Irregular Cornea Fitting
Irregular Cornea Fitting Grand Rounds
Many tools and resources are available to help you improve the vision and quality of life of patients who have irregular corneas.
By Robert J. Maynard, OD

|
Dr. Maynard has been in private practice in Arizona for 46 years. He is a past president and current member of the Arizona Optometric Association as well as a member of the Contact Lens Section of the American Optometric Association and the Central Arizona Optometric Association. In addition, Dr. Maynard is a clinical investigator for contact lenses and solutions with companies such as Boston material, Barnes-Hind, and Vistakon. |
One of the most challenging yet enjoyable aspects of contact lens practice is managing patients who have irregular corneas. GP contact lenses play a significant role in managing such patients. We have many lens designs and tools available today to help us achieve success with GP lens fitting. In addition, laboratory consultants are available to guide us through the fitting and problem-solving process.
Successfully fitting an irregular cornea is often life-changing for the patient. This article presents the lens fitting process and outcomes of three such cases.
Case 1: Post-Penetrating Keratoplasty
Background This 64-year-old physician presented with a corneal transplant OD that he underwent as a result of herpes simplex keratitis. (Modified from Bennett et al. GP Case Grand Rounds Troubleshooting Guide.)
Initial Evaluation and Lens Fitting The patient’s manifest refraction OD was +3.25 –0.75 × 064, >20/400 (count fingers at 8 feet). His keratometry reading OD was 45.25 @ 138/50.50 @ 048. Slit lamp evaluation showed corneal edema and scarring from 7 o’clock to 8 o’clock in front of the pupil. The iris was badly damaged, with an offset pupil. The scarring and edema were on an “island” of tissue.
At this first visit, we used a Surgi-Lens (reverse geometry design from ABB Concise) lens for an initial diagnostic fit. The parameters OD were:
• Power: +4.00D
• Base curve radius (BCR): 8.04mm
• Overall diameter (OAD): 10.3mm
• Optical zone diameter (OZD): 7.7mm
• Cap size: 7.7mm
• Secondary curve radius/width (SCR/W): 7.50mm/0.6mm
• Peripheral curve radius/width (PCR/W): 10.80mm/0.5mm
The patient’s visual acuity with this lens was 20/25-1. Slit lamp examination showed that the contact lens moved well but decentered nasally to the limbus. With fluorescein, there was apical clearance with slight inferior edge clearance.
First Follow-Up Visit One week later, the over-refraction with this lens was plano and the visual acuity was 20/25-3. Slit lamp examination showed that the contact lens decentered nasally and locked in position over the nasal limbus, exhibiting no movement with the blink. The fluorescein pattern showed isolated areas of pooling superiorly, nasally, and inferiorly as well as dimple veiling between 11 o’clock and 12 o’clock (Figure 1). An adherence ring was evident upon lens removal (Figure 2).
After reblending the inside lens surfaces, we rescheduled the patient to return in one week.
Second Follow-Up Visit At the two-week visit, the patient’s manifest refraction OD was +3.00 –0.50 × 165. His over-refraction was +0.25 –1.25 × 065, and his visual acuity was 20/25-1. The slit lamp examination OD showed that the lens still appeared to be adherent. However, there were no signs of abrasion or edema, and some tear exchange was occurring. There was lens clearance both superior-temporally and inferiornasally. We prescribed spectacles to correct the over-refraction and provide optimal vision for the right eye.

Figure 1. Right lens fluorescein pattern in Case 1.
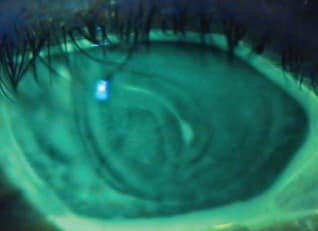
Figure 2. Adherence ring upon lens removal in Case 1.
Final Outcome We ordered the final lens with a larger diameter and flatter base curve radius in a hyper-Dk material. The final lens parameters OD were:
• Power: +4.00D
• BCR: 8.13mm
• OAD: 10.80mm
• OZD: 8.60mm
• Cap size: 8.60mm
• Material: Boston XO (Bausch + Lomb)
The patient’s visual acuity OD with this lens was 20/25-2. Slit lamp examination showed that the lens decentered slightly nasally with slight movement with the blink and mild apical clearance. There was a small area of inferior bearing, but no staining in this area. Figure 3 shows the corneal topography OD. Overall, the patient has been very satisfied with the vision and comfort achieved with the final lens.
Discussion/Alternative Management Options
This case demonstrates the importance of considering reverse geometry designs when fitting irregular cornea patients. Reverse geometry designs are predominantly indicated in post-refractive surgery and corneal reshaping cases. Although the topography map of this patient’s right eye did not exhibit a clear paracentral/midperipheral steepening oblate pattern, this case shows that reverse geometry lenses can be successful for post-penetrating keratoplasty patients. The Gas Permeable Lens Institute’s (GPLI) website at www.gpli.info features a comprehensive database of lens designs, including a list of reverse geometry lens designs, from all of the CLMA member laboratories.
This case also illustrates the importance of in-office modification. A simple edge or surface polish, or—as in this case—reblending or flattening of the peripheral curve radii can improve lens comfort, the fitting relationship, or both. Furthermore, the use of a hyper-Dk material is indicated in such cases to optimize corneal integrity and minimize the potential for edema in the newly transplanted cornea.
Large-diameter lenses (i.e., intralimbal and other similar designs) are often indicated in these cases because of their ability to center, to optimize initial comfort, and to overlap the graft. In this case, a 10.80mm lens provided the best fitting relationship. It is also important to emphasize that an ideal alignment fitting relationship is very difficult to achieve in these cases; therefore, there may be some decentration, regional bearing, and/or excessive clearance. You must consider the risk-to-benefit ratio, especially as it pertains to a patient’s quality of life.
Case 2: Post-LASIK/IOL
Background This 77-year-old female patient presented in June 2012 with a history of LASIK (with enhancements) OD and OS (1999) and bilateral intraocular lens (IOL) implants in 2005. She had an active social life and wanted clear distance vision. The patient was a former spherical GP lens wearer. She was not pleased with the vision out of her glasses, which she removed to see at near.

Figure 3. Corneal topography of patient in Case 1.
Initial Evaluation and Lens Fitting The patients visual acuity (with spectacles) was OD 20/40 and OS 20/80. Her manifest refraction was OD −2.25 −1.00 x 180, 20/20 and OS −2.00 −1.75 × 002, 20/20. Keratometry readings were OD 42.25 @ 180/43.50 @ 090 and OS 43.25 @ 007/45.00 @ 097. Figure 4 shows the patient’s corneal topography. Slit lamp examination showed superior stromal scarring with inferior iron deposits at 6 o’clock OD and an inferior rust deposit between 6 o’clock and 7 o’clock OS.
We fit this patient into the Maxim (AccuLens) scleral lens. The original right diagnostic lens had a sag value of 4.15, which was insufficient and resulted in central touch. The 4.42 sag lens resulted in a better fit, although a slightly higher sag value may be optimum. A similar result occurred with the left eye, for which a much higher sag value lens was required.

Figure 4. Corneal topography of patient in Case 2, right eye (on left) and left eye (on right).
The parameters of the initially dispensed Maxim scleral lenses were:
• Power: −5.50D OD, −3.00D OS
• Sag: 4.47 OD and OS
• BCR: 7.50mm OD, 7.85mm OS
• OAD: 16.0mm OD and OS
• OZD: 9.0mm OD, 10.0mm OS
The visual acuity with these lenses was 20/20 OD and OS. Over-refraction was OD plano, 20/20 and OS +0.50DS, 20/20. Slit lamp examination showed that OD the lens was well-centered and moved well with the blink. There was good fluorescein pooling centrally and sufficient clearance peripherally. We noted possible mild impingement nasally between 2 o’clock and 3 o’clock. The left eye exhibited a similar pattern, with slight nasal and temporal impingement.
First Follow-Up Visit The patient returned 11 days later. She reported no symptoms and was satisfied with both the vision and comfort OD and OS. The results were identical to those of the initial dispensing visit.
Second Follow-Up Visit The patient returned six weeks later and reported noticing redness and a ring around both of her eyes after lens removal. Her vision was somewhat “filmy.” Slit lamp examination showed good central clearance OD and OS. Both lenses exhibited some sectoral impingement/blanching, although when we applied fluorescein the dye quickly moved beneath the lens. Both lenses had a muco-protein film, which we cleaned in-office. An indentation ring was evident OD and OS with lens removal (Figure 5).
After contacting the laboratory and discussing the case with a consultant, we made adjustments to the diameter, flattened the periphery, and added the original over-refraction to the left lens power.
Final Outcome We dispensed final lenses in the following parameters:
• Power: −5.50D OD, −2.50D OS
• Sag: 4.45 OD, 4.74 OS
• BCR: 7.50mm OD, 7.85mm OS
• OAD: 16.2mm OD, 16.7mm OS
• OZD: 9.1mm OD, 10.1mm OS
The distance visual acuity with these lenses was 20/20 OD and OS and 20/15 OU. Slit lamp examination showed that both lenses exhibited optimal central and limbal clearance with no impingement (Figure 6).Three months later, we found no change in fitting relationship, vision, or comfort, and the patient was very satisfied with these lenses.

Figure 5. Indentation ring OD (on left) and OS (on right) after lens removal in Case 2.

Figure 6. Final lens-to-cornea fitting relationship OD (on left) and OS (on right) in Case 2.
Discussion/Alternative Management Options
Scleral lenses are rapidly becoming an essential part of any contact lens practitioner’s “toolbox,” especially for irregular cornea patients. This case illustrates how such a design was able to significantly improve vision and patient satisfaction. Post-penetrating keratoplasty patients and deep anterior lamellar keratoplasty patients who have highly irregular corneas can benefit from scleral lenses, as can some post-refractive surgery patients who’ve experienced less-than-optimal outcomes such as this patient.
This case also illustrates how valuable laboratory consultants can be in all aspects of the fitting process, especially for problem-solving. Any aides in the form of corneal topography maps, lens-to-cornea fitting photos, or even video of the fluorescein pattern are invaluable to consultants in making contact lens parameter changes.
Another invaluable resource is the Scleral Lens Education Society (www.sclerallens.org), which offers informational videos and resources for both patients and practitioners. These resources have become even more important with the increasing application of scleral lenses for correcting healthy astigmatic and presbyopic eyes.
Case 3: Post-Refractive Surgery
Background This 36-year-old male computer sales executive presented with a history of radial keratotomy OD and OS, followed three years later by LASIK OD and OS.
Initial Evaluation and Lens Fitting The patient’s visual acuity (with spectacles) was OD 20/80-1 and OS 20/100. His manifest refraction was OD −2.00 −0.75 × 013, 20/25-1 with ghosting and doubling and OS +3.00 −5.00 x 098, 20/25-1 with ghosting and doubling. Keratometry readings were OD 41.37 @ 018/45.37 @ 108 and OS 34.50 @ 109/43.12 @ 019.
We selected Comfort Kone (Metro Optics) as our initial diagnostic lenses in the following parameters:
• Power: −6.50D OD, −7.25D OS
• BCR: 7.67mm OD, 7.50mm OS
• OAD: 11.2mm OD and OS
• OZD: 8.8mm OD and OS
• SCR/W: 9.00mm/0.50mm OD and OS
• PCR/W: 11.75mm/0.50mm OD and OS
The over-refraction with these lenses was OD +0.75DS, 20/30 and OS +0.75DS, 20/25. Slit lamp examination showed that the lens OD was well-centered and moved well with the blink, with good fluorescein pooling centrally, superiorly, and inferiorly. The lens OS was also well-centered and moved well with the blink. There was central pooling with slight touch superior-temporally, slight touch nasally, and slight touch inferior-temporally.
First Follow-Up Visit Two weeks later, visual acuity (with lenses) was OD 20/100 (foggy vision) and OS 20/200 (foggy vision). Slit lamp examination showed that both lenses were centered over the superior limbus, with dimple veiling over the papillary zone; the lenses appeared to be tilting backward over the superior limbus.
The second pair of lenses that we selected had the following parameters:
• Power: −5.75D OD, −6.75D OS
• BCR: 7.80mm OD, 7.58mm OS
• OAD: 11.2mm OD and OS
• OZD: 8.4mm OD and OS
• Cap size: 8.40mm OD and OS
• SCR/W: 8.80mm/0.70mm OD and 8.60mm/0.70mm OS
• PCR/W: 10.00mm/0.50mm OD and OS
Over-refraction was OD +1.50DS, 20/30 and OS + 1.75DS, 20/25-2. Slit lamp examination showed that the lens OD was well-centered and moved well with the blink. A bubble was present at 12 o’clock above the pupil. The lens OS exhibited a similar fitting relationship, with the addition of mild dimple veiling.
Second Follow-Up Visit Two weeks later, visual acuity with this pair of contact lenses was OD 20/30+2 and OS 20/40-1. Over-refraction was OD +0.50DS, 20/30+2 and OS +1.75DS, 20/25-2. Slit lamp examination showed that the lens OD was well-centered with apical clearance and good peripheral edge clearance. The lens OS exhibited an identical fitting relationship with the exception of mild dimple veiling superiorly.

Figure 7. Fitting relationship of the right eye in Case 3.

Figure 8. Fitting relationship of the left eye in Case 3. Dimple veiling is evident centrally.
We selected a new lens OS only in the following parameters:
• Power: −6.75D
• BCR: 7.58mm
• OAD: 11.2mm
• OZD: 8.4mm × 9.0mm (oval)
• SCR/W: 8.60mm/0.70mm
• PCR/W: 10.00mm/0.50mm
Over-refraction with this lens OS was plano 20/25-2 (fluctuates). Slit lamp examination showed that the lens OS exhibited good centration and movement, although dimple veiling was still present in various regions beneath the lens.
Final Outcome We kept the right contact lens essentially unchanged, as it continued to provide excellent vision and comfort. We modified the left lens several more times, including adding fenestrations to reduce the dimple veil problem. The final lens parameters were as follows:
• Power: −5.75D OD, −6.00D OS
• BCR: 7.80mm OD, 7.50mm OS
• OAD: 11.2mm OD, 10.6mm OS
• OZD: 8.4mm OD, 6.8mm × 7.8mm (oval) OS
• Cap Size: 8.20mm OD, 6.80mm OS
• SCR/W: 8.80mm/0.70mm OD, 8.50mm/0.85mm OS
• PCR/W: 10.00mm/0.50mm OD, 10.50mm/0.85mm OS
• Five fenestrations (OS only)
Over-refraction with these lenses was OD +0.50DS, 20/25-2 and OS −0.75DS, 20/20-2. Slit lamp examination showed that the lens OD was decentered slightly superiorly with mild dimple veiling paracentrally at 4 o’clock and just inside the superior limbus from 11:30 to 12:30. The lens OS exhibited a similar fitting relationship, with good lid attachment. The fenestrations appeared to be successful. Minor punctate stain was evident at 4 o’clock, with very minor scattered dimple veiling and some inferior edge standoff. Figures 7 and 8 show the lens-to-cornea fitting relationships of both lenses. Overall, the patient was “delighted” with his vision and comfort. We decided to not correct the over-refraction for the left eye, as he would not gain that much improvement.
We instructed the patient to return for another complete primary care examination in three months. At this visit, his vision was holding steady, the fitting relationship was still good, and he had no complaints; therefore, we scheduled him to return for a routine six-month contact lens evaluation.
To date, the patient has retained this same pair of contact lenses, with only a minor power change to both. He has maintained good visual acuity as well as excellent corneal health.
Discussion/Alternative Management Options This case demonstrates the importance and benefits of having patience during the fitting process. It took 10 months to achieve a successful contact lens fit for his left eye, but it was well worth the effort. The oval optical zone and the fenestrations were exceptions to the rule for such fits, but their importance should not be discounted.
This case is yet another example of how important CLMA laboratory consultants can be. Their experience is invaluable when troubleshooting lens design parameter changes for irregular corneas. In addition, corneal topography is invaluable in managing these cases and should be shared with your laboratory in determining the final lens design parameters.
This case also illustrates the importance of the “risk-to-benefit” ratio. It is almost impossible to achieve a perfect alignment fitting relationship on an irregular cornea; therefore, we should strive to obtain the best possible contact lens fit, knowing that there may be slight compromise to the cornea, as the visual benefits for such patients can be life-changing. In this case, the patient was extremely pleased and experienced a better quality of life as his corrected visual acuity improved from an initial 20/80 OD and 20/100 OS to 20/25 OD and OS. The dimple veiling, which results from bubbles beneath the lens or an indentation in the epithelium (but it is not staining) should not be alarming if it does not impact visual acuity (i.e., as it would if excessive dimpling was located centrally). It is often caused by excessive pooling, a not uncommon clinical finding when a GP lens is fit to an irregular cornea.
It is evident that a GP contact lens was certainly indicated in this case—as is true for almost every irregular cornea patient because of a GP lens’ ability to provide a more spherical corneal contour and thus improve visual acuity. You can use corneal topography to determine the type of GP contact lens design to fit on a particular patient. For instance, in most post-refractive surgery patients, a reverse geometry lens design is indicated because of the flatter central topography (versus paracentral/midperipheral). A recent corneal topography map of this patient (Figure 9) illustrates that a reverse geometry design could have been considered as well.

Figure 9. Corneal topography for the patient in Case 3.
Summary
These cases demonstrate the potential for success of the latest GP tools for managing irregular cornea patients and how you can improve the quality of life for those fit into these designs. They are not overly complex—all you need is the motivation to fit them, to carefully assess the fitting relationships, and to utilize available fitting resources, most notably the laboratory consultants. The results are not only life-changing for patients, but can be rewarding professionally for you as well. CLS



