TORIC GP LENSES
A Toric GP Primer
A comprehensive examination of optimal toric GP candidates, contact lens design, and modalities.
By Annie Chang, OD, FAAO, & Dawn Lam, BSc, MSc, OD, FAAO
|
|
Dr. Lam is an associate professor who teaches cornea and contact lenses at the Southern California College of Optometry at Marshall B. Ketchum University. |
|
|
Dr. Chang is an assistant professor at the Southern California College of Optometry at Marshall B. Ketchum University. You can reach her at achang@ketchum.edu. |
Toric GP contact lens prescribing can be a valuable asset for an eyecare practitioner's office. GP lenses generally provide the best corrective option for patients who have high astigmatism and high ametropia. There are an estimated 37 million contact lens wearers in the United States; 22 percent are wearing soft toric lenses, while toric GP lenses make up less than 3 percent of the market (Nichols, 2012). In recent years, the availability of expanded soft toric lens parameters has made it possible for more patients to be prescribed this modality.
Still, patients who have high amounts of astigmatism and ametropia are generally excluded from wearing soft toric lenses. These are the very patients who would benefit most from contact lens wear. In this article, we discuss ideal toric GP patients, designing toric GP lenses, and the different toric GP lens designs available to optimize patient success.
Ideal Candidates
GP lenses often provide patients with superior vision compared to soft lenses and spectacles. Unfortunately, GP lenses have a reputation for being uncomfortable for patients to wear and challenging for practitioners to design. Achieving a successful GP lens fit means selecting appropriate patients.
Ideal GP wearers are patients who plan to wear their contact lenses on an everyday basis. GP lenses require adaptation; thus, part-time wearers are better suited for soft contact lens wear. Other considerations include patients' vocational and avocational needs. Patients who work or enjoy avocations in dusty or windy environments may not be comfortable wearing GP lenses.
Once you have determined that there are no contraindications to GP wear, ideal toric GP candidates are those who have regular corneal toricity of at least 2.00D. When there is less than 2.00D of corneal astigmatism, spherical GPs should be your first option. For these patients, a spherical GP can mask the majority of corneal astigmatism and still maintain an adequate fitting relationship.
Patients who have more than 2.00D of corneal toricity should generally be fitted with back-surface toric GP lens designs, which tend to provide enhanced lens centration, stability, and comfort. Surveyed eyecare practitioners agreed that back-surface toric GP lenses should be initiated for corneal toricities starting between 2.00D and 2.75D (Blackmore et al, 2006).
Spherical GP lenses on toric corneas >2.50D tend to not center well, and although patients can attain good vision, they tend to result in decreased lens comfort. A spherical GP lens on a with-the-rule (WTR) cornea may not center, but rather position superiorly or inferiorly on the cornea. On an against-the-rule (ATR) cornea, it may position nasally or temporally. Decentered GP lenses may also cause peripheral corneal desiccation. In addition, a superior lens position can result in corneal molding and lead to end-of-day spectacle blur. Toric GP lenses are more comfortable for such patients because the toric back surface better contours the toric shape of their corneas. Toric peripheral curves generally result in decreased lens movement, and they minimize lid interaction with the lens edge.
Patients who have significant refractive astigmatism and very little corneal toricity are not ideal back-surface toric GP candidates. Their astigmatism is primarily lenticular, and thus front-surface toric GP lenses or soft toric contact lenses are more suitable for these patients.
The magnitude of patients' ametropia should also be considered. There are limited standard silicone hydrogel (SiHy) toric lens designs for hyperopia greater than +8.00D and myopia greater than -10.00D. Typically, these SiHy soft toric lenses currently correct only up to -2.25D cylinder. Soft toric lenses provide optimal vision when the lenses are rotationally stable on the eye. This can be problematic for patients who have significant amounts of astigmatism, as even small amounts of axis misalignment or lens rotation may create visual blur. Every 10 degrees of lens misalignment will result in one-third of the correcting cylinder power manifesting in the sphero-cylindrical overrefraction (OR). A lens with -2.25D of cylinder power that rotates 10 degrees off axis will induce -0.75D of unwanted residual cylinder power (Snyder, 1989).
Fitting
Toric GP lens fitting can be performed empirically or by utilizing a diagnostic fitting set. Empirical fitting requires no additional chair time provided keratometry readings are part of your routine comprehensive examination. Initial lenses are designed using keratometry and manifest refraction data. Patients' initial GP lens experiences will be better and more comfortable with empirical fitting as the contact lens powers and base curve radii closely match patients' refractive error and corneal curvature.
An example of an empirical fitting guide is the Mandell-Moore Guide (www.gpli.info/mandell-moore/). This fitting guide designs a bitoric lens utilizing patients' keratometry and spectacle refraction findings. The Mandell-Moore Guide is convenient because there are no calculations to memorize, which makes this worksheet user-friendly. One study tested the Mandell-Moore fitting guide by designing lenses for 33 successful bitoric lens-wearing patients and found that when lens parameters were compared, no significant differences were detected (Pitts et al, 2001). The Mandell-Moore Guide incorporates a suggested "fit factor." This incorporates a slightly flatter than on-K fitting relationship and slightly undercorrects the amount of corneal toricity. This helps to achieve a fit that optimizes tear exchange, yet allows the back surface of the GP contact lens to align with the cornea for rotational stability (Mandell and Moore, 1988).
Another reference for empirical fitting is the GPLI Toric and Spherical Lens Calculator (www.gpli.info/lens-calculator/). This calculator shows tear film calculations dynamically (other parameters, such as overall diameter and any rotational considerations, are provided as well). When ordering lenses empirically, properly calibrated keratometers and precise manifest refractions are of utmost importance. This can save you time and money on future re-orders and provide your patients with exceptional initial GP experiences. If a keratometer is not available in your office, simulated keratometry values from topography imaging can also be utilized.
A second method of toric GP lens fitting uses a diagnostic fitting set at the initial examination. This allows practitioners to assess not only lens-to-cornea fitting relationships, but also to evaluate any lid interactions affecting GP lens fits. Although diagnostic fitting requires extra chair time, it allows practitioners to determine potential visual acuity through GP lenses and provides a dynamic view of lenses on the eye.
To perform a diagnostic fit in-office for a spherical or a toric cornea, a simple spherical GP fitting set is required. It is recommended that the spherical fitting set be organized by base curve radius for ease of use during lens fitting. A spherical GP diagnostic fitting is particularly useful when there is uncertainty about ordering spherical or bitoric GP lenses for patients who have low-to-moderate (1.50D to 2.50D) toric corneas. Placing a spherical GP lens on the eye prior to ordering a lens can confirm whether a spherical lens provides satisfactory fit and vision.
A bitoric GP fitting set can be useful when diagnostically fitting a toric cornea, but it is certainly not required. The advantage of using a bitoric fitting set is its capacity for a more accurate assessment of lensto-cornea fitting relationships on moderate-to-high (>2.50D) toric corneas. If ordering a bitoric fitting set, incorporating lenses with two different amounts of base curve toricity can be helpful—for example, having one set of lenses that has a 2.50D toric base curve and another set that has 4.00D. These two base curve toricity amounts will allow you to successfully fit the range of most toric corneas that you will encounter in practice. In addition, incorporating different tints and powers on the lenses can allow for quick identification and prevent mix-ups (Tables 1 and 2).
There are various methods used in selecting the initial base curve radii for diagnostic lens fitting. Base curves can be based on the amount of corneal toricity, average corneal curvature, steep K, or flat K. Regardless of the fitting philosophy, the ultimate decision on lens design is based upon the fluorescein pattern. We recommend using an empirical fitting guide so that the average base curve radius of the lens is equal to the average keratometry value minus 0.75D.
If the initial lens choice is a spherical lens, the following example illustrates our point. For keratometry values of 43.00 × 40.00 @ 180, the initial base curve selection would be the Average K - 0.75D = 41.50D - 0.75D = 40.75D.
| TABLE 1 Base Curve Toricity 2.50D |
|||||
|---|---|---|---|---|---|
| BCs* (D) | Powers (D) | OAD/OZD (mm) | Flat SCr (mm) | TCr/TCw (mm) | Tint |
| 41.50/39.00 | -0.50/+ 2.00 | 9.2/7.6 | 9.35 | 12.00/0.2 | Brown #1 |
| 42.00/39.50 | -1.50/+ 1.00 | 9.2/7.6 | 9.24 | 12.00/0.2 | Blue #1 |
| 42.50/40.00 | -2.50/Plano | 9.2/7.6 | 9.14 | 12.00/0.2 | Blue #1 |
| 43.00/40.50 | -3.00/-0.50 | 9.2/7.6 | 9.03 | 12.00/0.2 | Brown #1 |
| 43.50/41.00 | -2.50/Plano | 9.2/7.6 | 8.93 | 12.00/0.2 | Grey #1 |
| 44.00/41.50 | -3.50/-1.00 | 9.2/7.6 | 8.83 | 12.00/0.2 | Green #1 |
| 44.50/42.00 | -4.00/-1.50 | 9.2/7.6 | 8.74 | 12.00/0.2 | Blue #1 |
| 45.00/42.50 | -3.00/-0.50 | 9.2/7.6 | 8.64 | 12.00/0.2 | Green #1 |
| 45.50/43.00 | -4.00/-1.50 | 9.2/7.6 | 8.55 | 12.00/0.2 | Grey #1 |
| 46.00/43.50 | -3.50/-1.00 | 9.2/7.6 | 8.46 | 12.00/0.2 | Brown #1 |
| 46.50/44.00 | -4.50/-2.00 | 9.2/7.6 | 8.37 | 12.00/0.2 | Green #1 |
| 47.00/44.50 | -5.00/-2.50 | 9.2/7.6 | 8.28 | 12.00/0.2 | Grey #1 |
|
* Heading abbreviations as follows — BCs: Base Curves; OAD: Overall Diameter; OZD: Optical Zone Diameter; SCr: Secondary Curve Radius; TCr: Tertiary Curve Radius; TCw: Tertiary Curve Width Note: Fabricate the secondary curve to be 2.50D toric for all of the lenses. This will result in a round optical zone. TABLE COURTESY OF DR. TIMOTHY EDRINGTON | |||||
| TABLE 2 Base Curve Toricity 4.00D |
|||||
|---|---|---|---|---|---|
| BCs* (D) | Powers (D) | OAD/OZD (mm) | Flat SCr (mm) | TCr/TCw (mm) | Tint |
| 42.50/38.50 | -1.00/+3.00 | 9.2/7.6 | 9.47 | 12.00/0.2 | Brown #1 |
| 43.00/39.00 | -2.00/+2.00 | 9.2/7.6 | 9.35 | 12.00/0.2 | Blue #1 |
| 43.50/39.50 | -4.00/Plano | 9.2/7.6 | 9.24 | 12.00/0.2 | Blue #1 |
| 44.00/40.00 | -4.50/-0.50 | 9.2/7.6 | 9.14 | 12.00/0.2 | Brown #1 |
| 44.50/40.50 | -4.00/Plano | 9.2/7.6 | 9.03 | 12.00/0.2 | Grey #1 |
| 45.00/41.00 | -5.00/-1.00 | 9.2/7.6 | 8.93 | 12.00/0.2 | Green #1 |
| 45.50/41.50 | -5.50/-1.50 | 9.2/7.6 | 8.83 | 12.00/0.2 | Blue #1 |
| 46.00/42.00 | -4.50/-0.50 | 9.2/7.6 | 8.74 | 12.00/0.2 | Green #1 |
| 46.50/42.50 | -5.50/-1.50 | 9.2/7.6 | 8.64 | 12.00/0.2 | Grey #1 |
| 47.00/43.00 | -5.00/-1.00 | 9.2/7.6 | 8.55 | 12.00/0.2 | Brown #1 |
| 47.50/43.50 | -6.00/-2.00 | 9.2/7.6 | 8.46 | 12.00/0.2 | Green #1 |
| 48.00/44.00 | -6.50/-2.50 | 9.2/7.6 | 8.37 | 12.00/0.2 | Grey #1 |
|
*Heading abbreviations as follows — BCs: Base Curves; OAD: Overall Diameter; OZD: Optical Zone Diameter; SCr: Secondary Curve Radius; TCr: Tertiary Curve Radius; TCw: Tertiary Curve Width Note: Fabricate the secondary curve to be 4.00D toric for all of the lenses. This will result in a round optical zone. TABLE COURTESY OF DR. TIMOTHY EDRINGTON | |||||
Diagnostic fitting allows practitioners to assess the lens-to-cornea relationship as well as lid interactions.
If the initial lens choice is a bitoric lens, we recommend using the Mandell-Moore fitting guide. For the same keratometry values as above, Mandell-Moore recommends an initial lens with base curves of 42.25D/39.75D.
Fluorescein Patterns
Accurately assessing fluorescein patterns is essential for all GP contact lens fittings. Evaluating each fluorescein pattern in a systematic fashion can streamline the process and allow accurate analysis for lens changes if necessary. The major components to consider are the apical fitting relationship, corneal toricity, peripheral clearance, lens position, and lens movement. The following describes fluorescein patterns for toric corneas only.
Apical Fitting Relationship This is the central lens-to-cornea fitting relationship, which indicates whether the lens base curve radius is too flat or too steep relative to patients' corneal curvature. A steep-fitting spherical lens on a WTR cornea will result in a vertical column of fluorescein, flanked by two midperipheral small areas of bearing (apical clearance) (Figure 1). If a lens is too flat on a WTR cornea, there will be a horizontal area of central bearing (apical touch) (Figure 2). On a WTR cornea, the dark band will begin to appear longer (horizontally) as the lens becomes increasingly steeper, eventually extending from one end of the optical zone to the other when the lens is "aligned" (Figure 3).

Figure 1. A steep-fitting spherical lens on a WTR cornea.
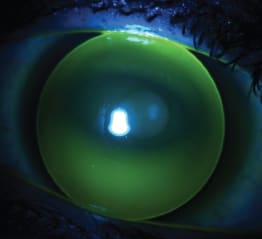
Figure 2. A spherical GP lens that is too flat on a WTR cornea.

Figure 3. A WTR cornea with an "aligned" lens, showing the dark band that extends from one end of the optical zone to the other.
A bracketing method is the best technique to determine an "alignment" fitting relationship in which the base curve radius best contours the cornea. If the initial lens exhibits apical touch, then steepen the base curve radius until the flattest base curve radius that reveals an apical clearance pattern is achieved. The "alignment" base curve radius will be approximately 0.25D flatter.
Toricity The keratometry readings will provide valuable information on the appearance of the fluorescein pattern. A WTR alignment fluorescein pattern will be most evident when a spherical GP lens is on a WTR cornea. This will appear as a horizontal dark band across the center of the lens and will resemble an oval or football shape. The more oval the pattern appears, the more toric the cornea. In addition, there may be an excessive amount of edge lift at the 12 o'clock and 6 o'clock positions of the lens, which will dictate whether a toric lens design should be prescribed. As the amount of toricity increases, the horizontal dark band will transition into a thinner, cigarshaped appearance (Figure 4). As a general rule of thumb for WTR corneas, the shorter the dark band (vertically), the greater the amount of corneal toricity. A spherical lens on an ATR cornea results in a dark vertical band across the center of the lens (Figure 5). The amount of toricity needs to be quantified to determine the amount of base curve toricity in the lens.
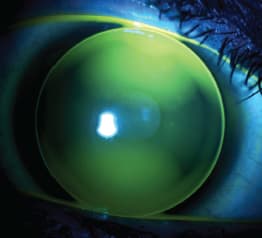
Figure 4. A fluorescein pattern with increased toricity, producing a thinner horizontal band.
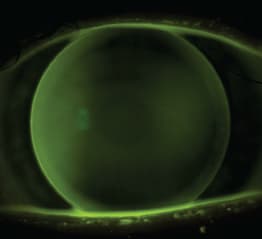
Figure 5. A spherical lens on an ATR cornea with a characteristic dark vertical band across the center of the lens.
Peripheral Clearance The amount of fluorescein at the edge of the lens indicates the peripheral clearance or edge lift. Obtaining an adequate peripheral clearance is important to enhance tear exchange beneath a GP lens. A thin, or minimum, amount of peripheral clearance can eventually lead to poor tear exchange and possible lens sealoff. Excessive peripheral clearance can cause excessive lens movement as well as create interaction with the lid, resulting in discomfort. Spherical lenses on a highly WTR cornea will present with an uneven peripheral clearance. Excessive peripheral clearance will be observed at the 12 o'clock and 6 o'clock positions, and minimum peripheral clearance will be seen at the 3 o'clock and 9 o'clock positions. In such cases, toric GPs are recommended.
Lens Position and Lens Movement An accurate evaluation of the fluorescein pattern requires appropriate centration of the lens on the eye. This may require manipulating a patient's eyelid to physically center the lens or evaluating the lens fit after a blink. Observing the lens position and movement in its natural state can also provide useful information. For example, lenses that habitually position inferiorly can create blur because patients are not looking through the optical zone, and lenses that exhibit excessive movement with each blink can cause discomfort.
Over-Refraction
When performing a diagnostic fitting, use an OR to determine the final contact lens power. Most often, simply performing a spherical OR through spherical GP diagnostic contact lenses will allow patients to read at their threshold visual acuity. If patients' vision is still reduced after a spherical OR, a sphero-cylindrical OR will be necessary. If a small amount of residual astigmatism is present in the initial OR (<0.75DC), convert the result to a spherical equivalent. A spherical GP lens will neutralize most of the corneal astigmatism, and little-to-no residual astigmatism is expected. If a large amount of residual astigmatism is present in the OR, then the residual astigmatism is either lenticular or is due to GP lens flexure. Performing over-keratometry or over-topography can identify the cause. If the over-keratometry values are not spherical, the spherical GP lens is flexing on the cornea, and increasing the center thickness of the GP lens may remedy this problem. If the keratometry values are spherical, then the residual astigmatism is lenticular, and this will need to be incorporated into the final lens power.
If the fluorescein pattern indicates that a toric back-surface GP lens is needed, add half of the observed amount of toricity to the steep meridian and subtract the other half from the flat meridian. Then place the OR on an optical cross to determine the final contact lens powers in each meridian. If the cornea is spherical or mildly toric (<1.00D of toricity) and there is significant lenticular astigmatism, consider a front-surface toric GP or a soft toric contact lens.
Consider the following example. For an initial diagnostic lens selection of 40.75D/-1.00DS, the fluorescein pattern exhibited apical touch by 0.50D/3.00D WTR toricity. The OR was -2.00 -0.50 × 180 (20/15) (Figure 6). The final lens base curve and power would be:
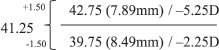

Figure 6. Utilizing a diagnostic GP spherical lens and over-refraction data to determine bitoric base curve radii and powers.
The ABCs of Toric GPs
There are three types of back-surface toric GP lenses.
Spherical Power Effect (SPE) Bitoric Design A SPE bitoric design lens has the same difference in the base curves (in diopters) and powers. In the following example, the difference in both base curves and powers is 3.00D.
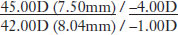
This type of bitoric GP lens enhances the fit on a toric cornea, but maintains an overall power equivalent to a spherical GP lens. The advantage of this design is that it allows the lens to rotate on the eye without inducing any residual astigmatism.
Cylinder Power Effect (CPE) Bitoric Design The following is an example of a CPE bitoric design lens:
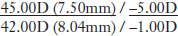
It has an unequal difference in the base curve radii (in diopters) and powers. This type of bitoric GP lens has a toric back surface, which improves the lens-tocornea fitting relationship by contouring a patient's toric cornea. The design also corrects for residual lenticular astigmatism and therefore requires good rotational stability. Any rotation of the lens on the eye could result in blurring of vision, although the toric back surfaces typically align with the respective toric corneal meridians.
Base Curve Toric (BCT) A BCT design lens has a difference in the powers that is approximately 1.5 times the difference in the base curves (in diopters).

This type of toric GP lens has a toric back surface and a spherical front surface. It allows for in-house modification on the front surface, such as polishing or adding minus.
Problem-Solving for Toric GP Lenses
Poor Vision If patients' vision is reduced through a toric GP lens, performing a sphero-cylindrical OR can determine whether additional spherical or cylinder power is necessary. If spherical power alone improves the patient's vision, add the spherical power to each meridian of the lens. If cylinder power improves the vision, use optical crosses to add the cylinder power to the appropriate meridian.
Patients may experience blurred vision from a poorly wetting GP lens. One way to combat non-wetting lenses is to mechanically rub them with a GP cleaning solution and soak them in GP conditioner. An alternative remedy is to order GP contact lenses with plasma treatment, and they will be shipped pre-soaked.
Blurred vision may also be due to lens rotation. If the lens is a CPE bitoric or a BCT, oneye lens rotation may cause visual blur. An insufficient amount of base curve toricity can cause the back-surface GP lens to rotate. Increasing base curve toricity will allow the lens to better "lock" into place on the cornea.
Poor Fit Ideally, a toric GP lens on a toric cornea will exhibit an alignment fluorescein pattern similar to a spherical lens on a spherical cornea. If distinct WTR bands or ATR patterns are apparent upon fluorescein evaluation, increasing the amount of toricity in GP lenses will generally provide better alignment fitting relationships. If a distinct circular area of central bearing is present and accompanied by excessive movement, steepening the base curve radius in both meridians can achieve an alignment fitting relationship.
Concluding Thoughts
Toric GP contact lenses are a useful option in an eyecare practitioner's contact lens armamentarium. There is a sector of astigmatic patients for whom these lens designs provide the best visual correction and optimize patients' corneal health. CLS
For references, please visit www.clspectrum.com/references.asp and click on document #217.





