Prescribing for Presbyopia
Breaking up Is Not Hard to Do
BY CRAIG W. NORMAN, FCLSA

Lens awareness. Decreased wearing time. Fluctuating vision. Dryness. We hear these symptoms often from presbyopic contact lens wearers, but what tests allow us to determine the etiology, in particular the dryness component, while lenses are being worn?
With corneal GP lenses and sclerals, this was easily evaluated during lens wear by measuring tear breakup time (TBUT). This method is performed by instilling fluorescein into the ocular tear film, then counting the seconds required for the front surface of the lens to begin to form dry spots. Evaporation and diffusion of tears across the lens surface in a normal healthy eye will start occurring between blinks at about 10 to 12 seconds, when the blink reflex kicks back in. If the TBUT is less than the blink rate, the lens surface develops dry areas, and patient awareness of lens-related dry eye is increased.
With soft lenses, the symptoms of lens dryness occur more frequently but TBUT is of no use, mainly because fluorescein is ineffective for the test. Clinically, we understand how soft lens dehydration takes place. We also know that this is exacerbated if the wearer doesn’t blink often enough or has a poor quality tear film. Newer hydrogel and silicone hydrogel materials aim to increase surface wettability, lubricity, and thus ocular compatibility.
So what method can be used in-office to evaluate on-eye soft lens surface dryness?
Alternate Tear Film Testing
One is the Oculus Keratograph 5M Topographer, which has a “dry eye suite” known as TF Scan built into its software package, allowing for tear film assessment using either white or infrared illumination. It can measure tear meniscus height, while also evaluating lipid layer and tear film dynamics. Additionally, it employs Non-Invasive Keratograph Break-Up Time (NIKBUT). The company suggests that it is primarily designed for ocular evaluation and not contact lens wetting, but our group was curious of the possibilities of analyzing tear interaction over lens surfaces.
Figures 1 to 3 demonstrate its potential in managing our presbyopic patients who describe dryness symptoms. Green colors show intact tear film, while “hotter” reddish colors show areas of tear breakup. Here, the patient’s tear film integrity was stable with both no lens on-eye and with a scleral GP, while unstable with the silicone hydrogel lens.
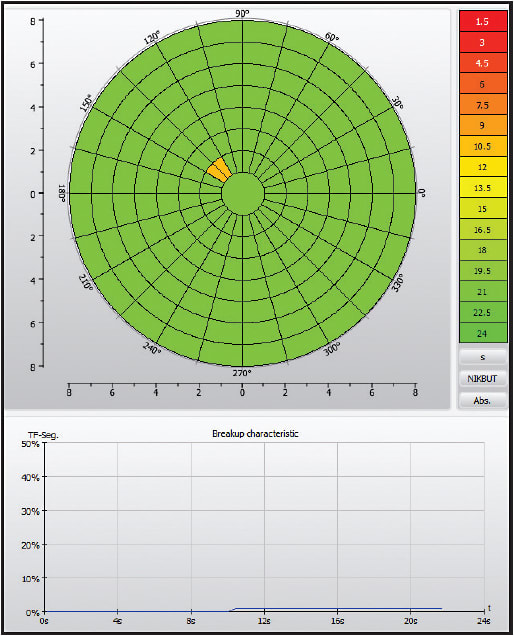
Figure 1. A baseline NIKBUT analysis with no lens on-eye.
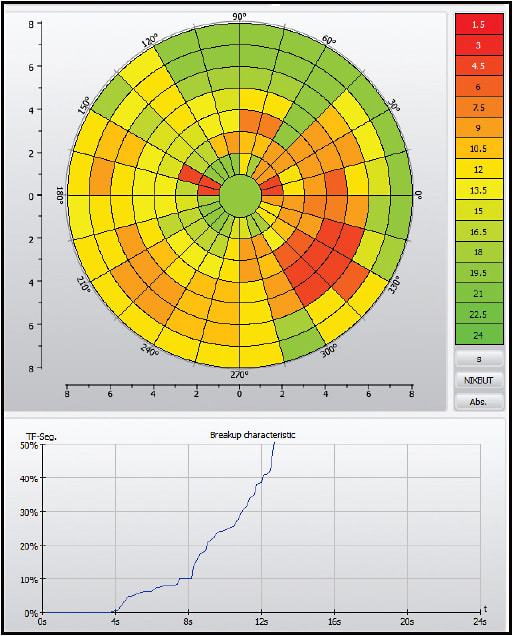
Figure 2. A NIKBUT analysis with a silicone hydrogel lens.
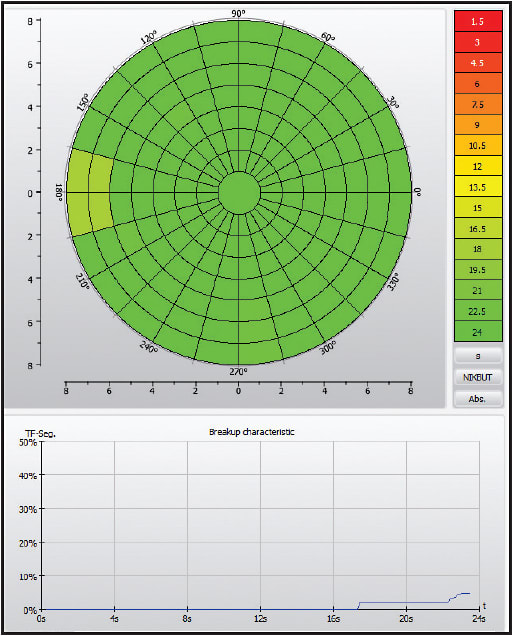
Figure 3. A NIKBUT analysis with a scleral lens.
Does this mean that the scleral lens is a better alternative in cases such as this? Maybe not. But as we further evaluate NIKBUT, it may be helpful in best lens determination among sufferers of contact lens-induced dry eye symptoms. CLS
Craig Norman is Director of Research, Michigan College of Optometry at Ferris State University. He is a fellow of the Contact Lens Society of America and is an advisor to the GP Lens Institute. You can reach him at CraigNorman@ferris.edu.



