LENS OPTIONS
Toric and Multifocal Scleral Lens Options
Don't save scleral lenses for only the most difficult and irregular corneas when others may also benefit.

By Roxanna T. Potter, OD, FAAO
Historically, the primary goal in fitting patients who have irregular corneas or high refractive errors was to improve distance visual acuity in a tolerable corneal GP contact lens. Scleral lens technology has not only improved potential comfort while preserving GP optics and superior vision, but has progressed to also include multifocal and toric designs that can optimize any patient's quality of life in contact lenses.
If a practitioner considers standard spherical scleral lenses as difficult “specialty” lenses, the thought of fitting toric and multifocal scleral lenses may be overwhelming. However, the additional effort required to fit a toric or multifocal scleral lens is actually very minimal once a patient has been fit in an appropriate standard scleral or semi-scleral trial lens.
With a basic understanding of scleral lens fitting and access to a fitting set, practitioners can now offer patients of almost any refractive status comfortable contact lens wear and excellent, versatile visual acuity at all distances. Toric and multifocal scleral options are no longer just possible, they are readily available and growing in popularity. As many contact lens fitters are beginning to realize, scleral lenses are not just for irregular corneas anymore, and multifocals and torics are not just for regular corneas.
Toric Scleral Lenses
One of the advantages of semi-scleral or scleral lenses is that a spherical scleral design can correct larger amounts of both regular and irregular corneal astigmatism as compared to standard spherical corneal GP lenses. By vaulting the corneal surface, even large amounts of corneal toricity can be easily addressed in a spherical design without further toric calculations, such as in Case 1.
However, we need to make a distinction between toric refractive correction and toric fitting design. The need to add additional refractive astigmatic correction to a scleral lens should be rare except in cases of true internal astigmatism. When the need does arise, it is often determined based on the resultant over-refraction performed on a well-fitting scleral lens that cannot be contributed to flexure. If unexpected spherocylindrical over-refraction is a common result in scleral lens fitting, it's more likely that the lenses are being fit with excessive sagittal depth, inadequate central thickness, or have some other fitting problem that induces flexure.
Should there be a significant toric over-refraction that is not the result of flexure or a poor lens-tocornea fitting relationship, there is an option to add a front toric to a scleral lens in some scleral lens designs. As front-toric lenses require specific rotational position, it is advisable to seek the help of laboratory consultants who can offer valuable advice in designing lenses for these cases. A front-toric scleral lens sounds intimidating; however, once a scleral lens has been chosen and appropriate fit determined from a trial set, adding the spherocylindrical over-refraction and necessary stabilization adjustments are easily left to a consultant for completion. Depending on the laboratory and design, stabilization options vary from double slab-off, prism ballasting, or truncation modifications. While there is no consensus on the “best” way to stabilize a front-surface toric scleral, consultants can guide you to what is most successful according to their design research and experience.
Toric fitting designs differ from toric refractive options in scleral lenses in that they are generally not used to directly improve visual acuity, but instead to better fit a toric sclera. While the shape and toricity of the human sclera still requires much research, many practitioners are finding that perfectly symmetrical scleral shape is the exception rather than the norm. Toric fitting adjustments can be made to the peripheral curves (also known as the landing zone) of scleral lenses to help better align the lens with the patient's ocular surface. This has little to do with corneal toricity; in fact, it is not unusual for a patient who has a spherical cornea to require a toric periphery in a scleral lens, or a quadrant-specific adjustment to a peripheral lens section. Back-surface torics (across the central base curve only or continuing through the periphery) have a limited availability but are generally not necessary in scleral lens fitting for improving acuity or fit. Table 1 lists a few examples of available semi- and full scleral designs that allow for toric modifications (both refractive and fitting).
| TABLE 1 | ||||
|---|---|---|---|---|
| Toric and Multifocal Scleral Lens Availability (Not Comprehensive) | ||||
| Design | Front Toric | Peripheral Toric | Multifocal | Other Options |
| Maxim Scleral (Accu Lens) | Yes | No | No | �A0; |
| Dyna Semi-Scleral (Lens Dynam ics) | Yes | Yes | Yes (aspheric) | Quadrant-specific periphery |
| Digiform and Tru-Scleral (Truform Optics) | Yes | Yes | Yes (center-near) | Quadrant-specific periphery,back toric |
| So2Clear (Dakota Sciences, Art Optical/Metro Optics) | No | No | Yes (center-near) | �A0; |
| Jupiter Scleral (Various Distributors) | Yes | Yes | No | Quadrant-specific periphery, back toric |
To determine whether a toric periphery is necessary, when evaluating the fit of a semi-scleral or scleral lens, be careful to look for appropriate alignment of the peripheral lens against the sclera in all 360 degrees of lens coverage. Compression or impingement, or excessive edge lift or stand-off that differs in one meridian or quadrant from another, may be best addressed using a toric periphery. If the problem appears to occur throughout most of the periphery, or is accompanied by any decentration, a uniform change to peripheral curvature, base curve, or diameter may be more appropriate. Be sure to check for this after the lens has had sufficient opportunity to settle. Toric peripheral curves will align naturally on a toric scleral surface if used appropriately and do not require special patient application techniques or stabilization designs. If available (though certainly not required), anterior optical coherence tomography (OCT) visualization of the periphery of a scleral lens can help determine whether a lens is aligned with the sclera symmetrically around the circumference of the lens (Figure 1).
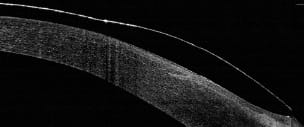
Figure 1. Anterior optical coherence tomography.
Bitoric scleral lenses combine toric peripheries and front-surface cylindrical design (note the difference in the meaning of bitoric when compared to bitoric front/back surface corneal GPs). Again, check with your preferred laboratory to determine whether it offers these options on scleral lens designs, and use consultants as a source of experience and knowledge in designing these lenses. Once you've accomplished a basic scleral fit from your fitting set, asking for a toric periphery or giving a spherocylindrical over-refraction to a fitting consultant is no more difficult than asking for a minor correction to any GP lens, such as enlarging the optical zone diameter on a corneal GP lens for keratoconus or raising the seg height on a translating GP bifocal.
Case #1
A 57-year-old white male presented desiring contact lens wear despite previous failures in multiple lens modalities. He reported poor vision in soft toric lenses and better vision but poor comfort in bitoric corneal GP lenses. He admitted that he only desired part-time wear for sports and occasionally for social activities, that he had never adapted to GP wear fully due to intermittent use of the previous lenses, and that he didn't wear them full time because of the hassle of needing reading glasses over the lenses.
He also had a history of mild bilateral refractive amblyopia. Best corrected visual acuity with a refraction of +8.25 –4.75 x 164 was 20/25 OD and with +8.00 –5.00 x 005 was 20/25 OS. Corneal topography revealed with-the-rule toricity as shown in Figures 2 and 3.

Figure 2. Case #1 topography OD.

Figure 3. Case #1 topography OS.
When the corneas are similar in size, shape, and curvature between the eyes, I will often start with one eye and then make any desired changes by using the next lens in the other eye, leaving the first lens applied when possible to compare side by side. Then any final changes are made to both lenses prior to placing any order.
Beginning with an 8.03mm base curve radius (BCR), 14.0mm overall diameter (OAD), So2Clear mini-scleral lens OD (Dakota Sciences/Art Optical/Metro Optics), the patient was immediately surprised at how comfortable the lens was. It centered well with complete corneal and limbal clearance and no scleral impingement or compression. After the lens was allowed to settle, however, the peripheral fit of the lens appeared slightly tight around the entire circumference of the lens, so the next eye was fit with a slightly flatter 8.13mm BCR. This decreased the overall sagittal depth of the lens, which created less pressure out in the periphery where the lens rested on the sclera while maintaining sufficient corneal and limbal clearance. After an over-refraction was performed and vertexed OD and OS, the lenses ordered had parameters of OD 8.13mm BCR, 14.0mm OAD, +5.75D and OS 8.13mm BCR, 14.0mm OAD, +5.25D with a +2.25D add OD and OS. Due to a slight cylindrical component found in the over-refraction, the center thickness of the lens was increased to prevent flexure.
At the first follow up, the patient presented after having worn the lenses for a few hours and reported mild distance and near blur, but good comfort and no problems with application or removal. More plus over-refraction was found, likely due to further settling of the lenses and loss of some of the application tear prism; therefore, new lenses were ordered. After these were dispensed, the patient returned with improved vision of 20/30 OD and 20/30 OS, OU 20/25 distance and near. He complained only of mild haziness after eight hours of wear. This was likely due to debris build-up or end-of-day dryness, so a mid-day removal, rinse, and refill was recommended as needed for longer wearing times. As is typical of simultaneous multifocal designs, visual acuity was expected to improve with further adaptation.
Two years later, the patient has remained quite pleased with his contact lenses. They have exceeded his desired goal of part-time wear, as he now wears them all day at work with the ability to read almost everything quite comfortably without requiring reading glasses.
Multifocal Scleral Lenses
Perhaps even simpler to fit than toric designs, multifocal semi-scleral or scleral lenses offer patients of all corneal types a multifocal lens option. It can be very rewarding to give keratoconus patients or any patient who has irregular corneas the opportunity to not only improve their distance vision in a GP lens, but to also have a multifocal correction. Occasionally, it may not be advisable to further compromise visual acuity with multifocals, but in many cases aspheric GP designs are used to better fit irregular corneas, which can actually unintentionally induce a multifocal effect. Post-refractive surgery patients in particular are often very motivated to gain near correction without readers, as in Case 2.
On regular corneas, multifocal scleral lenses exhibit some of the best properties of both GP and soft multifocals. Because scleral lenses have little to no lens movement, they are not expected to translate and therefore require simultaneous multifocal designs: concentric or aspheric. The So2Clear lens, like many scleral multifocals, has a center-near design. Although not exactly the same, the center-near concept is one that many are familiar with from many soft multifocal designs. Fine-tuning visual performance in a multifocal scleral lens is, in many ways, more similar to soft multifocal techniques than to previous corneal GP multifocal problem solving. Changes in BCR, overall diameter, or other fitting properties are limited on most regular corneas, maintaining centration is not generally an issue, and translation is not required. These lenses are also highly customizable, offering ranges of refractive correction to many patients.
Case #2
This case involves a 60-year-old white female with a history of laser-assisted in situ keratomileusis (LASIK) OD and OS five years prior to her examination. She was wearing soft multifocals somewhat successfully but noted increasing dryness and difficulty seeing and handling the lenses, with frequent folding and loss of lenses. She desired something that was easier to handle, clean, and apply, and that would provide better vision at all distances. It was decided that a semi-scleral lens was an excellent option, provided that a reverse geometry fit wasn't found to be necessary, as this would have eliminated the multifocal option available at that time.
Her refraction was +1.25 –0.75 x 120 (20/20) OD, and +1.25 –0.50 x 061 (20/20) OS with a +2.25D add OD and OS. Topographies (Figures 4 and 5) revealed an oblate corneal shape OD and OS. Knowing that the patient had an average scleral shape despite her surgically flattened corneas, and experiencing difficulty obtaining a good central and peripheral lens-to-cornea fitting relationship with lenses from the standard fitting set, the first lenses ordered were from a combination of trial and empirical fitting.

Figure 4. Case #2 topography OD.

Figure 5. Case #2 topography OS.
The fitting set lenses, when fit with an appropriately flat BCR, exhibited decentration and undesirable edge lift from peripheral curve radii (PCR) that were too flat in curvature. The initial power chosen was determined using over-refraction on a lens with sufficient central base curve corneal vaulting (no bubbles) but poor peripheral alignment; however, this was still worth attempting to obtain a more accurate refractive starting point. The lenses ordered were OD 8.43mm BCR, 14.0mm OAD, plano and OS 8.33mm BCR, 14.0mm OAD, –1.00D with +2.25D add and 44.00D PCR OD and OS.
At the first follow-up visit after dispensing, tightening was noted OD and OS along with poor near visual acuity OS. After the PCR were flattened 1.00D OD and OS and the size of the central near zone of the left lens was increased slightly, the patient was able to obtain 20/20 visual acuity at both distance and near and more than 12 hours of comfortable lens wear.
Take note that in both cases presented in this article, the lenses could have been fit without topography. In fact, a standard or even a loaner semi-scleral lens fitting set may be all that is required to fit patients of various toric and multifocal corrections. With the So2Clear standard fitting set, I often choose the same initial diagnostic lens, found in the middle of the set, regardless of keratometry or topography readings and ignoring base curve recommendations. Once the peripheral fit of the lens is assessed, corneal vaulting/clearance is evaluated, and only then are changes in BCR made. The necessity of toric PCR is determined based on lens fitting observations, as scleral anatomy measurement is unobtainable with corneal topographers. If the patient is known to have a particular corneal shape, then the initial diagnostic lens can be adjusted slightly flatter or steeper in BCR to save time; however, scleral shape and peripheral lens fit is less directly related to corneal condition, and the same initial diagnostic lens will often be a sufficient starting point. Other scleral lens designs simplify this concept further and recommend lenses be fit with a single or limited starting peripheral design and adjustments made in terms of sagittal depth.
Conclusion
Saving scleral lenses for only the most difficult and irregular corneas can be a disservice to other scleral lens candidates. Patients who have all forms of astigmatism can be fit in standard spherical or front-surface toric scleral lenses, and patients who have both regular and irregular corneas can be given access to multifocal correction. The option of toric PCR has made it even easier to fit more patients, and with these tools we can continue to gain confidence in fitting these lenses by trying them more often on patients who have both regular and irregular corneas. CLS
| Dr. Potter owns a private practice in Sylvania, Ohio. She enjoys fitting, writing about, and lecturing on specialty contact lenses. She can be reached at rpotter@personaleyecare.com. |



