Reader and Industry Forum
An Unusual Case of Acute Corneal Hydrops

By Bezalel Schendowich, OD, FIACLE
The Association of Contact Lens Educators (AOCLE) Living Library describes acute corneal hydrops as “an uncommon complication seen in patients with keratoconus. It is characterized by significant corneal edema resulting from a spontaneous rupture in Descemet's membrane. Clinical findings include dense stromal and epithelial edema with corneal protrusion, possible conjunctival hyperemia and irregular epithelium secondary to microcystic edema. The location and area of the involved cornea is variable.”
Patients typically report sudden onset of monocular visual impairment, ocular irritation or pain, photophobia, and tearing. Patients frequently notice corneal opacification observable by the unaided eye (AOCLE).
In general, sources report that after treatment most hydrops-related scarring absorbs, and vision can be better than what it was before the hydrops incident. With a flatter corneal topography, these eyes can be somewhat easier to refit with contact lenses compared to before the hydrops.
I wish to report a case of acute corneal hydrops that is unusual in that after healing, the cornea predominantly cleared of scarring and then went on to progression of the ectasia.
Patient History
In fall 2000, our patient first presented as an 11- year-old boy who had itchy allergic eyes and a history of eye rubbing. His referral was for suspected keratoconus and a need for new glasses.
Refraction at that time demonstrated poor retinoscopy reflexes, moderate astigmatism, and visual acuity of around 6/15 (20/50) in each eye. Keratometry and corneal topography evidenced corneal irregularity and steepness (Figure 1). We suggested a contact lens fit. The fit was successful with vision increased to around 6/7.5 (20/25) in each eye.
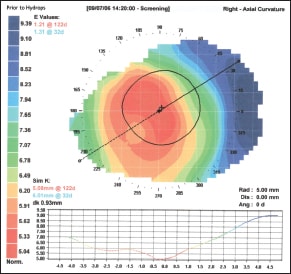
Figure 1. Pre-hydrops topography. Note on the figures: the topography images are normalized to the same scale to emphasize changes in the corneal surface topography.
As our patient grew up, we followed him and changed his contact lenses and lens designs from time to time. By May 2009 he was using a KBA (Essilor, Precision Technology Services) contact lens design (4.85mm base curve radius [BCR], 10.2mm overall diameter [OAD], power of –25.75D, and eccentricity of 1.55), which when dispensed gave him approximately 6/9 (20/30) visual acuity.
Soon after, he phoned with the complaints of pain and vision reduced to light perception in his right eye with his lens in place. I asked him to come in to show me, upon which acute corneal hydrops was quickly diagnosed.
Post-Hydrops Management
Initial treatment consisted of a systemic diuretic to drain fluids from the cornea as well as from the rest of the body; a steroid-antibiotic combination drug to reduce inflammation and to protect from infection; and a prostamide to reduce intraocular pressure, thus producing a negative anterior chamber gradient to reduce fluid movement across the endothelium and Descemet's membrane into the stroma. Figure 2 shows the hydrops scar.
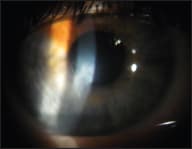
Figure 2. Hydrops scar.
By the end of July the scarring had subsided, and by mid-August I was able to refit using a substantially different KBA lens design (6.20mm BCR, 10.2mm OAD, –13.75D, eccentricity of 1.30). The lens was much flatter and boasted a much reduced eccentricity value. The cornea was by comparison less hyperbolic. Good vision was again achieved, but the contact lens fit was only “as good as could be expected” considering the resultant very irregular corneal surface (Figure 3).
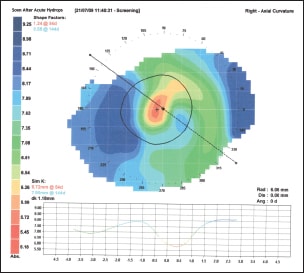
Figure 3. Early post-hydrops topography.
This patient is one of a multitude who remember their contact lens fitter only when something seems out of place. He returned a year later (2010) for examination. His contact lens was now very flat and loose, requiring an over-refraction of +1.75D. Remarkably and unexpectedly, to refit this eye with another KBA lens, I needed to steepen the BCR to 5.00mm. With this lens he complained about his quality of vision. I tried a series of larger corneal lenses and intra-limbal contact lens designs without success. Figure 4 shows the most recent corneal topography, and Figure 5 shows the partially resorbed hydrops scar.
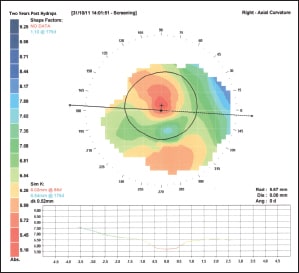
Figure 4. Most recent topography.
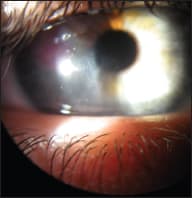
Figure 5. Partially resorbed scar.
I fit the eye with the MSD (Blanchard) mini-scleral design lens that in trials provided visual acuity of 6/9- (20/30-), which I considered a significant improvement. In addition, the lens was more stable and was unlikely to cause corneal insult. As a result, we were motivated to continue, especially considering the irregular surface involved.
At dispensing of his mini-scleral design lens, the patient's visual acuity was 6/6- (20/20-).
Table 1 shows a summary of the patient's contact lens fitting data.
| TABLE 1 Summary of Patient's Lens Fitting Data | |||||
|---|---|---|---|---|---|
| Date | K/Sim-K | Design | BCR | OAD | Power |
| 10/2000 Initial fitting | 6.94/6.46 | Rose K | 6.90mm | 8.7mm | –6.50D |
| 3/2007 Last prehydrops | 6.01/5.08 | KBA | 5.00mm | 10.2mm | –23.75D |
| 9/2009 First posthydrops | 7.90/6.72 | KBA | 6.20mm | 10.2mm | –13.85D |
| 10/2011 Current | 6.54/6.02 | MSD | 6.60mm (5.00-D) | 15.8mm | –10.75D |
Discussion
The literature representing world experience with acute corneal hydrops indicates that when controlled, the scarring caused by fluid leaked through a rupture in the endothelium and Descemet's membrane absorbs and clears, with the resulting corneal topography somewhat flatter and easier to fit with contact lenses. In a discussion addendum to Grewal et al (1999), Dr. Thomas J. Liesegang notes that “A recurrence of the hydrops is unlikely; the corneal ectasia, however, may continue…”
It is not clear whether Dr. Liesegang saw a case similar to the one presented here, but this case certainly bears out his supposition that ectasia may well progress after the initial incident has resolved.
Scanning our patient's corneal topography maps, we can clearly identify advanced keratoconus in the pre-hydrops image (Figure 1) with an ectasia encompassing some 80 percent of the mapped cornea. The post-hydrops images (Figures 3 and 4), however, are difficult if not impossible to interpret without a patient history. All that can be discerned directly is the presence of a central scar and a subsequent progression of the ectasia.
A Final Note
In conversation with the ophthalmologist who attended my patient during the active stage of his acute hydrops, I presented my findings of recurrent aggressive ectasia. He commented that the cornea was likely very weak and that our patient would very likely be requiring a corneal transplant in the not-so-distant future.
Referring again to the paper by Grewal et al, their study of 22 patients who had hydrops indicated that four (or 18 percent) later needed surgery within the restricted period covered by their investigation.
We shall wait and continue to follow our patient, working to provide him with the best vision possible without insulting his corneal integrity. He may yet have several years of use from his original cornea. CLS
Acknowledgement
As always, my respect and thanks must be expressed to my patients for choosing me to help them confront their visual adversities invoked by their corneal ectasias.
I should be remiss if I did not mention and thank the consultants at MSD Corp. and at Blanchard Contact Lens, Inc. for their advice in designing the MSD contact lens that I fit for this patient.
To obtain references for this article, please visit http://www.clspectrum. com/references.asp and click on document #196.
| Dr. Schendowich is a Member of the Medical Advisory Board of the National Keratoconus Foundation, USA, a Fellow of the International Association of Contact Lens Educators, and an adjunct assistant clinical professor of optometry at SUNY-Optometry in the ophthalmology clinic at the Sha'are Zedek Medical Center in Jerusalem, Israel. |



