Contact Lens Care & Compliance
Contact Lens Deposition and Dry Eye

By Susan J. Gromacki, OD, MS, FAAO
We all have patients—perfectly content with spectacles—who struggle with comfortable contact lens wear. We diagnose dry eye, but how closely did we evaluate the condition of the lenses? That might be our key to solving the patient's dryness and discomfort problems.
Deposited Lenses
Contact lens wear can exacerbate dry eye in some patients. The contact lens splits the tear film into pre-lens and post-lens tear layers. The thinner pre-lens layer now can evaporate more readily than before, particularly in a dry eye environment. Deposited lenses compound the problem. Deposition provides physical resistance to an even tear flow over the lens, causing an even more premature tear breakup. In addition, it creates mechanical discomfort by irritating the palpebral conjunctiva of the upper eyelid, adding to the symptoms that are already present due to the dry eye.
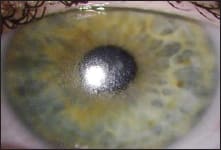
Figure 1. Deposition on a hydrogel contact lens.
Many practitioners, eager to treat the dry eye medically, have a disconnect regarding deposited lenses in dry eye patients and their impact on increased symptoms and decreased wearing time. However, the literature contains several studies that support the link between deposited lenses and dryness/discomfort (Subbaraman, 2010; Richdale, 2007; Brennan, 2000; and others. For complete list visit clspectrum.com.) Other papers reported decreased wettability as a result of the deposition (Lorentz, 2007; Bleshoy, 1994). This may be due to the deposits' physical presence, in combination with the fact that lens deposition may alter tear composition and physiology (Thai, 2004). Ultimately, lens discomfort, often from deposits, is a primary reason for discontinuing lens wear (Riley, 2006; Richdale, 2007; Sankaridurg 1999; and others. For complete list visit clspectrum.com.)
Treatment
The lens deposition arises from the tear film—proteins, lipids, mucins, and inorganics—and begins within minutes of lens application (Nichols, 2006). To best eliminate the deposits, it is helpful to understand their composition. First of all, traditional polyHEMA-based materials tend to deposit proteins more readily, while lipid deposition tends to be more prevalent with silicone hydrogel lenses (Jones, 2009; Gromacki, 2012).
In general, first treat any blepharitis or meibomian gland dysfunction to improve the quality of the tears. Secondly, instruct patients to rub and rinse their lenses (Nichols, 2006). If rubbing with a multipurpose solution does not resolve the problem, then add a surfactant cleaner. Next, consider refitting patients into a more deposit-resistant material (Jones, 2009). Lastly, consider a shorter replacement schedule, such as with daily disposable contact lenses.
Keeping Lenses Clean
A clean contact lens surface goes a long way in aiding patient comfort and satisfaction, particularly in dry eye patients. CLS
For references, please visit www.clspectrum.com/references.asp and click on document #200.
| Dr. Gromacki is a diplomate in the American Academy of Optometry's Section on Cornea, Contact Lenses and Refractive Technologies and practices in Lutherville, Md. |



