TOPOGRAPHY SURVEY
A Survey of Consecutive Corneal Topographies
More than 1,700 patient records over four years illustrate one clinic’s disease frequency and progression.

| Dr. Schendowich is a Member of the Medical Advisory Board of the National Keratoconus Foundation, USA, a Fellow of the International Association of Contact Lens Educators, and an adjunct assistant clinical professor of optometry at SUNY-Optometry in the ophthalmology clinic at the Sha’are Zedek Medical Center in Jerusalem, Israel. |
By Bezalel Schendowich, OD, FIACLE
Perhaps the greatest boon to diagnosing and differentiating corneal anomalies since the slit lamp has been the computerized video-keratographer or corneal topographer. Since the early 1990s when these devices first began to appear, corneal diagnosis and condition progression, contact lens fittings, and results of corneal surgery have all become much more objective and founded upon calculations rather than on keratometer readings, which in cases of complicated corneae can be largely irreproducible and certainly unreliable.
I practice in the ophthalmology clinic of a major metropolitan hospital. Our clinic topographer holds in memory several thousand patient records, many of which document change secondary to disease progression, surgical treatment, or contact lens usage. A survey of these mappings yields data describing the frequency of various conditions seen in our clinic. While this information cannot be used to generate incidence data in the general population because of our clinic’s skewed patient population, we can see the relative frequencies of these various conditions with reference to each other.
Probably the only major category of corneal condition that is grossly under-represented in this survey is the normal or only minimally astigmatic cornea. This can be explained by observing that many such eyes see well and may not be examined on a regular basis by any eyecare practitioner. This category also includes those with low or minimal refractive errors corrected to good or excellent visual acuities and for whom a topography mapping wouldn’t have been ordered.
In contrast, we have made a rule that we’ve become more careful in keeping over the years that the corneae of all new contact lens patients are mapped as we begin the fitting process to help us better design the shape of contact lenses that will fit most forgivingly to their corneae. This has helped to improve our normal cornea statistics. On the other hand, because we are located in a busy hospital clinic, the proportion of normal corneae found in our overall patient population is much smaller than that which would be found in practices that have more popular, mainstream exposure.
Review of Corneal Topography Maps
Retrospectively, I categorized the corneal maps of 1,711 patients. This count does not include low astigmats, otherwise normal corneae, a variety of traumatized corneae, post-refractive surgery corneae, post-penetrating keratoplasty corneae, and pterygia.
This retrospective chart review is in accordance with the tenets of the Declaration of Helsinki.
The breakdown of corneal conditions represented by our survey includes:
• High regular astigmatism (HRA, Figure 1)
• Keratoconus (KC) (nipple, oval, and forme fruste; including secondary ectasia, Figures 2 and 3)
• Pellucid marginal degeneration (PMD, Figure 4)
• Global keratoconus (GK—not keratoglobus, Figure 5)
• Keratoconus—superior (Figure 6)
• Keratoconus—lateral (Figures 7 and 8)
• Corneal warpage (CW)
I have arbitrarily defined the cut-off for high regular corneal astigmatism to be around 3.00D depending on the other eye and how dominant the cylinder appears in the topograph.
Forme fruste keratoconus (KCff) describes a corneal topography similar to traditional keratoconus in that there is an area, generally in the inferior hemicornea, which is steeper compared to the surrounding area. The difference is that the degree is far less; the ‘ectasia’ does not progress and refraction is stable, while visual acuity may well be 20/20. Retrospective analysis of topographies cannot accurately differentiate KCff from incipient or mild KC—a history is required. The history will answer the diagnostic question of measured or perceived change over time. For this reason, I have combined all those patients whose topographies hint at KCff within the greater classification of traditional KC.
A recent review article in Contact Lens and Anterior Eye (Jinabhai, et al, 2011) describing PMD remarks that it is a rare diagnosis. Our survey agrees with that observation in that roughly 3 percent of our non- ‘normal’ population exhibits PMD. I would like to suppose, however, that PMD is actually more common than what series topographies of an eye clinic will show.
The locus of the ectasia in PMD is from four o’clock to eight o’clock close to the inferior limbus. In early PMD, distortion would hardly be apparent with the retinoscope and thinning would be difficult to see with the slit lamp. Other than a certain amount of astigmatism that increases and becomes more irregular as the condition progresses, early PMD would be more likely a missed diagnosis. These patients tend to see well and sometimes have only nominal refractions. Many of them have been diagnosed only when seeking refractive surgical solutions for their ametropia.
GK describes a gross ectasia characterized by full or nearly full corneal involvement. The keratoconus index, or I/S value, indicates that KC may be present when the relationship of inferior to superior corneal power exceeds around 1.5D (Medmont E300 manual). Many of the corneae that I have categorized as GK boast an I/S value of 15.0D or more. On inspection of their apical power or curvature maps, we see a huge inferior steep area matched by a nearly as large superior flat area, notable for the gross disparity in shape between them. This can be appreciated by the huge change in curvature in the corneal profile graph below the topography (Figure 5).
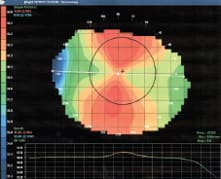
Figure 1. High regular astigmatism (5.8D by sim-K). The calculated I/S for this eye is −0.01D.
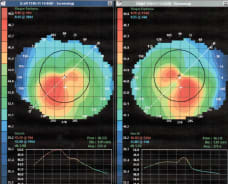
Figure 2. A patient who has moderate keratoconus with irregular corneal cylinders of 4.00D and 5.00D. The I/S here for both the right eye and the left eye is 2.88D.
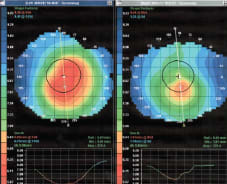
Figure 3. A patient who has a more concentrated and a more diffuse central cone. The I/S values here differed: OD 1.99D, OS 2.47D.
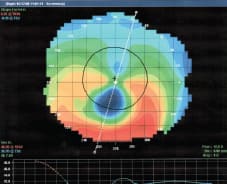
Figure 4. A classical presentation of a PMD cornea, I/S = 2.77D.
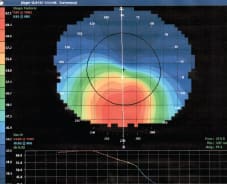
Figure 5. A nearly full corneal ectasia—Global Keratoconus with an I/S value of 12.79D.
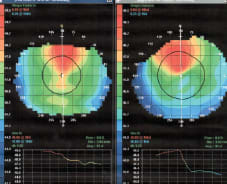
Figure 6. Superior keratoconus with I/S values of −1.90D and −0.90D.
The big surprise for me was the frequency of superior and lateral asymmetries, which I have taken the liberty of labelling superior and lateral keratoconus, respectively. Just to make the observation more interesting, lateral asymmetry can be either temporal (Figure 7) or nasal (Figure 8). I did not pick up any right or left homonymous ectasiae.
Table 1 shows the occurrence data divided according to these definitions and conventions.
Conclusions
The proportional data presented relates the various corneal anomalies to each other and not to the whole population. Therefore, while the available statistics show that keratoconus may occur in 0.25 percent of the general population, my survey of KC as a part of the specific sub-population of ectasia and other corneal distortions shows a frequency that is explicably far higher (around 64 percent of the group I chose to investigate).
Primary corneal ectasiae occur in busy ophthalmology clinics more commonly than they do in the general population. My results culled from roughly four years of topography mapping summarizing more than 1,700 patients show by far that the largest population sub-grouping from among those I have defined is of traditional keratoconus (including nipple, oval, and forme fruste varieties). The fringe subgroupings of superior, lateral, global keratoconus, and PMD all show pretty nearly the same proportion, and their frequency is significantly smaller compared to the traditional KC group.
| TABLE 1 Occurrence Data Divided According to Definitions and Conventions Explained in the Text | ||
|---|---|---|
| COUNT | ROUNDED PERCENTAGE | |
| High Regular Astigmatism | 324 | 19 |
| Keratoconus including likely forme fruste | 1,098 | 64 |
| Pellucid Marginal Degeneration | 49 | 3 |
| Global Keratoconus | 48 | 3 |
| Superior KC | 100 | 6 |
| Lateral KC | 22 | 1 |
| Corneal Warpage | 70 | 4 |
| Total | 1,711 | 100 |
My analysis included two groups of variations of normal corneae because these often complicate the differential diagnosis of KC: high regular astigmats and corneal warpage.
The HRA sub-group was largely derived from referrals for topography and refraction to rule out ectasia from clinics where these services are not provided. It is quite likely that there is a far larger frequency of HRA in the general population than in my survey because many will have their refractive needs cared for by their primary eyecare practitioner and will not have required referral to our secondary level facility.
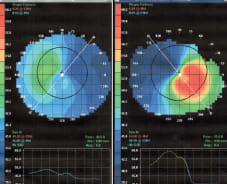
Figure 7. Lateral keratoconus—temporal (I/S values of OD 0.16D and OS 4.33D).
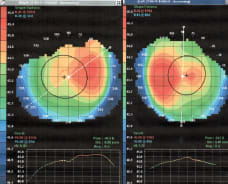
Figure 8. Lateral keratoconus—nasal (I/S values of -1.15D OD and -0.46D OS).
The CW sub-group is small because we tested them to prove or disprove supposed ectasia. Were we to begin mapping the corneae of our contact lens-wearing population as a whole, the percentage would leap. I am certain that many of our successful contact lens wearers, especially those who wear contact lenses designed with aspheric back surfaces, would exhibit CW should their corneae be mapped.
To our ophthalmology clinic, corneal topography is an aid in diagnosis and treatment. To our contact lens clinic, the mappings guide us in choosing and developing contact lens designs appropriate to the specific surface shapes of our patients’ eyes: high regular astigmatism should be fit with back-surface toric (including bitoric) lenses; moderate keratoconus should do well with any of the proprietary KC designs; and advanced KC, PMD, post-trauma corneae, and many post-keratoplasty will inevitably succeed to a greater degree with less complications using scleral lenses. CLS
Acknowledgement
As always, I must express my respect and thanks to my patients for choosing me to help them confront the visual adversities invoked by their corneal ectasias.
For references, please visit www.clspectrum.com/references. asp and click on document #204.



