent of PK eyes will have an oblate shape postoperatively (Ibrahim et al, 1996), which may necessitate a reverse geometry design. Using latheable hydrogel or silicone hydrogel materials will allow you to increase the center thickness as needed to mask mild amounts of irregularity. Start with 0.3mm center thickness for transplants that have irregularity and consider using a silicone hydrogel lens material to reduce hypoxic-related complications.
Most patients who wear a contact lens after a corneal transplant do so because they develop surface irregularity and are subsequently fit with GP lenses. Corneal GP lenses are an excellent choice for patients who have mild-to-moderate irregularity. Large-diameter GP lenses (10mm to 12mm) offer a relatively broad weight distribution that can help improve centration, stability, and comfort. If there is excessive bearing or excessive decentration with a corneal GP, then switching to a scleral or hybrid lens will often improve the fit as lens bearing is transferred from the cornea to the sclera. Most of these irregular corneal transplant fits will be more dependent on sagittal depth rather than on keratometry values. However, topography is helpful in determining the overall shape, especially changes that occur at the graft-host interface. A reverse geometry GP or reverse geometry hybrid design may be necessary for optimizing the fit on a cornea that has an induced oblate geometry.

Figure 4. Corneal topography right eye of 44-year-old who underwent PRK and PK.
Case Examples
• A 44-year-old who underwent a PK of his right eye after having complications from a PRK surgery was interested in vision correction options. His uncorrected acuity was 20/60 OD and 20/25 OS. The patient's vision OD improved to 20/30 with a refraction of +3.00 –4.75 x 116. Topography of his right eye showed central corneal oblique astigmatism with significant midperipheral steepening (Figure 4). After discussing options, we diagnostically fit a reverse geometry soft contact lens (RevEyes, hioxifilcon) and ordered a lens with the following parameters: base curve 9.1mm (center thickness 0.2mm), secondary fit curve 8.6mm, diameter 14.5mm, and power +3.75 –4.75 x 125. The contact lens fits perfectly and provides the patient with 20/25 vision.
• A 69-year-old patient underwent previous Descemet's Stripping Automated Keratoplasty (DSAEK) of her right eye and a PK of her left eye secondary to Fuchs' corneal dystrophy. Her resultant refraction was OD +2.50 –1.25 x 022 and OS –3.25 +5.75 x 070. Topography OS showed oblique central corneal astigmatism and mild irregularity. The patient was referred for contact lens evaluation. Her left eye was successfully fit with a large-diameter GP lens (Dyna Z [Lens Dynamics], Boston XO) with the following lens parameters: base curve 7.03mm, diameter 11.2mm, and power –6.37D. With the lens successfully fitting her corneal transplant, she was able to see 20/30 with a –0.25D over-refraction. The patient wore progressive addition lenses in addition to her contact lens that corrected the ametropia of her right eye and incorporated the –0.25D over-refraction for the left eye. She had no problems with the remaining anisometropia, and she appreciated her improved acuity.
• A 68-year-old patient had best-corrected acuity of +6.50 –6.00 x 014 20/200 of her right eye post-PK for Fuchs' dystrophy. Corneal topography showed the right eye to have with-the-rule astigmatism with irregularity. An initial diagnostic attempt with large-diameter GP contact lenses failed secondary to poor fitting, so we fit a mini-scleral contact lens (MSD [Blanchard] Boston XO) (Figure 5) with the following parameters: sag 4.2mm with a 7.6mm profile, power +3.00D, diameter 15.8mm. She was able to wear the lens without problems, and it improved her visual acuity to 20/40.

Figure 5. Mini-scleral contact lens successfully fitting over a corneal transplant.
Conclusion
Contact lenses can play an important role in a patient's visual function after ocular surgery. In some cases contact lenses enhance postoperative patients' vision, and in other instances they may be required for patients to obtain their best potential vision. Consider both standard and specialty designed lenses in soft and GP materials to successfully fit the broad spectrum of surgically corrected eyes. CLS
To obtain references for this article, please visit http://www.clspectrum.com/references.asp and click on document #190.

| Dr. DeNaeyer is the clinical director for Arena Eye Surgeons in Columbus, Ohio. His primary interests include specialty contact lenses. He is also a consultant to Visionary Optics. Contact him at gdenaeyer@arenaeyesurgeons.com. |



