FITTING CORNEAL ECTASIA
Contact Lens Options for Managing Keratoconus and Keratectasias
Advancements in designs and materials have brought many contact lens options for managing keratoconus.
By S. Barry Eiden, OD, FAAO; Clark Chang, OD, MS, FAAO; Robert Davis, OD, FAAO; & Shana Brafman, OD
|
Dr. Eiden is president and medical director of North Suburban Vision Consultants, president and medical director of the National Keratoconus Institute, and co-founder of EyeVis Eye and Vision Research Institute. He is an adjunct faculty member at The University of Illinois Medical Center as well as at the Indiana, Illinois, Salus, and PCO Colleges of Optometry. Dr. Eiden is a consultant or advisor to CooperVision, Alcon, B+L, Visionary Optics, Alden Optical, Oculus, Diopsys, Paragon Vision Sciences, and SpecialEyes. |
|
Dr. Chang is the director of the Contact Lens Division at The Cornea and Laser Eye Institute-Hersh Vision Group at Teaneck, N.J. He is president of New Jersey Academy of Optometry, he serves as an adjunct faculty member for Pennsylvania College of Optometry at Salus University, and is an advisory member at National Keratoconus Institute. He has received travel funding from B+L and Oculus and lecture or authorship honoraria from Alden Optical. |
|
Dr. Davis is a cofounder of EyeVis Eye and Research Institute and practices in Oak Lawn, Illinois. He is an adjunct faculty member at Southern California College of Optometry, Illinois College of Optometry, Pennsylvania College of Optometry at Salus University, and University of Alabama at Birmingham. Dr. Davis is a Diplomate in the Cornea, Contact Lenses and Refractive Technologies section of the American Academy of Optometry as well as an inductee in the National Academies of Practice in Optometry. He has received research funds from SynergEyes, CooperVision, and B+L and has a proprietary interest in SpecialEyes, Alternative Vision Solutions, and in the Recess Pillow Lens System. |
|
Dr. Brafman is co-director of Contact Lens Specialty Services at North Suburban Vision Consultants, Ltd. and is an assistant clinical professor at the Illinois College of Optometry and Illinois Eye Institute. |
Keratoconus is a thinning disorder of the cornea that leads to conical ectasia (Figure 1). The thinning and conical protrusion of the cornea in keratoconus typically results in irregular astigmatism, increased high-order aberrations, visual distortion, and visual impairment. The frequency of keratoconus is estimated to be approximately 1 in 2,000 to as high as 1 in 500 (Gordon-Shaag et al, 2012); presumably, incorporation of more sensitive and advanced diagnostic technologies such as corneal topography and tomography may prove the prevalence to be even higher. Other forms of corneal thinning or keratectasia, such as iatrogenic keratectasia following refractive surgery, can also create clinical presentations that appear quite similar to keratoconus and are often managed in similar ways.

Figure 1. Keratoconic cornea with thinning and conical protrusion.
Contact lenses are the primary modality for vision correction in managing keratoconus. They can "mask" the irregularity of the anterior corneal surface, and as such they provide clearer vision with less distortion and reduced high-order aberrations. Traditionally, rigid corneal contact lenses have been the mainstay in treating keratoconus based on their ability to create a regular anterior optical surface; however, more contemporary contact lens modalities have been developed that allow for vision correction.
In this article, we will review the array of contact lens and other treatment options available for keratoconus management and outline the advantages and disadvantages of each. We will discuss as well the most appropriate indications for their utilization.
Using Spectacles in Managing Keratoconus
The role of spectacles in managing keratoconus is often underestimated. Spectacles can provide excellent vision correction in keratoconus cases in which the conical protrusion and secondary anterior corneal surface distortion does not affect the visual axis (Figure 2). Topography maps will often provide an indication of vision quality expectations with refraction and subsequently with spectacle lenses.

Figure 2. Corneal tomography demonstrating regularity of astigmatism within the optic zone, thus suggesting adequate spectacle lens acuity. This was confirmed by manifest refraction resulting in best-corrected acuity of 20/25+.
However, even in cases in which there is no significant visual impairment and in which spectacle lenses can provide adequate vision quality, there are a number of other issues to consider that make the use of spectacle lenses challenging in managing keratoconus. Patients must tolerate high degrees of astigmatic correction and anisometropia in spectacles as well as frequent prescriptive changes that are common in progressive keratoconus.
Spectacle lenses can be successfully used in conjunction with contact lenses in keratoconus management to address issues such as residual astigmatism not corrected by the contact lenses as well as presbyopia. Finally, promising new technologies in spectacle lens correction may directly address high-order aberrations common to keratoconus.
General Concerns Regarding Contact Lenses for Keratoconus
Contact lenses primarily address the visual challenges of keratoconus by masking the anterior corneal surface irregularity and creating a smoother, more regular anterior optical surface. There are typically three key elements to success in all areas of contact lens treatment: 1) providing appropriate vision correction; 2) providing acceptable comfort during lens wear; and 3) providing an appropriate ocular physiological response to lens wear.
Specific to keratoconus, we always want to avoid mechanical pressure on the apex of the cornea, avoid hypoxic stress to the cornea, provide maximum comfort through contact lens fitting design, and optimize vision through contact lens optical design (addressing not only keratoconic visual distortion but also residual astigmatism, presbyopia, and other influences on visual performance).
Soft Contact Lens Utilization in Keratoconus
Soft contact lenses provide advantages over other lens modalities in keratoconus management that include initial and ongoing comfort, relative centration of the lens optics over the visual axis, and protection of the ocular surface. Potential disadvantages of soft lenses for keratoconus include relative visual compromise due to the draping effect over the irregular corneal surface, increased risk of deposition, microbial contamination/infection, and dehydration.
Standard soft contact lenses (either in disposable/frequent replacement or for conventional annual replacement modalities) can be considered in cases in which corneal distortion is limited and best-corrected manifest refraction acuity is fairly good (typically 20/25 or better). Typically, toric standard soft contact lenses are needed for keratoconus; however, keep in mind that the final lens power parameters, including astigmatic power and axis, often can't be predicted from manifest refraction outcomes due to draping effects over the irregular corneal surface. Sphero-cylindrical over-refractions are very valuable in these cases.
Consider custom specialty keratoconic soft contact lenses in cases of more advanced corneal irregularity. Such designs typically utilize increased thickness in the optical portion of the lens to mask corneal irregularity (Figures 3 and 4). As the degree of corneal irregularity increases, you can increase the thickness of the optical zone accordingly. Thickness values in these lenses typically range from 0.25mm to up to 0.60mm, with an average of approximately 0.40mm. It is important to note that this thickness is limited to the central optical zone (typically the central 8mm to 9mm).

Figure 3. Custom soft contact lens for keratoconus demonstrating a thick optic section for masking corneal irregularity and thin midperiphery and periphery to optimize physiological response.

Figure 4a. Photokeratoscopy image of distorted cornea in keratoconus.

Figure 4b. Same eye with a custom keratoconic soft lens demonstrating a significant reduction of surface distortion.
The midperiphery and far peripheries of these soft keratoconus contact lenses are thinned out by lenticulation. This helps address oxygen transmission concerns because the portion of the lens that is excessively thick does not lie over the limbal stem cells in the peripheral cornea. Additionally, these lenses typically move more on the eye compared to standard soft contact lenses. We typically strive for about 0.75mm of lens movement when evaluated in primary gaze. Finally, a number of custom specialty keratoconic contact lenses are now available in higher-Dk silicone hydrogel materials.
A significant advantage of using custom keratoconic soft lens designs is the ability to incorporate toric correction to address residual astigmatism, which is quite common in keratoconus contact lens fitting. There are numerous manufacturers of these lenses (Table 1). Usually working with two or three designs at most will allow you to fit a significant percentage of patients successfully.
| TABLE 1 |
|---|
|
Custom Keratoconus Soft Lens Designs* • HydroKone (Visionary Optics) • NovaKone (Alden Optical) • Kerasoft IC (distributed by B+L) • Soft K (Accu Lens, Advanced Vision Technologies, & Strategic Lens Innovations Corp. [SLIC]) • Continental Kone (Continental Soft Lens) • Keratoconus lens (Gelflex) • Soflex (Orion Vision Group) • Ocu-Flex K (Ocu-Ease, Optech) • UCL-55 (United Contact Lens) • Flexlens Keratoconus (X-Cel) * This represents only a partial list of available soft contact lens designs for keratoconus. |
Corneal GP Lenses
As stated previously, the mainstay of contact lens fitting for keratoconus has been and continues to be corneal GP contact lenses. This modality provides the obvious advantage of excellent visual outcomes when properly fit on keratoconic eyes. However, managing keratoconus with corneal GPs can present challenges, especially in more advanced cases, with ongoing comfort, potential apical compromises, and stability of lens positioning.
The Collaborative Longitudinal Evaluation of Keratoconus (CLEK) study found that 87 percent of patients wearing rigid lenses at the entry point in the study were fit flat with apical bearing (Zadnik et al, 2005). At the end of the eight-year study, 31 percent of subjects who wore apical-bearing contact lenses developed corneal scarring, while only 9 percent of subjects wearing lenses with apical clearance developed corneal scarring. This and other data suggest that one of our goals in fitting corneal GP lenses in keratoconus should be to "clear the cone," or fit without bearing on the apex of the cone if at all possible. In cases in which this is not possible, we should accept only light touch, also termed "feather touch," of the lens at the apex of the cone.
To maximize lens-wearing comfort, we want to also try to match the midperiphery of the cornea and provide appropriate peripheral lens edge clearance. Keratoconic corneas are often quite asymmetric, especially along the vertical meridian. Asymmetric intermediate and peripheral curve systems can help better align these corneas and allow for more consistent edge clearance.
The appropriate corneal GP lens overall diameter is typically based upon the anterior corneal surface topography and elevation or on corneal tomography data (Figure 5). For smaller and more central cones, otherwise known as "nipple cones" (Figure 5a) we tend to fit small-diameter, multi-curve lenses. These lenses have overall diameters below 9.0mm with optical zone diameters of 7.0mm or less. Choose an initial base curve radius for diagnostic lens fitting that is between the steep and mid-keratometric (mid-K) or simulated keratometry values. Proprietary lens designs such as Rose K2 (Menicon, Blanchard, and various other distributors), Dyna Cone (Lens Dynamics), and McGuire cone (many laboratories) are examples of this lens type. Fitting small-diameter GP lenses requires appropriate centration over the visual axis because the optical zone diameter is so small. As corneal GP lenses tend to center over the apex of the cornea, only central cones will result in the proper positioning for desired optical performance.
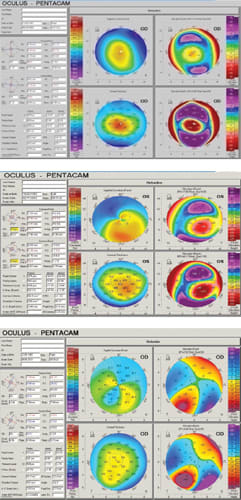
Figure 5. Various topographic shapes that influence corneal GP lens diameter and design: Figure 5a (top). Small central cone. Figure 5b (center). Oval decentered cone. Figure 5c (bottom). Pellucid-like decentered cone.
When faced with larger, more decentered cones, also known as oval or sagging cones (Figure 5b), we typically fit larger-diameter GP corneal lenses that tend to range in diameter from 9.2mm to just under 11.0mm, with optical zone diameters of 7.2mm to 9.0mm. Select the initial base curve radius for diagnostic fitting based on the steep keratometric or apical topographic curvature. Clearance over the apex of the cone is desired; however, often in these cases feather touch or light apical bearing must be accepted. Examples of this type of lens include proprietary designs such as I Kone (Valley Contax, Advanced Vision Technologies) and Keratoconic Bi-Aspheric or KBA (Essilor, Precision Technology Services) as well as custom GP designs.
Finally, even larger and more decentered cones (also known as globus cones) (Figure 5c) as well as pellucid marginal degeneration cases often require corneal GP lens designs known as intralimbal lenses. These lenses are typically 11.0mm to 12.2mm in overall diameter and have optical zone diameters as large as 8.5mm to 9.4mm. These lenses are typically fit so that the periphery of the lens is within less than 1mm of the limbus. Choose an initial base curve radius for diagnostic fitting that is slightly steeper than the mid-K value or based on curvature approximately 4.0mm temporal on the topographic axial/sagittal map. When fit well, these lenses demonstrate corneal alignment or perhaps light apical touch along with limited on-eye movement compared to smaller-diameter corneal GP lenses.
Piggyback or Tandem Lens Systems
A "piggyback" contact lens system, which consists of a GP lens fit over a soft lens, continues to be very useful in keratoconus management. Perhaps a more appropriate term for this type of lens system, as described by Jerome Legerton, OD, is a "tandem" contact lens system. Most commonly, a thin, low-powered soft contact lens is initially placed on the cornea, then a corneal GP contact lens is applied on top (Figure 6). The combination system provides a number of advantages, including improved overall on-eye comfort compared to a corneal GP lens fit directly on the cornea, and potentially improved centration of the GP lens over the corneal optics. Finally, there is better corneal surface protection in cases in which epithelial compromise cannot be avoided when a GP lens is placed directly on the cornea.
Today we have the advantage of numerous soft lenses that have high oxygen transmission and are also frequent replacement or disposable. Monthly or two-week replacement silicone hydrogel lenses such as Air Optix Night and Day Aqua (Alcon, Dk/t = 175), Acuvue Oasys (Vistakon, Dk/t = 147), PureVision2 (Bausch + Lomb [B+L], Dk/t = 112), and Biofinity (CooperVision, Dk/t = 160) are most commonly utilized in piggyback/tandem lens systems.

Figure 6. A well-fit piggyback/tandem contact lens system.

Figure 7. Soft lens edge fluting with a high-modulus soft lens in a piggyback/ tandem lens system.
Perhaps the best option available now would be to use a highoxygen-permeable daily disposable lens for such use. With the introduction of Acuvue TruEye (Vistakon, Dk/t = 118) and Dailies Total1 (Alcon, Dk/t = 156), we have excellent options available for this purpose.
Another attribute to consider in selecting the soft contact lens is modulus. Higher-modulus soft contact lenses may result in edge fluting or gape (Figure 7) when fit on steeper and more asymmetric keratoconic corneas.
There are two ways to address the problem of GP lens instability in a piggyback/tandem contact lens system. First, a higher plus or hyperopic soft frequent replacement lens (e.g., +6.00D) may add central thickness, thus providing some minimal masking effect of the corneal irregularity and forming a pseudo-central apex on which the GP lens can center and stabilize. When utilizing such higher-powered soft lenses, bear in mind that the soft contact lens will contribute approximately 20 percent of its labeled lens power to the tandem lens system. The second option is a recessed soft lens carrier. Such a soft lens has a cut-out portion in which the GP lens is placed, and if fit properly it will remain centered and stable within the recess. Examples of this type of soft lens carrier include the Recessed Pillow Lens System or "RPLS" (Fusion Technologies and EyeVis Eye and Vision Research, Figure 8) and the Flexlens Piggyback lens (X-Cel).

Figure 8. Recessed Pillow Lens System. Figure 8a (left) shows the actual lenses on a patient's eye, and Figure 8b (right) shows a schematic representation demonstrating the angular cut-out and recess in the soft carrier lens that allows for GP lens centration and stability.
Hybrid Lenses
With a GP lens center and a soft lens periphery, hybrid contact lenses can provide the optical performance of a corneal GP lens with comfort more similar to a soft lens. Not only do hybrid lenses offer improved lens centration and stability, they also offer reduced complexity in lens handling and care when compared to other corneal GP alternatives or combination approaches such as piggyback/tandem systems. Earlier versions of hybrid lenses had very low oxygen transmission and junctional weakness that caused lens splitting at the rigid/soft junction. Problems with hybrid lenses have included lens tightening over time with secondary inflammatory responses and progressive discomfort. Newer designs and fitting methodologies have significantly addressed these issues.
More recent generations of hybrid lenses are manufactured using high-oxygen-transmission materials in both the GP center and the soft peripheral skirt. The soft skirt helps center the GP lens component, which is required to significantly reduce distortion from higher-order aberrations that occur in keratoconus and other forms of corneal ectasia. Clinical complications of hypoxia and difficulty with lens removal were reported with previous generations of hybrid lenses; however, the increased Dk values of recent generations of hybrid lenses and their expanded range of fitting parameters have seemingly improved clinical outcomes in keratoconus patients, with reported fitting success rates of over 86 percent.
In fact, the most recently released hybrid lens design, UltraHealth (SynergEyes), contains a GP center with a Dk of 130 and a silicone hydrogel soft skirt with a Dk of 84. Thus, patients who have a more compromised cornea (i.e., post-corneal graft) and dry eye complaints may benefit from this latest hybrid technology due to its enhanced oxygen permeability and lowered wetting angle secondary to a plasma-like treatment process across the entire lens surface.
A reverse geometry design has also been incorporated in the recent hybrid lens platform. This welcomed addition has further enhanced the clinical applications of hybrid lenses in irregular cornea patients. Not only does this feature enable increased midperipheral sagittal height to better vault over a decentered corneal apex, it also improves overall optics by approximating the optical zone closer to the corneal plane.
The introduction of new generations of hybrid lenses over the last few years have been accompanied by updates in their fitting nomograms. This has resulted in improved lens-to-cornea fitting relationships and improved maintenance of lens movement, which is key to successful hybrid lens fitting. Experience has shown that applying conventional rigid contact lens fitting methodologies to the GP center, combined with flatter soft skirt curves to maximize alignment and tear flow, will result in higher success rates.
In addition to the improved fitting algorithms, there is also evidence demonstrating the possibility of topography-assisted hybrid contact lens fitting. Such clinical tools may be able to streamline future fitting processes in keratoconus patients who can benefit from this new lens platform.
Scleral Lenses
Scleral GP contact lens use has been gaining wider clinical acceptance over the past few years, especially for fitting irregular corneas. The advantages provided by scleral lenses include improved comfort when they are fit to align the relatively insensitive conjunctival/ scleral surface, corneal surface protection by providing a "bath" of tears between the lens and the cornea, and excellent lens centration and stability even for highly irregular corneas.
The primary criteria in successfully fitting scleral lenses are to fully vault the cornea, have increased vault in the limbal zone, and to align the conjunctival/ scleral surface with lens haptic. The initial decision to make when fitting a scleral lens is what diameter to select. Generally speaking, the more irregular the corneal surface, the larger the diameter should be to fully vault the corneal surface. Larger-diameter lenses are typically fit with greater vault compared to smaller scleral lenses. Vault centrally can range from under 100 microns to well over 400 microns depending on the lens design and the specifics of the case involved. One consideration when fitting with significant central vault is the effect on the quality of optics. High-vault fits are often associated with reduced optical quality, which can potentially result in reduced bestachievable visual acuity. Newer scleral lens designs incorporate reverse geometry configurations that allow corneal vaulting in cases of severe corneal irregularity or when an elevated peripheral cornea may result in limbal bearing such as in some post-penetrating keratoplasty cases that have secondary oblate topographies. You can estimate corneal vault by highlighting the retro-lens tear layer with sodium fluorescein and comparing that thickness to the known center thickness of the lens itself. Anterior segment ocular coherence tomography (OCT) can more accurately obtain imaging and measurements of vault as well as peripheral conjunctival/scleral lens alignment (Figure 9).
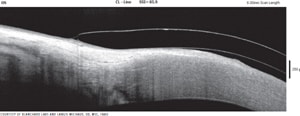
Figure 9. Utilization of anterior segment OCT to evaluate peripheral landing of a scleral GP lens.
Many Ways to Achieve Keratoconus Contact Lens Fitting Success
Comprehensive management of keratoconus involves a clear understanding of the disease and the integration of all available treatment methods to control progression, reduce severity, and to provide optimal visual performance. Contact lenses remain the primary modality of vision correction for patients who have keratoconus. Historical thinking has equated contact lenses for keratoconus with GP corneal lenses. While corneal GP lenses still play a prominent role, today we have a multitude of contact lens options for managing keratoconus. Understanding the appropriate application of these contact lens alternatives will help optimize clinical outcomes for our patients who suffer from keratoconus and other forms of corneal ectasia and irregularity. CLS
To obtain references for this article, please visit http://www.clspectrum.com/references.asp and click on document #217.



