FITTING MULTIFOCALS
Successful Strategies to Increase Multifocal Fits
Implementing these seven factors can lead to increased multifocal fitting-and enthusiastic patients.

| Dr. Wan currently owns and operates two optometric practices in San Diego, Calif. He does specialty contact lens fittings as well as primary eye care. He has received lecture or authorship honoraria from CooperVision. |
By Keith Wan, OD
Although there are an increasing number of presbyopes in my practice, I was initially reluctant to fit soft multifocal contact lenses. I heard colleagues cite challenges with fitting multifocals such as the excessive fitting time, lack of compensation for the additional chair time, and visual compromise. However, once I decided to fit multifocals, I discovered that all of these concerns were unfounded.
In 2011, my office was one of 15 offices (10 in the United States and five in Europe) that took part in a study conducted by CooperVision to determine whether adopting recommended fitting strategies would increase the number of successful soft multifocal fits. This study was based on previous research in which highly successful multifocal fitters were interviewed to identify the key factors that promoted an increase in the number of successful multifocal fits.
All of the offices that took part in this study had their soft multifocal fittings tracked for three months. At the end of the study period, the key multifocal success factors were discussed with each office. The success factors were then implemented and soft multifocal lens fittings tracked for another three months. At the end of this period, a statistical analysis was conducted to determine whether there was a measurable increase in the number of multifocal fits (Figure 1). The results revealed a statistically significant increase in the number of successful fits in Europe (50 percent) and in the United States (17 percent).
Success Factors
The seven multifocal success factors that were identified are:
1. Train your staff to be knowledgeable about multifocals. This quality was universal in each of the offices that successfully fit multifocals. All staff members should be trained to answer questions regarding multifocal contact lenses at each possible patient touch point—the reception desk, pretesting, optical dispensing, or on the phone. Your staff can be an effective and proactive advocate for multifocal lenses. The staff should also be trained to recognize potential multifocal candidates and to share that information with the practitioner.
2. Determine eye dominance during the refraction. Many of the successful practitioners determine eye dominance while the patient is looking through the phoropter. While viewing the eye chart after the subjective exam is completed, the practitioner will place the retinoscopy lens in front of one eye and then switch it to the opposite eye, and ask the patient which way feels more visually comfortable. The nondominant eye is the eye that feels more comfortable when looking through the retinoscopy lens. Most patients ask why that test is being conducted. The practitioner can explain that they are candidates for multifocals and should they be interested in trying them, eye dominance needs to be determined. This creates an opportunity for a discussion regarding multifocals.
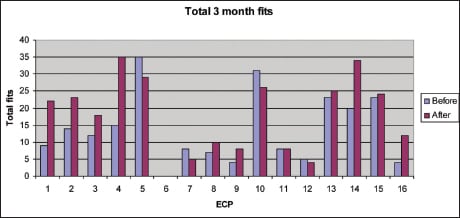
Figure 1. A comparison of multifocal lens fits before and after focal fitting strategies were implemented
3. Use a cell phone to test functional near vision. After fitting patients with diagnostic lenses, most practitioners determine the best near vision by having patients read a near point card. Patients will usually look at the smallest line first and may not be able to see it clearly. This can cause patients to be disappointed and to have a negative first impression. All of the successful fitters used a patient’s cell phone to initially assess near vision, because most of a patient’s near tasks revolve around a cell phone. If the patient can view his phone, there is immediate positive reinforcement and added enthusiasm for the patient.
Many practitioners resist fitting multifocals because they believe that patients will experience poor visual acuity. It is important to remember that you can’t judge fit success based on an acuity chart. An interesting clinical study by Woods et al (2009) compared multifocals, monovision, and distance-only corrections while engaged in various tasks. Although monovision was slightly more preferable to multifocals when measuring low-contrast acuity objectively, multifocals were preferred subjectively for 15 out of 16 dynamic tasks. The conclusion of the study reinforces that it is not wise to predict success based solely on an acuity chart measurement.
4. Set expectations frequently. It is essential to give patients a true understanding of what they can expect visually with multifocals and to frequently reinforce those expectations. Always under-promise but try to over-deliver. Patients should be aware that multifocals will be sufficient for most activities, but there may be occasions when glasses or two distance contact lenses may be preferable to the multifocals.
5. Achieve the final prescription in one to two visits. One of the main reasons why practitioners hesitate to fit multifocals is the perception that the fitting process is very time consuming. If you are changing lenses five or six times, it is time consuming. Successful practitioners realize that if you need to change the prescription for a particular design more than two times, that design most likely will not work. It is essential to be able to understand why some lenses will be better for some patients than for others. Some factors to consider are pupil size, lens centration, and the differences between center-near and centerdistance designs.
Pupil size is critical to the performance of a simultaneous vision lens. Because the pupil size may decrease with age, this becomes more problematic with presbyopic patients. Assess pupil size prior to fitting lenses and determine which design may be most appropriate. If the pupil is fairly small, using a centernear design in one eye and a center-distance design in the opposite eye may be warranted.
Lens centration is also critical to achieving acceptable vision. Practitioners may use a topographer to determine the lens center and the visual axis to establish whether they are in close enough proximity to provide adequate vision.
It is important to remember that a center-near design has an aspheric anterior surface and a centerdistance design has an aspheric posterior surface. This will create a difference in the amount of spherical aberration that is either induced or reduced. Using an aberrometer without a lens in place and then with a contact lens applied will indicate whether a particular design improves vision or makes it worse. This will also help in deciding whether a center-near or center-distance design is more beneficial.
6. Always dispense the optimal prescription for the first diagnostic pair of lenses. Successful fitters agree that it is imperative to dispense a pair of diagnostic lenses that provide the best possible vision. If a patient does not feel that the vision is clear enough, particularly at distance, he will not wear the lenses during the adaptation period. The result is a patient who is not wearing the diagnostic lenses to the follow-up visit and, unless better vision can be provided, ultimately gives up on multifocals. If practitioners take the time to provide the best possible prescription on the first visit, subsequent visits should only necessitate fine tuning.
Advise patients that the adaptation period will be longer than the 10-minute to 15-minute equilibration period that follows the initial application of the diagnostic lenses. Adaptation is a cortical process whereby the brain learns to selectively choose the clearer image depending on the distance at which an object is viewed. Make sure that the patient under-stands it will take one to two weeks for the brain to adapt to this new means of visual correction.
7. Proactively recommend multifocal contact lenses. This is my personal success factor. Patients want your recommendation. As long as it is in their best interest, they will usually follow that recommendation. Whether it is multifocals, daily disposables, or torics, proactively recommending any lens type will result in an increased number of patients wearing that type of lens.
More Multifocals, More Patients
There are additional benefits to a practice beyond just an increase in the number of multifocal fits. Multifocals are a great practice builder. Invariably, whenever I successfully fit a patient with multifocals, that patient is enthusiastic and refers a friend, family member, or co-worker who could also benefit from a multifocal. This increases the number of patients coming into my practice as well as practice revenue.
I have found that by implementing these seven key strategies, multifocal lenses have become easy to fit and provide distinct advantages over monovision. In particular, multifocals provide better stereopsis and intermediate vision. If you have been reluctant to fit multifocal lenses, I encourage you to implement these key strategies. Not only can you be a successful multifocal fitter, multifocal lenses can be a great practice builder for you, too. CLS
For references, please visit www.clspectrum.com/references.asp and click on document #204.



