Nanophthalmos, or simple microphthalmos, is a rare, bilateral, sporadic, or autosomal dominant or recessive inheritance form of microphthalmos with the following clinical features: shorter axiallength, small cornea, shallow anterior chamber, marked iris convexity, normal or increased lens thickness, thickened sclera and choroid, and high lens/eye volume ratio (Duke-Elder and Cook,1964; Singh et al,1982; Brockhurst,1975). Due to the high lens/eye volume ratio, steep cornea, and high hyperopia, contact lens fitting is very challenging in a nanophthalmic eye.
CASE REPORT
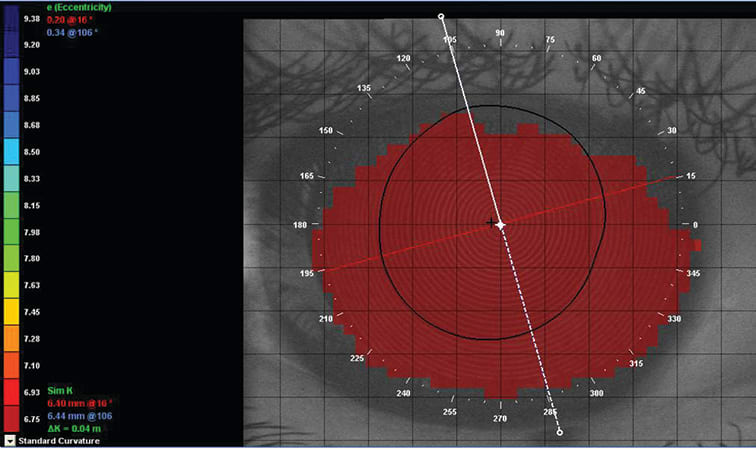
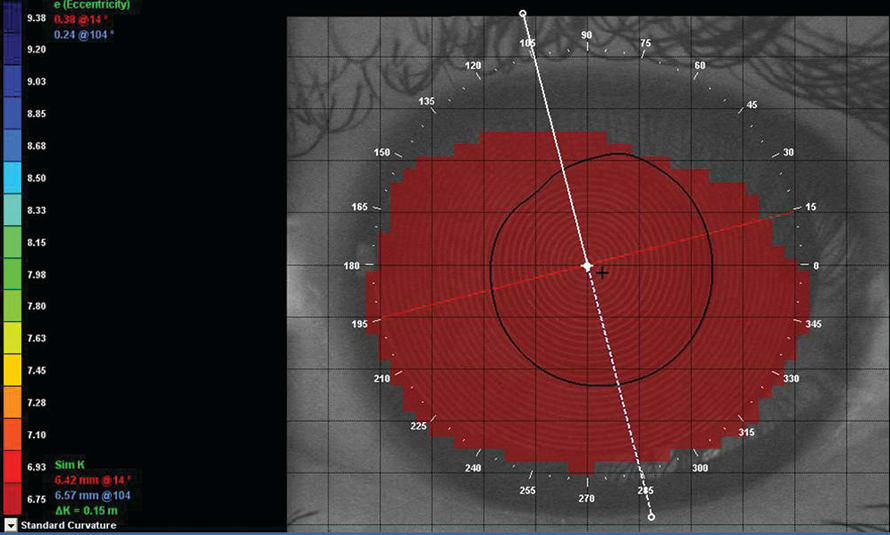
A 21-year-old female teacher presented with manifest refraction of +14.00 –0.75DC x 90 OD and OS. Best-corrected visual acuity was recorded as 20/80. For both eyes, axial length was 15.4mm, anterior chamber depth was 2.70mm, and intraocular pressure (IOP; Goldmann applanation tonometry) was 12 mmHg. Gonioscopy revealed a convex iris configuration in both eyes, and retinal examination showed hyperopic discs. Automated keratometry readings were 51.87 @ 104/52.62 @ 14 OD and 51.75 @ 94/52.25 @ 4 OS. Horizontal visible iris diameter was 10.5mm OD and OS, and vertical visible iris diameters were 9.5mm OD and 10mm OS. Palpebral fissure height was 10mm in both eyes. Simulated K readings were 52.73 (6.40mm) @ 16/52.40 (6.44mm) @ 106 OD and 52.57 (6.42mm) @ 14/51.36 (6.57mm) @ 104 OS (Figure 1).
According to the patient’s preferences, we first attempted to fit soft contact lenses, even though our previous clinical experience had been unsuccessful with this type of lens for a nanophthalmic eye. Specifically, previous issues had resulted from the unavailability of customized steeper base curve soft lenses. Therefore, we performed a GP lens trial.
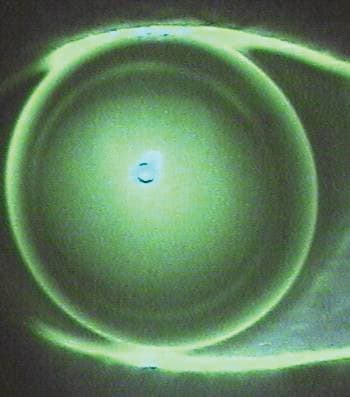
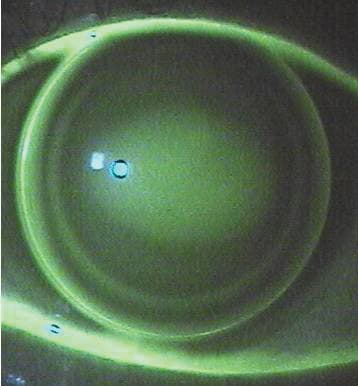
Our initial GP lenses were fit on-K with a small diameter (8.00mm) OD and OS. Ultimately, an optimal interpalpebral fit was achieved with a steep base curve and a small-diameter lenticular design. The final GP lenses had parameters of 6.2mm base curve, 8.0mm overall diameter (OAD), +16.50DS, and oxygen permeability (Dk) of 30 OD and OS. At lens dispensing, her best-corrected visual acuity with these GP lenses was 20/80 OD and OS. The lenses demonstrated adequate movement, with good pupillary coverage in both eyes. The right lens exhibited a diffuse fluorescein pattern with adequate edge clearance, and the left lens demonstrated slight central fluorescein pooling with adequate edge clearance (Figure 2). The patient is currently enjoying her vision with the GP lenses, without any complications.
DISCUSSION
GP lens performance can be influenced by lid characteristics, palpebral fissure height, corneal curvature, lens mass, lens thickness, lens diameter, lens edge-to-lid relationship, and lens material. Common philosophies used in GP fitting are “lid-attachment” and “interpalpebral” fitting. An interpalpebral fitting can be achieved by using GP lenses with a steep base curve and a small diameter (e.g., 8.2mm to 8.8mm) (Bennett and Sorbara, 2009). Upper lid forces, gravitational forces, and the lens-to-cornea relationship are three factors that usually determine lens centration. Compared to flatter lenses, steeper ones have greater centering forces. In the case of a high superior lid, an interpalpebral fit is more successful when a lid-attachment fit is not achievable. The center of gravity is located anteriorly with thick lenses, so they have a tendency to drop. With thinner lenses, however, the center of gravity is more posterior, so thin lenses center well.
To reduce the total lens mass in a plus lens, a GP lens with a lenticular design is recommended (Bennett and Sorbara, 2009). Although GP lenses are available in higher-Dk materials, lens thickness and diameter still play an important role in maintaining normal corneal physiology.
Considering all the factors, it was decided in this case to dispense GP lenses with a steeper base curve for better centration; a smaller diameter to achieve an interpalpebral fit; and a minus lenticular design to reduce lens mass and to minimize the risk of inferior decentration.
Customized soft and mini-scleral lenses can be successfully fit for a small eye in cases of GP intolerance. However, customized soft lens availability depends on the manufacturers, while mini-scleral lenses are more expensive than GP lenses.
In addition, nanophthalmic patients require regular follow up to monitor for any sort of development of angle closure glaucoma or an increase in IOP.





