June 2014 Online Photo Diagnosis
BY LUCIANO BASTOS
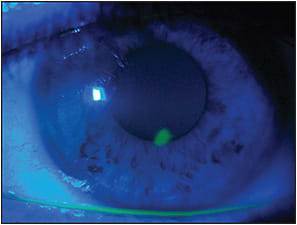
This image shows a paracentral erosion caused by a GP lens that was bearing on the apex of a keratoconic cornea. The resultant lesion is superficial and limited to the corneal epithelium, but, if it is not treated and the fit is not corrected accordingly, it may evolve into a corneal ulcer. It also may result in a corneal leukoma after healing due to breakage in Bowman's layer if it reaches the corneal stroma, especially if it is a case of recurring epithelial lesions due to repeated wear of an improperly fitted corneal GP lens.
Patients fitted with well-designed and high-quality specialty GPs typically do not complain until some discomfort develops. This particular case occured because the patient had lost his current lens and had been wearing a previous lens that was a little flatter compared to his current lens. The patient was instructed to cease lens wear and was treated with Epitezan (Allergan) three times a day for four days, after which he returned for a new fit. Figure 2 shows his previous lens that he had been wearing; the lesion had healed, and you can see the significant lens bearing that caused the erosion.
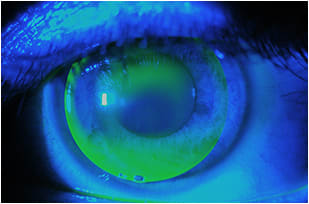
Figure 2. Lens bearing over the corneal apex.
Complications such as this can also occur with keratoconus patients who are fit with the three-point-touch technique. Keratoconic corneas are among the most challenging to fit, and the reason why many such patients have difficulty adapting to corneal GPs is because of poor lens designs or improperly fitted lenses. This explains why scleral lenses are rapidly becoming popular among practitioners; they land on the sclera and [should] not touch the cornea.
Fitting Keratoconus
Figure 3 shows the patient’s anterior corneal tomography. This patient has a stabilized case of keratoconus. It is important to note that keratoconus advances only if there is some sort of stress to the cornea combined with the oxidative stress presented in this condition. Less than 5% of the individuals diagnosed with keratoconus will need a corneal transplant if they are properly fitted with good contact lenses.
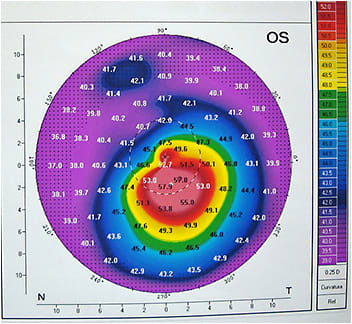
Figure 3. Anterior sagittal curvature using Pentacam (Oculus).
Scleral lenses are more forgiving with respect to the design; in many cases, it will not make a significant difference whether a scleral lens has 150 or 250 microns of corneal clearance. On the other hand, some mild-to-moderate complications may develop if some regions of the cornea present greater corneal clearance, especially when near the limbus.
On the other hand, specialty corneal GPs for keratoconus must be very well designed and perfectly finished to offer the best corneal contour while allowing only the lens periphery to land smoothly, with a well-rounded edge. This type of fitting may be time consuming, but it may be in the best interest of keratoconus patients. In our practice in Brazil, we always make corneal GPs our first choice. Although we are very passionate about sclerals lenses, we understand that they should be indicated only when corneal GPs fail to offer the best possible visual acuity and comfort, and especially to preserve the integrity of the overall corneal physiology.
Case Resolution
After complete healing of the corneal erosion, we refit the patient with a new lens in the proper lens parameters. The fluorescein pattern shows virtually no bearing on the corneal apex (Figure 4). The visual acuity also improved, as the patient had been wearing his previous lens for more than two years.
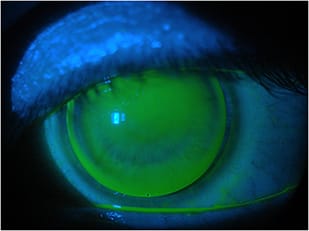
Figure 4. The updated fit with a new Ultracone (Ultralentes) design.
Conclusions
Most corneal complications with GP lens wear occur due to poorly designed lenses or improper fits—or both combined, which is the worst scenario. However, if patients, especially those who have keratoconus, are well fit, there is a tendency for them to postpone their regular follow-ups. This can also cause corneal complications.
It is important to instruct (and insist) that patients make regular visits, even if they feel fine. Even if patients are fit with well-designed lenses, there is still a possibility that lesions can develop over time. The force of the superior lid presses the lens against the eye with every blink. If a lens is too flat for that corneal apex, it will cause an erosion—it’s only a matter of time, depending on the extent of the bearing.
It is also imperative to note that patients wearing lenses with some sort of touch may have better quality vision compared to a non-touch lens. Patients may ask for their previous lens because of better vision, but this may lead to a recurrent erosion and eventually to a corneal scar.
Luciano Bastos is director & clinical instructor on Specialty Lenses at Instituto de Olhos Dr. Saul Bastos, Brazil.



