Soft Lens Fitting
Reviving the Art of Soft Lens Fitting
Fitting soft lenses involves more than keratometry readings and base curve selection.
By Eef van der Worp, BOptom, PhD, FAAO, FIACLE, FBCLA, FSLS

|
Eef van der Worp is an educator and researcher. He has served as a head of the contact lens department at the Hogeschool van Utrecht in the Netherlands (NL) for over eight years. He is currently affiliated with the University of Maastricht as an associate researcher, a visiting scientist at Manchester University (Manchester, U.K.), an adjunct professor at the University of Montreal College of Optometry (CA), and an adjunct assistant professor at Pacific University College of Optometry. He has received educational grants from Bausch + Lomb Boston and Contamac. |
This article will focus on soft contact lens “fitting,” although perhaps we should say soft contact lens “selection,” because we haven’t been “fitting” soft lenses for some time now. To the surprise of some and the discontent of others, central keratometry values are not very useful in fitting soft lenses. In other words, there is a very weak correlation between the central K readings and the soft lens fit. What, then, about the base curve values printed on the lens boxes? What does the number “8.3”or “8.6” mean?
Eye Shape and Soft Lenses
In daily contact lens practice, we should always be aware of the eye’s shape and take this into account when fitting contact lenses. Therefore, we should respect the anterior ocular surface shape. This is true for all types of lenses and for every individual.
Similar to GP lenses, soft lenses can have an impact on the cornea and on corneal shape if fitted incorrectly. However, are most practitioners even aware of the lens design when they fit soft lenses? Is it a monocurve? A bicurve? An aspheric lens? If a lens has a monocurve design, this could interfere with corneal shape, as the cornea flattens toward the periphery (in some eyes more so than in others).
The fitting of soft lenses unfortunately has become a bit of a lost art. Corneal deformations as a result of suboptimal soft lens fittings are not as uncommon as many may think. If practitioners would remove soft lenses at every follow-up visit and perform corneal topography, they would be surprised by the amount of unwanted changes that can take place beneath a soft lens (Figure 1). According to a study by Schornack et al in Contact Lens & Anterior Eye (2003), about one-third of all corneal warpage cases result from soft contact lenses. Refractive surgeons have made it quite clear for some time that it is critically important to cease soft lens wear for a substantial period of time to let the cornea settle before laser surgery can take place. In fact, most unsuccessful refractive surgery outcomes that result in residual refractive error are caused by lens wearers who undergo the procedure before their corneas have had sufficient time to stabilize.

Figure 1. Corneal warpage beneath a soft lens OD and OS.
The main question here is—what is “sufficient time”? That really depends on what criterion is used. According to a study by Ng et al in Optometry & Vision Science (2007), it takes on average 10.7 ± 10.4 days before a stable refractive state is reached after cessation of soft lens wear. If we use the keratometry value as the criterion, then it takes an average of 16.2 ± 17.5 days for the cornea to become stable. Using corneal topography, it takes 28.1 ± 17.7 days. For the mentioned methods, a change of 0.5D or less between two examinations is used as the criterion. But if pachymetry (corneal thickness measurement) is used as a method, then it takes on average 35.1 ± 20.8 days before stability is reached in a soft lens wearer (with an 8μm change at the thinnest point on the cornea as the criterion).
It is also interesting to note the large spread within these outcomes—for some subjects it apparently takes significantly longer compared to the average eye before the cornea is considered stable.
Base Curve Radius
The indicated base curve on a soft contact lens package (usually expressed in numbers with or without mm) is by many considered to be the lens’ back surface radius. However, it may be more useful to consider this as more of a stock sorting helper and a symbolic value. More often than not, it is questionable as to whether the contact lens actually has an 8.3mm or 8.6mm spherical base curve on its back surface. A “base curve equivalent” or BCE would perhaps be a more appropriate term.
Some contact lens designs feature eccentricity to mark a flattening toward the periphery, as well as an edge lift, which together with the base curve form the total sagittal (sag) height across the total diameter of the lens. So the way in which the lens fits is certainly not defined by that single number on the lens box. The total sag height and diameter combination of the contact lens is of much more importance, and this should relate to the sag height of the anterior ocular surface and to the shape of the limbus—i.e., the transition from the cornea into the conjunctiva/anterior sclera.
The total sag height of the ocular surface can be calculated over a certain diameter, called a “chord.” The distance from a baseline (chord, base of the sagitta) to the top of the sagitta is the sag height. For a normal eye, the total sag height of the anterior ocular surface is roughly 3,700 microns for a 15mm chord, according to studies at Pacific University. The variation, defined as standard deviation, is fairly limited: roughly 200 microns. To put things in perspective, in scleral lens fitting, a 200-micron difference would typically be one step up or down in a scleral lens trial set. As another reference: in keratoconus, the total sag height is estimated to be about 200 microns higher, or 3,900 microns, over a 15mm chord because of the ectasia—but with a slightly higher variation, as you may expect (in the 400-micron range). New instruments can measure optical coherence tomography (OCT) and “fringe topography,” such as that generated with the new Eye Surface Profiler (Eaglet-Eye) (Figures 2 and 3). These devices are capable of imaging the total sag height of the ocular surface over any given chord and offer substantial diagnostic assistance.
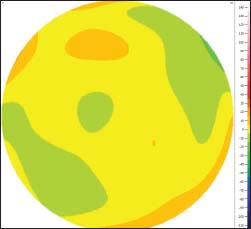

Figure 2. Height topography map of a normal eye with the Eye Surface Profiler. 2a shows the relative height map with an even pattern (scale in microns compared to a best-fit sphere). Figure 2b shows the absolute height map, with a sagittal profile of the anterior ocular surface (sagittal values in microns).


Figure 3. Height topography map of advanced keratoconus with the Eye Surface Profiler. Figure 3a shows a relative height map with severe irregularities and a decentered top of the cone (scale in microns compared to a best-fit sphere). Figure 3b shows the absolute height map, with a sagittal profile (sagittal values more than 200 microns higher than that of the normal eye in Figure 2).
Lens Sag Height
If we have a given sag height, as described above, we can potentially use this information in contact lens practice. The goal is to fit (or select) a soft lens with a sag height that correlates to that of the anterior ocular surface. But there is more to it than that. As mentioned previously, for any cornea or lens of choice, many variables together form the total sag height of that cornea or lens; radius of central curvature is just one of them. The numeric eccentricity of the approximated elliptical shape of the cornea is another, and the shape of the limbus and the anterior sclera/conjunctiva adds an additional variable.
OCT imaging has recently showed that the transition from cornea to sclera (the corneoscleral profile) is actually quite different from what we had previously assumed. Specifically, the anterior ocular surface is not composed of a steep corneal curve placed on a flatter scleral curve, with a concave or hollow limbal area. Rather, the transition from cornea to sclera is relatively straight or tangential in shape—e.g., it continues in an almost straight line in many cases (van der Worp et al, 2010). This may change the way we look at peripheral soft lens design in the future. Hall et al (2013) recently showed that the corneoscleral profile shape is related to soft contact lens fit (movement), which could have some interesting clinical implications.
Young et al (2010) showed that for aspheric soft lenses, the eccentricity has a larger impact on total sag height than central radius has. For example: a 0.12 change in eccentricity is believed to be equivalent to a 0.2mm base curve radius change. In addition, diameter seems to play an even larger role (Figure 4). For instance, an increase in lens diameter from 14.0mm to 15.0mm in a contact lens that has an 8.3mm base curve can add up to a 700- or 900-micron increase in sag height depending on whether the lens design is spherical, aspheric, or multicurve. The effect is slightly less for an 8.7mm base curve radius because the total sag height of that lens is also less, but it still could increase the sag height by 600 microns to 750 microns.
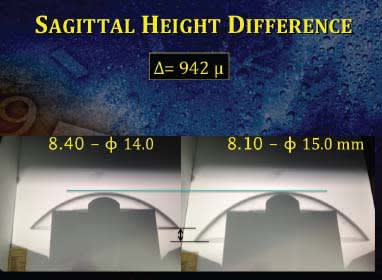
Figure 4. Sagittal height difference between an 8.4mm base curve soft lens with a 14.0mm diameter and an 8.1mm base curve soft lens with a 15.0mm diameter with the same lens geometry from one trial set. The total difference is 942 microns.
This has significant consequences when we fit toric soft lenses, as they are commonly 0.5mm or more larger than their spherical variant, resulting in a change of easily 500 or 600 microns—or about the thickness of the entire cornea, which is about 540 microns on average.
By comparison, if we change an 8.3mm base curve to an 8.7mm base curve while keeping the total diameter the same, then this change in sag height would be in the order of 300 microns, which is much more limited. The lens becomes “flatter,” although it would actually be better in this regard to refer to it as having less sag height. Perhaps going forward we should refrain altogether from using terms such as “flatter” or “steeper” in soft contact lens fitting and rather transition into using terms such as “higher” and “lower” sag values to better convey what is happening on the ocular surface. In scleral lens fitting, these terms have now become fairly mainstream and are widely used.
If we think in terms of changing contact lens fit—because a lens is too tight, for instance—then we should think about changing the diameter first rather than changing the base curve radius if we want to have a significant impact. In defense of using the radius, eyes that have flatter central K values more often also have larger corneal diameters. In that sense, there may be some indirect relationship between curvature and lens fit. Nonetheless, it would be better to look directly at the more influential parameter—corneal diameter.
Therefore, if a cornea is larger than average, and if the central K readings are steep and/or the eccentricity is low, this combination has a huge impact on the total sag height of that cornea and consequently on the soft contact lens of choice. Of course, the opposite is also true: smaller corneal diameters combined with flat curves and high eccentricities result in clinically significant lower sag values, for which the lens sag should be selected accordingly to achieve an optimal or acceptable contact lens fit.
That said, measuring corneal diameter is an art in itself. First, there is typically a difference between the horizontal and the vertical corneal diameters (the vertical being smaller compared to the horizontal). Additionally, the vertical diameter is difficult to measure, as the eyelids can be a physical barrier. It is common practice to use the oblique meridian as some sort of “average value.” Measuring “white-to-white” at a 45-degree angle using a corneal topographer may be a good way of doing this, rather than using a ruler.
How Bent are Curves?
It follows, therefore, that sag height might become a new standard in soft contact lens fitting, as it seems to be a much more relevant parameter relative to other variables. Radius and curvature may become obsolete in the future. Lathes that manufacture contact lenses and that make molds for cast-molded soft lens production “think” exclusively in height—not in curves. With up to micron accuracy (or even fractions of that—nanos, which are 1/1000 of a micron), the height can be programmed as long as there is an x,y,z coordinate. Such capabilities are generally possible in this new age of 3D printing. But what should we do as contact lens practitioners? We still seem to live in the last century, relying on trial sets that have huge parameter steps and on contact lenses that offer no clue about their design and shape.
So, is the base curve radius that is printed on the soft lens box completely useless? Does an 8.3mm base curve result in a “steeper fit” compared to an 8.7mm base curve? For the exact same lens (design, type, and brand), that is probably true. In other words, within the same lens, if the 8.3mm lens is too tight, an 8.7mm lens with a lower sag height should provide a better fit. However, if we compare an 8.3mm base curve lens of one manufacturer to an 8.3mm base curve lens of another manufacturer, the likelihood of observing differences in the fitting characteristics is fairly high. Significant differences may occur even between different contact lens designs (brands) of one manufacturer that have the same base curve printed on the box, because we don’t know how much sag height difference there is between them. In this sense, it might be better to speak of an “A” lens and a “B” lens rather than the somewhat misleading base curve radius values on the lens box. An even better idea would be to print the absolute sag value on each lens pack.
Almost by definition, soft lenses in-vivo dehydrate. This is especially true with traditional hydrogel materials. During the course of the day, they tend to “tighten up” during wear. For this reason, manufacturers and educators suggest compensating for this by selecting traditional lenses that are around 0.7mm flatter than the central cornea. Low-water-content silicone hydrogel materials and some more water-retaining materials tighten up as well, but to a lesser extent. In theory, this means that these contact lenses can be fitted somewhat steeper. So, for instance, we should select them to be only 0.4mm flatter rather than the otherwise 0.7mm for traditional hydrogels. But it is interesting to note that with only one exception, the base curves listed on silicone hydrogel contact lens packages typically have the same or very similar values as compared to traditional hydrogel lenses even though they could be fitted steeper.
Reviving the Art
There recently has been a bit of a revival of custom-made soft lenses. Some companies even specialize in this, solely offering lenses outside of the standard range and/or custom-made lenses. Thanks to recent innovations, such custom soft contact lenses can now be manufactured in a silicone hydrogel material. But apart from these outside-of-standard and custom-made soft lenses, it may be a good idea to revisit the fitting of soft contact lenses altogether.
In an average contact lens practice, time and energy are invested in acquiring new lens wearers. But how much do we invest in our current lens wearers to give them the best available lenses today? Perhaps we can reverse the trend that is making soft lens fitting a lost art. Using sag heights in the fitting process and having those available on lens packages and trial lenses would be a big step forward. As contact lens practitioners, we are limited in what we can do, even if we strive for the best possible lens for our patients. We need better tools. Hopefully we can “elevate” soft lens fitting back to a higher level in the future. Quite literally—thinking in sag heights. CLS
Parts of this article have previously been published in different editions of Global Contact (MediaWelt GmbH). Special thanks to Helmer Schweizer of Euromcontact for his valuable input.
For references, please visit www.clspectrum.com/references.asp and click on document #214.



